When a generic drug company wants to prove their version of a medicine works just like the brand-name version, they don’t just guess. They run a crossover trial design. This isn’t just a common method-it’s the gold standard for bioequivalence studies. And for good reason. It cuts down the number of people needed, reduces noise from individual differences, and gives regulators like the FDA and EMA clear, reliable data. But it’s not simple. Get one step wrong-like a washout period that’s too short-and the whole study can fail.
Why Crossover Designs Rule Bioequivalence
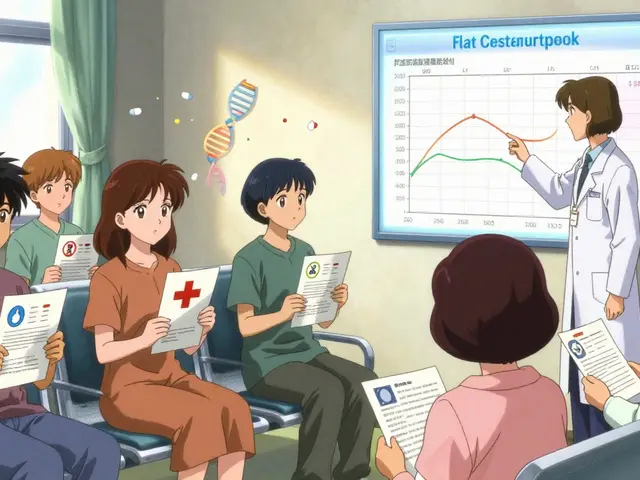
Imagine testing two painkillers. In a parallel study, one group gets Drug A, another gets Drug B. But people vary so much-age, metabolism, body weight-that even if both drugs work equally well, the results might look different just because of who was in each group. That’s noise. Crossover designs fix this by having each person take both drugs, one after the other. Now, you’re comparing how the same person responds to each drug. Their unique biology cancels out. That’s the power. This isn’t theory. In practice, a crossover design can cut the number of participants needed by up to 80% compared to a parallel design. For a drug with moderate variability, you might need just 24 people instead of 72. That saves time, money, and reduces burden on volunteers. The FDA and EMA both say this design is preferred for most bioequivalence studies. In fact, 89% of generic drug approvals in the U.S. between 2022 and 2023 used crossover designs.The Standard 2×2 Crossover: AB/BA
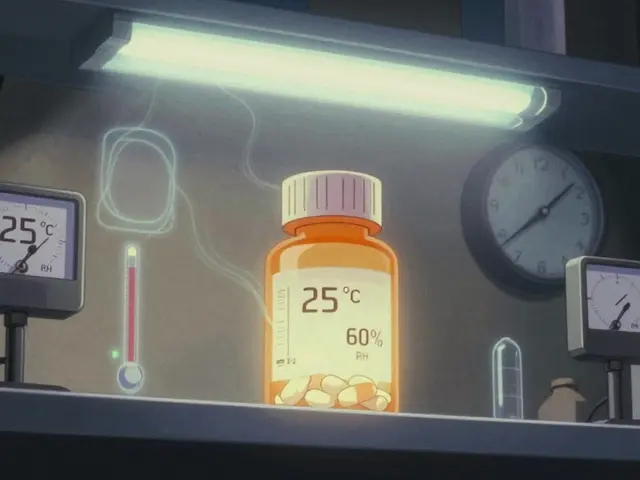
The most common setup is called the 2×2 crossover. That means two treatment periods and two sequences. Half the participants get the test drug first, then the reference (brand) drug after a break. The other half get the reference first, then the test. It’s labeled AB/BA-A is test, B is reference. Between the two doses, there’s a washout period. This isn’t just a rest day. It’s a mandatory pause-usually at least five half-lives of the drug-so the first dose is completely cleared from the body. If any of the first drug is still hanging around when the second starts, it skews the results. That’s called a carryover effect, and it’s the #1 reason studies get rejected. For example, if a drug’s half-life is 4 hours, the washout needs to be at least 20 hours. But for drugs like warfarin, which has a half-life of 36-42 hours, that’s 7-9 days. Studies have to prove this washout works. That means taking blood samples before the second dose to confirm drug levels are below the detection limit.What Happens When the Drug Is Too Variable?
Not all drugs behave the same. Some have high intra-subject variability-meaning the same person’s response changes a lot from one dose to the next. If the coefficient of variation (CV) is above 30%, the standard 2×2 design struggles. Why? Because the confidence interval for bioequivalence might not fit within the 80-125% range, even if the drugs are truly equivalent. That’s where replicate designs come in. These use four treatment periods. There are two types:- Partial replicate (TRR/RTR): The test drug is given twice, and the reference once. One sequence gets T-R-R, the other gets R-T-R.
- Full replicate (TRTR/RTRT): Both drugs are given twice. One sequence is T-R-T-R, the other is R-T-R-T.

Statistical Analysis: What Happens Behind the Scenes
The raw data from a crossover study looks simple: blood samples at set times, measuring drug concentration. But the analysis? It’s complex. You can’t just average the numbers. You have to account for three things:- Sequence effect: Did the order of drugs matter? (e.g., did people respond differently because they got the test drug first?)
- Period effect: Did time itself affect results? (e.g., were people more stressed or tired in the second period?)
- Treatment effect: Is there a real difference between the two drugs?
Real-World Wins and Failures
One company saved $287,000 and eight weeks by using a 2×2 crossover for a generic warfarin study. With an intra-subject CV of 18%, they needed only 24 subjects. A parallel design would have needed 72. But another team lost $195,000 and months of work. They tested a highly variable drug with a 42% CV using a 2×2 design. They assumed a 10-day washout was enough. It wasn’t. Residual drug was still detectable in period two. The study failed. They had to restart with a four-period replicate design. These aren’t rare mistakes. In 2018, 15% of major FDA deficiencies in bioequivalence submissions were due to inadequate washout periods. It’s not that people don’t know the rules. It’s that they underestimate how long it takes for some drugs to fully clear.
When Crossover Doesn’t Work
Crossover designs are powerful, but they’re not universal. If a drug has a half-life longer than two weeks, you can’t wait five half-lives. That’s six months or more. No volunteer will stay in a study that long. In those cases, parallel designs are the only option. Also, if the drug causes permanent changes-like a vaccine or a drug that alters immune function-crossover is out. You can’t give someone a second dose if the first one changed their biology permanently. And for narrow therapeutic index drugs-where even small differences can cause toxicity or ineffectiveness-regulators are now approving 3-period replicate designs (TTR/RRT/TRR) to get even tighter control over variability.What’s Next for Crossover Trials?
The future is getting smarter. Adaptive designs are on the rise. These let researchers pause halfway through the study, look at the data, and adjust the sample size if needed. In 2022, 23% of FDA submissions included adaptive elements-up from 8% in 2018. The EMA’s 2024 update will likely make full replicate designs the default for all highly variable drugs. And while digital health tools-like wearable sensors that track drug levels continuously-could one day reduce the need for washout periods, they’re not ready yet. For now, crossover designs remain the backbone of bioequivalence testing. They’re efficient, precise, and trusted. But only if they’re done right. Every washout must be validated. Every sequence must be randomized. Every model must be checked for carryover. Skip any of that, and the data doesn’t just look bad-it’s invalid.What is the main advantage of a crossover design in bioequivalence studies?
The main advantage is that each participant acts as their own control. By receiving both the test and reference drug, individual differences in metabolism, age, or genetics are eliminated from the comparison. This reduces variability and allows researchers to detect true differences with far fewer participants-often six times fewer-than in a parallel-group study.
Why is the washout period so important in a crossover trial?
The washout period ensures that the first drug is completely cleared from the body before the second drug is given. If any residue remains, it can interfere with the measurement of the second drug’s effects-a phenomenon called carryover. This can make it look like the drugs are different when they’re not, or mask a real difference. Regulatory agencies require washout periods to be at least five half-lives of the drug, and this must be proven with pharmacokinetic data.
When should a replicate crossover design be used instead of a 2×2 design?
A replicate design (TRR/RTR or TRTR/RTRT) should be used when the drug has high intra-subject variability-typically when the coefficient of variation (CV) exceeds 30%. Standard 2×2 designs can’t reliably estimate within-subject variability, making it hard to prove bioequivalence. Replicate designs allow regulators to use reference-scaled average bioequivalence (RSABE), which adjusts the acceptance range based on the drug’s natural variability, making approval possible without needing hundreds of participants.
What are the most common reasons bioequivalence studies using crossover designs get rejected?
The top reasons are inadequate washout periods leading to carryover effects, failure to properly test for sequence or period effects in statistical models, and improper handling of missing data. Studies that don’t validate washout with pharmacokinetic data or use incorrect statistical methods (like ignoring random effects) are frequently flagged by regulators. About 15% of major deficiencies in 2018 submissions were due to washout issues alone.
Can crossover designs be used for all types of drugs?
No. Crossover designs are unsuitable for drugs with very long half-lives (over two weeks), where the washout period would be impractical. They’re also not used for drugs that cause permanent changes in the body, like vaccines or immunomodulators. In these cases, parallel-group designs are required. Additionally, for narrow therapeutic index drugs, regulators now prefer more complex replicate designs to ensure safety and precision.





Lisa Detanna
November 22, 2025 AT 18:57Man, I remember when my cousin’s company ran a bioequivalence study and they totally blew the washout on a warfarin generic. Thought 7 days was enough because ‘it’s just blood thinning stuff.’ Nope. FDA came back with a rejection letter thicker than a textbook. They had to restart with a full replicate design and lost like $200K. Never underestimate half-lives.
Also, the part about RSABE for high-variability drugs? So glad regulators finally get it. Some of these generics are for epilepsy or anticoagulants - you can’t treat them like ibuprofen.
And honestly? The fact that 89% of U.S. approvals use crossover designs says everything. Efficiency isn’t just nice - it’s ethical. Fewer volunteers, less waste, better science.
Demi-Louise Brown
November 23, 2025 AT 16:02Crossover designs reduce inter-subject variability by design. This is not merely statistical convenience - it is scientific integrity. Each subject serves as their own control. The reduction in sample size is not a cost-saving trick; it is a validation of precision.
Washout periods must be pharmacokinetically validated. Failure to do so invalidates the entire study. Regulatory agencies do not tolerate assumptions. Data must speak - clearly, cleanly, and without carryover noise.
Suresh Ramaiyan
November 23, 2025 AT 17:06Interesting how the math behind this mirrors life sometimes. We all think we’re seeing the world clearly - but we’re just comparing our own experience to someone else’s. A crossover design? It’s like forcing yourself to walk in both shoes before judging which one fits better.
And the washout? That’s the quiet pause we all need before reacting to the next thing. Too often we rush into the next dose - of opinion, of action - without letting the last one fully clear. The science here is beautiful because it’s human.
Also, replicate designs for high-variability drugs? That’s not just statistics. That’s humility. Admitting that some things just don’t behave predictably - and designing around that instead of forcing a square peg into a round hole.
Katy Bell
November 24, 2025 AT 10:51Okay but can we talk about how wild it is that people still mess up washout periods?? Like, the half-life is NOT a suggestion. It’s a biological deadline. And yet, I’ve heard of labs just ‘guessing’ based on what worked last time.
Also, I love that they’re using adaptive designs now. It’s like the study has a brain. ‘Hmm, we’re not getting enough data? Let’s add more people.’ That’s next-level smart. Also, I’m lowkey obsessed with wearable sensors that could one day replace blood draws. Imagine testing a drug and your Apple Watch just tells you the concentration. No needles. No waiting. Just vibes.
Also also - why is no one talking about how much this saves volunteers? People don’t realize how grueling these trials are. 24 people instead of 72? That’s like turning a month-long prison sentence into a weekend retreat.
Ragini Sharma
November 25, 2025 AT 01:36so like… if the drug has a 42hr half life, washout is 7-9 days? yeah ok but who the heck stays in a clinic that long?? like i get the science but also… is anyone even gonna sign up for that??
also why do they use SAS?? why not python?? just asking for a friend who got roasted by their boss for suggesting R
and i swear every time i see ‘reference scaled average bioequivalence’ i think it’s a new type of yoga. RSABE: Rest, Stretch, Align, Breathe, Euphoria.
Linda Rosie
November 25, 2025 AT 16:16Washout must be validated. Carryover invalidates results. Replicate designs are necessary for high variability. Statistical models must account for sequence and period. Regulatory standards are clear. Compliance is non-negotiable.
Vivian C Martinez
November 27, 2025 AT 04:48This is one of those topics where the science is so elegant it almost feels unfair. You take the biggest source of noise - human variation - and you make each person their own control. It’s like magic, but with statistics.
And the fact that we’re moving toward adaptive designs? That’s the future. Not just doing things right, but learning while you do them. It’s not just about getting approval - it’s about getting better every time.
Also, props to the teams who caught their own washout errors before submission. That takes guts. Most would’ve just pushed through. Kudos to the ones who paused, checked, and fixed it.
Ross Ruprecht
November 27, 2025 AT 12:17So… this whole post is just a 10-page manual on how to not screw up drug tests? I get it. Washout. Stats. Replicates. But can we just make one drug that works the same for everyone and call it a day? Why does everything have to be this complicated?
Also, who has time to read all this? I just want my generic pill to not kill me.