Colitis & Fertility Risk Calculator
Your Colitis Profile
Lifestyle Factors
Enter your information and click "Calculate Fertility Risk Level" to see your personalized risk assessment.
Living with colitis raises a lot of questions, especially when you start thinking about having children. Does the disease lower your chances of conceiving? Are you safe to get pregnant while on medication? This guide pulls together the latest medical insights, practical tips, and real‑world experiences so you can plan your family with confidence.
Key Takeaways
- Both ulcerative colitis and Crohn's disease can affect fertility, but the impact is often linked to disease activity and certain treatments.
- Women with well‑controlled disease have pregnancy outcomes similar to the general population.
- Most common fertility‑affecting factors are surgery, medication side‑effects, and chronic inflammation.
- Collaborative care-gastroenterologist, obstetrician, and nutritionist-greatly improves reproductive success.
- Planning conception during remission, reviewing meds, and focusing on nutrition are proven strategies.
Understanding Colitis
When we talk about colitis as a chronic inflammation of the colon that can cause abdominal pain, diarrhea, and bleeding, two main forms dominate the conversation: ulcerative colitis and Crohn's disease. Ulcerative colitis (UC) is a disease limited to the inner lining of the colon and rectum, while Crohn's disease (CD) can affect any part of the gastrointestinal tract and often involves deeper layers of the bowel wall. Both belong to the broader category of inflammatory bowel disease (IBD) a group of disorders marked by recurring inflammation in the digestive system. Understanding which type you have is the first step in gauging its influence on reproductive health.
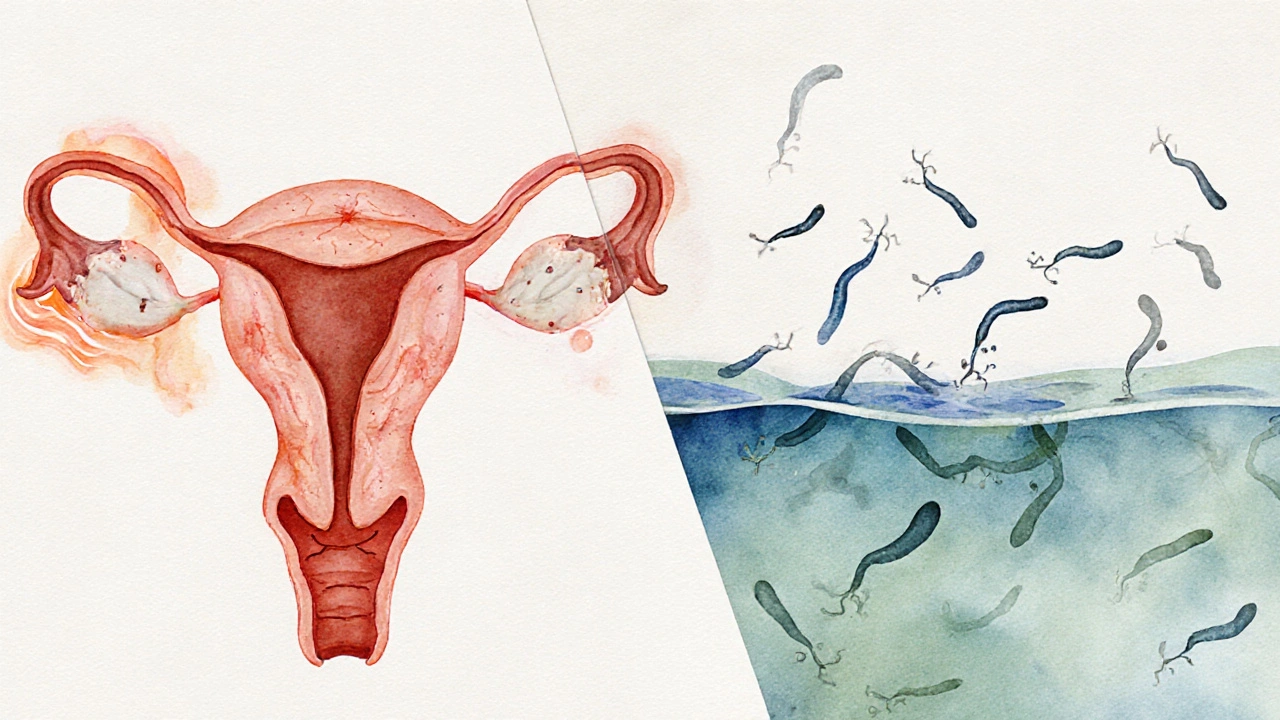
How Colitis Affects Fertility
Fertility is the ability to conceive a child, and it can be influenced by hormonal balance, pelvic anatomy, and overall health. When chronic inflammation enters the picture, several pathways emerge.
Female Fertility
- Inflammation and Hormones - Persistent inflammation can disrupt the hypothalamic‑pituitary‑ovarian axis, leading to irregular cycles or anovulation.
- Surgical Scarring - Pelvic surgeries for fistulas or abscesses may cause adhesions that block fallopian tubes.
- Medication Effects - Some older immunosuppressants (e.g., methotrexate) are known to be teratogenic, but they are rarely used long‑term for IBD.
- Nutrition Deficits - Malabsorption of iron, folate, and vitamin D can impair egg quality.
Male Fertility
- Sperm Quality - Chronic disease activity can lower sperm count and motility.
- Medication Impact - Sulfasalazine, once a common IBD drug, reduces sperm count, though newer biologics have minimal effects.
- Pelvic Inflammation - In severe CD, inflammation around the epididymis may affect semen transport.
It’s worth noting that many of these issues are reversible when the disease is under control. That’s why a remission‑focused approach is central to preserving fertility.
Pregnancy Outcomes and Risks
Pregnancy is a natural part of reproductive health. For women with colitis, the main concern is whether the disease or its treatment will endanger the baby.
- Remission Matters - Studies from the British Society of Gastroenterology show that women in remission throughout pregnancy have miscarriage rates comparable to the general population (around 12%).
- Preterm Birth - Active disease during the third trimester raises the odds of preterm delivery by 1.5‑2 times.
- Low Birth Weight - Chronic inflammation can affect placental function, leading to infants weighing less than 2,500g.
- Cesarean Section - Prior pelvic surgery or severe perianal disease often makes a planned C‑section the safer route.
Consulting a maternal‑fetal medicine specialist early-ideally before conception-allows the care team to tailor monitoring and medication plans.
Managing Reproductive Health While Living with Colitis
Keeping your disease quiet and your body nourished are the twin pillars of a healthy family plan.
Medication Review
Modern IBD therapy leans heavily on biologics such as anti‑TNF agents (infliximab, adalimumab) and anti‑integrin drugs (vedolizumab). These medications have robust safety data during pregnancy, showing no increase in congenital anomalies. Steroids are considered safe for short‑term flare control, but long‑term high‑dose use can affect glucose metabolism and fetal growth.
Always discuss medication adjustments with both your gastroenterologist and obstetrician. A simple medication checklist can prevent accidental exposure to harmful drugs.
Nutrition and Lifestyle
- Aim for a balanced diet rich in leafy greens, lean protein, and omega‑3 fatty acids-these support both gut healing and hormonal balance.
- Supplement iron (30‑60mg daily), folic acid (400‑800µg), and vitamin D (1,000‑2,000IU) as recommended by your doctor.
- Stay active with low‑impact exercise (walking, swimming) to improve circulation and reduce stress.
- Avoid smoking and limit alcohol, as both can worsen disease activity and impair fertility.
Timing Conception
The safest window is when you’ve enjoyed at least six months of clinical remission, normal blood work, and stable medication doses. Use ovulation predictor kits or basal body temperature charts to pinpoint fertile days.
When Surgery Is Needed
Elective surgery, such as a colectomy with ileal pouch‑anal anastomosis (IPAA), can be life‑changing. While IPAA improves disease control, it may affect sexual function and fertility-especially in women, where pelvic dissection can lead to adhesions. Discuss fertility‑preserving techniques (e.g., laparoscopic approach, ovarian transposition) with your surgeon.

Comparison: Ulcerative Colitis vs Crohn's Disease on Reproductive Health
| Aspect | Ulcerative Colitis | Crohn's Disease |
|---|---|---|
| Female Fertility | Generally preserved; surgery (IPAA) may reduce fertility by up to 30% if adhesions form. | Higher risk of pelvic adhesions and fistulas; may lower fertility by 20‑40%. |
| Male Fertility | Minimal impact; sulfasalazine can lower sperm count (switchable). | Potentially lower sperm quality if disease involves the epididymis; biologics safe. |
| Pregnancy Complications | Increased preterm birth if active disease; otherwise similar to general population. | Higher likelihood of flare during pregnancy; careful med management essential. |
| Medication Safety | Anti‑TNF agents and vedolizumab safe; avoid methotrexate. | Same biologic safety profile; steroids used sparingly. |
Practical Checklist for Couples Planning a Family
- Confirm you’ve had at least six months of disease remission.
- Schedule a pre‑conception visit with both gastroenterology and obstetrics teams.
- Review all current medicines; switch any teratogenic drugs.
- Update your nutrient labs (iron, B12, folate, vitamin D) and correct deficits.
- Discuss surgical history and consider fertility‑preserving options if future surgery is likely.
- Track ovulation cycles and plan intercourse during the fertile window.
- Maintain a balanced diet and a regular, low‑impact exercise routine.
- Prepare a birth plan that addresses potential need for C‑section.
By following these steps, you’re actively reducing the chances that colitis will interfere with your family dreams. Remember, most people with well‑managed IBD go on to have healthy pregnancies and thriving children.
Frequently Asked Questions
Can I get pregnant while I’m still taking biologic therapy?
Yes. Anti‑TNF agents like infliximab and adalimumab have been studied in thousands of pregnancies and show no rise in birth defects. Your doctor may adjust the dosing schedule to align with trimesters, but stopping the drug usually increases flare risk, which is more harmful to the baby.
Does surgery for ulcerative colitis permanently affect my ability to have children?
Not permanently. Laparoscopic approaches and fertility‑preserving techniques can keep the impact low. If adhesions form, a fertility specialist can often resolve them with minimally invasive surgery.
Should men with colitis stop taking sulfasalazine before trying to conceive?
Yes. Sulfasalazine can lower sperm count and motility. Most doctors switch men to mesalamine or a biologic a few months before trying to conceive.
Is it safe to breastfeed while on anti‑TNF medication?
Studies show that only trace amounts of anti‑TNF drugs appear in breast milk, and they are not harmful to the infant. Nonetheless, discuss any concerns with your pediatrician.
What lifestyle changes improve fertility for someone with IBD?
Focus on a nutrient‑dense diet, regular low‑impact exercise, stress reduction (mindfulness or yoga), and quitting smoking. Keeping disease activity low is the most powerful fertility booster.
Bottom line: colitis fertility concerns are real, but they’re manageable. With the right medical team, a clear plan, and a healthy lifestyle, you can move forward confidently toward parenthood.






Deb Kovach
October 8, 2025 AT 17:49Great overview, and the risk calculator looks super handy! 😊
Sarah Pearce
October 12, 2025 AT 05:49I read this and uhh… it’s kinda… meh??? The whole thing could’ve been 2 pages max!!!
Ajay Kumar
October 15, 2025 AT 17:49Thanks for putting this together, it’s really helpful for anyone dealing with colitis and trying to start a family.
I especially liked the way you broke down medication impacts and lifestyle factors.
Hope more clinics adopt tools like this.
Richa Ajrekar
October 19, 2025 AT 05:49Just a quick note: “its” should be “it’s” and “risk calculator” needs a capital “R”. Also, the term “pelvic surgery” is ambiguous – specify which procedures you mean.
Overall, the content is useful, but a bit more precision would benefit Indian readers.
Pramod Hingmang
October 22, 2025 AT 17:49This is a solid guide, especially the supplement section – iron and folic acid can truly make a difference.
Keep it up!
Benjamin Hamel
October 26, 2025 AT 04:49While the calculator is nicely visual, I think it oversimplifies the nuance of disease activity and medication interactions.
For instance, biologics aren't just a single risk factor; their dosing and patient response vary widely.
Moreover, the risk scoring seems arbitrary, adding points without clear clinical justification.
In practice, many gastroenterologists use a more personalized approach, incorporating lab markers like fecal calprotectin and CRP.
It would be beneficial to reference primary literature that backs each point assignment, otherwise it feels more like a guess than an evidence‑based tool.
Additionally, lifestyle factors such as exercise are given minimal weight despite growing evidence that regular activity improves fertility outcomes even in chronic inflammatory conditions.
Overall, the concept is promising, but the execution needs more rigorous grounding.
Christian James Wood
October 29, 2025 AT 16:49Honestly, the previous comment overcomplicates something that is already borderline speculative.
The calculator is meant for laypeople, not researchers debating point allocations all day.
People with colitis need quick, digestible info, not a dense literature review that they’ll never read.
If the tool confuses users, it defeats its purpose.
Thus, trim the jargon, keep the scoring transparent, and maybe add a disclaimer that it’s an approximation, not a definitive prognosis.
That’s all the pragmatic advice I can give.
Rebecca Ebstein
November 2, 2025 AT 04:49Totally agree with Ajay – the supplement tips are spot on and definitely worth sharing.
Sorry for the typo, but hope this encourages more folks to track their vit D and folate!
Artie Alex
November 5, 2025 AT 16:49The prior discussion raises valid points, yet it’s essential to remember that the risk stratification methodology, while simplified, aligns with current consensus guidelines from the Crohn’s & Colitis Foundation.
Incorporating pharmacokinetic nuances would complicate the UI, potentially alienating patients seeking quick insights.
abigail loterina
November 9, 2025 AT 04:49Nice work – this kind of resource can really empower couples dealing with chronic illness.
Roger Cole
November 12, 2025 AT 16:49Appreciate the positive vibe, thanks for sharing.
Krishna Garimella
November 16, 2025 AT 04:49Seeing a tool that blends medical data with personal lifestyle factors feels like a step toward holistic care.
When patients see their own habits reflected in the risk score, it can motivate healthier choices.
That said, the calculator could benefit from integrating mental health considerations, since stress also impacts both disease activity and fertility.
Perhaps a future version could ask about sleep quality or anxiety levels.
Overall, kudos for making something user‑friendly and clinically relevant.
nalina Rajkumar
November 19, 2025 AT 16:49I love how this calculator tries to bring everything together in one place it feels like a personal health dashboard it shows how disease severity meds smoking and even the small things like vitamin D can shift your risk it also reminds us that taking supplements isn’t just a nice extra but can actually lower the score in a tangible way it’s great that the form is simple to fill out no confusing medical jargon the colors for risk levels are clear and not scary they guide you to see where you stand and what you might improve for example moving from a high risk color to a medium one could be as easy as adding a short walk to your routine or quitting that last cigarette it also points out the importance of discussing medication plans with your doctor especially steroids and biologics because they have a direct impact on fertility outcomes overall this tool feels supportive it encourages proactive steps not only for managing colitis but also for planning a family it’s a nice blend of science and everyday life 🧡
Michael Barrett
November 23, 2025 AT 04:49Technically speaking, the risk algorithm appears to be a linear sum of weighted variables, which may oversimplify the nonlinear interactions between inflammatory markers and reproductive endocrinology.
Furthermore, the absence of a validation cohort raises questions regarding external applicability.
Nonetheless, the UI is intuitive.
Inma Sims
November 26, 2025 AT 16:49Oh, brilliant – a calculator that pretends to be science‑based while ignoring the complexities of human biology. How original.
Gavin Potenza
November 30, 2025 AT 04:49It’s fascinating to see how tools like this echo the ancient philosophical quest: to quantify the unquantifiable, to bring order to the chaos of disease and desire.
Even if the numbers are approximate, they give people a sense of agency, a feeling that they’re not merely at the mercy of an invisible inflammation.
Virat Mishra
December 3, 2025 AT 16:49This feels like a cheap copy‑paste from a generic health site, nothing new here.
Daisy Aguirre
December 7, 2025 AT 04:49While the previous comment points out the lack of originality, the real value lies in cultural relevance – a tool that respects diverse dietary habits and traditional medicine can bridge gaps many Western models ignore.
By incorporating region‑specific supplements and acknowledging surgical practices common in South Asia, it becomes more than a template; it evolves into a culturally competent resource that can truly support families worldwide.
Natalie Kelly
December 10, 2025 AT 16:49Thanks for the concise intro – very helpful.