The Real Struggle with Chronic Heartburn: Why Surgery Comes Into Play
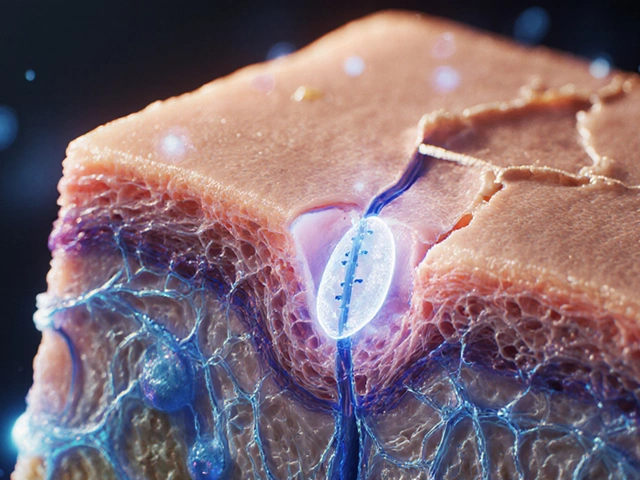
If you’ve ever felt that burning pressure in your chest after a meal, you’re not alone. Heartburn is ridiculously common—affecting about 20% of adults in the US. For most folks, an over-the-counter pill or a tweak in diet is enough to push back those fiery symptoms. But what if antacids, H2 blockers, or even that pricey prescription don’t bring real relief? That’s when things get serious. Doctors call it GERD—gastroesophageal reflux disease—when that burning sticks around week after week, creeping into your sleep and interrupting your days.
Chronic heartburn isn’t just uncomfortable. It can change your life. Eating out starts to feel like a risky game. You end up fearing coffee or pizza, and you view your bed as a battleground, stuck propped up by pillows like a mummy so you don’t wake up coughing acid. For some, GERD becomes more than a nuisance—it messes with relationships, disrupts work, and can lead to complications like ulcers, strictures, or even precancerous changes called Barrett’s esophagus. It’s no wonder that after trying piles of meds, many people look for a more definitive fix.
Around 30% of patients with severe GERD don’t get full relief from medications like Nexium (esomeprazole) or its cousins. If you’ve already studied all the alternatives to Nexium without luck, surgery might seem like the only path left. Sure, surgery sounds scary—but modern procedures are more effective (and less invasive) than you might think. Let’s break down the options.
Fundoplication: The Time-Tested Gold Standard
When you talk surgical heartburn fixes, fundoplication always comes up first. This old-school technique dates back to the 1950s, but it’s gotten a lot safer and slicker since then. The magic idea? Your stomach is somewhat wrapped around the lower part of your esophagus, like a scarf, so that the squishy tissue strengthens the weak valve that normally keeps acid from splashing up the wrong way.
There are flavors of this surgery, but Nissen fundoplication is the most famous—named after the Swiss surgeon who first perfected it. In most hospitals today, this procedure gets done using tiny “keyhole” incisions and a camera. You’re usually home in a day or two. During surgery, the surgeon gently frees up the top part of the stomach, brings it around the base of the esophagus, and stitches it together without squeezing things too tightly. Get the wrap right, and acid stays in the stomach where it belongs.
Here’s why fundoplication is still the go-to blueprint for serious GERD:
- Success rates are impressive—up to 90% of patients stop relying on daily acid meds.
- Improvement is often immediate; many wake up symptom-free.
- This isn’t experimental. Surgeons have refined the technique for decades.
- Complications are usually minor and temporary, like trouble burping or feeling full faster than before.
But it’s not just about fixing reflux. Many gain peace of mind knowing they’re less likely to develop Barrett’s esophagus down the road. If your reflux is stubborn or you’re worried about long-term complications, fundoplication really is the play you hear about most. Still, it isn’t for everyone. If you’ve got poor esophageal movement (peristalsis), or health conditions that make anesthesia risky, doctors might steer you elsewhere. Plus, there’s recovery—a few weeks where soft food is your best friend, and heavy lifting stays off the agenda.
Think of fundoplication like a reliable old pickup truck—it may not be trendy, but it just works if you need something that’ll last for years.
The LINX Device: Modern Tech Meets Acid Reflux
If fundoplication is the classic ride, then the LINX device is the shiny new car on the lot. LINX uses a tiny band of magnetic titanium beads—kind of like a flexible bracelet—that wraps around where the esophagus meets the stomach. The magnets are strong enough to snap closed and block acid, but gentle enough to open wide for food and drink.
This procedure exploded in popularity about a decade ago, thanks to studies showing that it worked for patients who didn’t want classic surgery. Instead of reshaping your stomach, your anatomy stays pretty much untouched—just a little gadget added to boost what nature forgot.
Here’s what sets the LINX device apart:
- Placed laparoscopically (with tiny incisions), often as a same-day procedure.
- Most folks go home the same day and start eating real food within days—not weeks.
- Preserves the ability to belch and vomit, which are sometimes tricky after fundoplication.
- If it doesn’t work or causes trouble, the device can usually be removed without much fuss.
The big question: does it work? According to long-term data, about 85% of people get significant relief from reflux and can ditch daily acid meds. In a five-year follow-up study, over 90% of patients were satisfied with their results. The LINX is FDA-approved and has helped more than 50,000 people worldwide so far.
Still, it’s not a one-size-fits-all fix. Metal allergies, large hiatal hernias, or advanced esophageal problems often rule you out. MRI scans aren’t advised with the device (unless you’ve got a newer MRI-safe version). Some people feel a little discomfort when swallowing big bites, especially in the first few weeks. But that usually fades as your body adapts.
The LINX device is especially appealing if you’re younger, fairly healthy, and want to avoid the downsides of traditional surgery. If you hate the thought of anatomical changes, this option feels less “invasive,” even though it’s still technically a surgery.

How Do You Know If You Need Surgery?
So, how do you know if it’s time to trade your pill bottle for a surgical fix? Not everyone with heartburn needs a procedure. Here’s what usually points doctors toward surgery:
- Acid reflux is stubborn—prescription medications and lifestyle changes just aren’t enough.
- Serious complications, like esophagitis (inflammation), strictures, chronic cough, asthma, or Barrett’s esophagus, show up in your medical records.
- You’re young and want to avoid a lifetime on pills.
- You experience side effects from long-term acid-blocker use—such as magnesium deficiency or risk of certain infections.
- Your reflux is so bad it triggers asthma attacks, sinus problems, recurring laryngitis, or sleeping issues.
Decision-making isn’t only clinical. Your personal goals matter too. Maybe travel plans or work hours make a daily pill complicated. Maybe you’re just tired of side effects or uncertainty. Surgeons don’t rush anyone into the OR. Before they schedule you, you’ll run through a battery of tests—think upper endoscopy, pH monitoring, manometry—that make sure surgery will actually help and not bring bigger headaches.
Timing is key: the best outcomes come when you’re healthy enough to tolerate surgery, but not so sick from GERD complications that recovery becomes a struggle. Be ready to ask questions about your own risks and goals. Real recovery takes time. If someone promises a magical overnight cure, run the other way.
What Happens Before, During, and After Surgery
Surgeons love to make it look easy on TV, but anyone heading into a fundoplication or LINX knows there’s plenty to prep. The process starts weeks ahead, usually with discussions about your full health history, blood work, and possibly tests for sleep apnea or lung issues. You’ll meet with the anesthesiologist and maybe even a nutritionist. Learning what food you can eat afterward (soups and soft stuff at first, then a gentle ramp-up to normal meals) saves a lot of discomfort—nobody wants to be caught guessing when they’re already groggy post-op.
If you’re having fundoplication, expect a few small belly incisions, usually above the belly button. Most folks spend one night in the hospital, and plenty are up and walking the same day. Swallowing feels weird at first, but that’s normal. You’ll be eating gentle foods within a day or so and can usually return to your usual life (but with a “no heavy lifting” clause) within two weeks.
LINX is a little quicker. Sometimes you’re in and out in an afternoon. You may have mild chest discomfort or trouble swallowing certain foods, but that almost always resolves over time. Eating regular meals (in smaller bites, with a little patience) helps your esophagus adjust. Surgeons want you to walk and move around right away—just no gym heroics until cleared.
Big tips for after surgery:
- Stick to your food plan and don’t rush into steak or crusty bread. Your esophagus will thank you.
- Small, frequent meals work way better than massive plates in those first weeks.
- Stay hydrated and take your pain meds as directed, but avoid narcotics if you don’t absolutely need them—they can slow down digestion.
- Call your surgeon if you can’t swallow water, develop a fever, or feel sudden severe pain.
- Plan for gradual improvement—most people get full strength and energy back over 2–4 weeks, not overnight.
Driving? You’re usually back behind the wheel in a week, once you don’t need strong painkillers. Returning to the office depends on your job, but desk work is often possible after a week or so for many people.
Weighing the Pros, Cons, and Long-Term Realities
Both fundoplication and the LINX device have impressive track records, but there isn’t a one-size-fits-all winner. Your lifestyle, symptoms, anatomy, and even your career can influence what’s best. Here’s a quick side-by-side table that sums up the basics:
| Procedure | Approach | Hospital Stay | Return to Normal Eating | Ability to Belch/Vomit | Effectiveness (% off meds) |
|---|---|---|---|---|---|
| Nissen Fundoplication | Laparoscopic | 1-2 days | 2-6 weeks | Sometimes reduced | Up to 90% |
| LINX Device | Laparoscopic | Same day | 1 week | Usually preserved | 85–90% |
Long-term studies show that about 1 in 5 patients need a tweak—an adjustment, removal, or additional meds—down the road. But for most, surgery brings a giant leap in quality of life. Acid reflux no longer runs the show. Weight gain or lifestyle changes still matter. Big meals or lying completely flat may trigger some burn, but way less than before. Plus, there’s no daily reminder to pop a pill.
An annoying truth: surgery doesn’t fix everything. If you crave spicy tacos at 11PM or ignore doctor’s orders, even the strongest surgical fix can be overwhelmed. Staying at a healthy weight, ditching late-night snacks, and skipping out on trigger foods will always help your odds. If your main concern is medication side effects or inconvenience, then weighing surgical solutions for heartburn against alternatives to Nexium is smart—each path has benefits and drawbacks.
Always ask your surgeon about their track record. Like any procedure, experience matters. Choose a center or doctor who does these operations frequently. The difference in outcomes between an experienced and a less-practiced surgeon can be significant.
No matter which solution you lean toward, just knowing you have choices is huge. That burning in your chest doesn’t need to run your life. With the right info and a team that listens, you can put acid reflux in its place—finally, and for good.





Kai Röder
July 17, 2025 AT 22:18This is a really thoughtful breakdown of surgical interventions for chronic heartburn, a condition that can seriously impact quality of life.
Understanding both fundoplication and the LINX device is key for anyone considering surgery after exhausting other treatments.
What stands out to me is the focus on patient selection and what to expect post-op, which is often overlooked in many resources.
I'd add that engaging with a gastroenterologist and a surgeon collaboratively can provide a more tailored treatment plan.
Also, lifestyle adjustments should continue even after surgery to maximize benefits.
Anyone here undergone these procedures? Curious about personal experiences.
Thanks for sharing this guide – it demystifies a complex topic nicely.
Nicholas Blackburn
July 19, 2025 AT 19:38Honestly, people act like surgery is some miracle fix. It’s not.
If you’re still dealing with heartburn after trying every diet tweak and OTC medicine, your problem might be more complicated than these procedures claim to fix.
Fundoplication has been around for a while, sure, but it’s not without risks and failures.
And that LINX device? Sounds like Silicon Valley tech babble more than real healing.
Before everyone rushes to cut and clamp, get real data on success rates and complications, because half the time these ‘solutions’ just swap one issue for another.
I’m skeptical about selling surgery as a panacea.
Seriously, read the fine print, people.
Dave Barnes
July 21, 2025 AT 17:38It's funny how the body’s internal mechanisms are so delicately balanced and yet we resort to surgical 'fixes' as if patching a leaky faucet.
Sure, the LINX device and fundoplication aim to restore normalcy, but what about the less visible psychological impacts of chronic heartburn?
Stress and anxiety often exacerbate digestive issues, making me wonder if a 'healing' process should be more holistic.
Though I’m no surgeon, I think a combo of mind and body approaches could be more effective long-term.
Still, for genuine anatomical issues, these procedures might be necessary—the question is always about the artful balance.
Anyone else see surgery as symbolic of our broader struggle against human frailty?
Brandi Thompson
July 24, 2025 AT 12:56Isn’t it absolutely maddening how many people just tolerate this constant burning sensation like it’s normal? Spoiler alert: It’s not.
The article glosses over the brutal reality of post-surgical symptoms that some patients just endure silently.
We need more transparency on the possible lifelong impacts, like difficulty swallowing or gas bloat syndrome after fundoplication.
Also, the LINX device isn’t exactly a walk in the park; foreign body sensations and device migration are real, scary complications.
People should not be spoon-fed sugarcoated facts; the dangers and downsides need spotlighting.
Otherwise, we end up with another generation signing up for surgery thinking it’s simple when it’s far from it.
So, don’t just listen to the hype. Demand the gritty details.
Emily Moody
July 26, 2025 AT 06:56This discussion wouldn’t be complete without spotlighting how these innovations place our nation at the forefront of medical progress.
Both fundoplication and the LINX system exemplify a fusion of high-tech progressivism and surgical adeptness that can dramatically alleviate chronic heartburn’s grip on millions.
We must champion these homegrown advances and resist any defeatist rhetoric that undermines their potential.
True, no medical intervention is flawless, but embracing these tools asserts our commitment to superior healthcare solutions.
Moreover, educating the public on when and how to pursue these options ensures we safeguard collective health with informed decisiveness.
So let’s recognize the bold strides in surgical treatment, leaving behind outdated skepticism and fully appreciating these life-changing options.
Prateek Kohli
July 28, 2025 AT 01:10I appreciate how this post lays out the options clearly and calmly 😊.
Living in a region where sometimes access to surgical options is limited, having well-informed insights helps patients weigh their decisions safely.
The LINX device seems nifty, but I wonder about long-term maintenance and monitoring, especially for those far from specialized centers.
Also, the psychological toll of chronic heartburn is real — it’s disruptive beyond just physical pain.
It’s vital that post-surgical care includes support systems addressing mental and emotional wellness too.
I've read that lifestyle changes combined with surgery yield the best outcomes, so a multidisciplinary approach is essential.
Does anyone here have thoughts on the coordination of surgical and psychological care?
Noah Seidman
July 29, 2025 AT 19:10Yeah, because nothing says progress like implanting a ring around your esophagus. Brilliant.
Look, chronic heartburn is often a symptom, not a disease unto itself.
Rushing to fix symptoms surgically without understanding the underlying causes is just another example of medical hubris.
Plus, the whole idea that these procedures fix everyone is naive at best.
Maybe instead of celebrating these gadgets, we should focus more on prevention and addressing lifestyle factors first.
Otherwise, we end up reinforcing a quick-fix culture that ignores root causes.
Anyone else feel this medical commodification is a bit unsettling?
Anastasia Petryankina
July 31, 2025 AT 13:10Oh wonderful, more invasive procedures touted as the panacea for heartburn sufferers everywhere.
Because we really need more silicone rings and surgical wraps crowding the market, right?
Honestly, anyone with half a brain should be wary of buying into the LINX hype without scrutinizing the quality of evidence.
There’s always the risk of turning complications into trendy business opportunities for medical device companies.
But hey, if you enjoy feeling like a walking science experiment, by all means, take the plunge.
Meanwhile, I’ll stick to tried-and-true non-invasive therapies and critical thinking.
Just saying.
Tim Ferguson
August 2, 2025 AT 09:56While I respect the surgical options discussed, I wonder about the nuance in patient experiences after these procedures.
It's tempting to view surgery as a definitive answer, yet I’ve seen plenty who find mixed results.
Ultimately, it seems these solutions are not one-size-fits-all but part of a broader spectrum of care.
Perhaps emphasizing patient education on both risks and realistic expectations could bridge the gap.
I also ponder if cultural factors influence acceptance or skepticism toward these procedures.
Anyway, it’s clear the journey to relief requires critical thinking and openness to multiple paths.
Noah Cokelaere
August 4, 2025 AT 06:43This article’s a solid primer! Gotta love how it breaks down complex surgical options into digestible info.
Still, I’m curious about real-world outcomes beyond clinical trials — like patient satisfaction long-term.
Also, any tips on what questions to ask your surgeon before committing?
From experience, knowing recovery timelines and lifestyle impacts is crucial for managing expectations.
Does anyone have personal stories about adjustment periods post-fundoplication or LINX implantation?
And how do you balance hope with realism when considering these choices?
Appreciate the thoughtful conversation here!
Chip Hutchison
August 16, 2025 AT 22:16Thanks all for the insightful perspectives — it’s clear this topic sparks diverse views.
As someone who’s researched both procedures extensively, I want to emphasize the importance of shared decision-making between patient and provider.
Every case is unique, and surgery should be considered after careful evaluation of risks and benefits.
Moreover, multidisciplinary support including nutritionists and mental health professionals can enhance outcomes.
I encourage anyone confronted with chronic heartburn to seek multiple opinions and explore all options before deciding.
Feel free to ask me if you want details on recovery processes or lifestyle adaptations post-surgery.
It’s about empowering you with knowledge for the best path forward.