Why Medications for Alcohol Use Disorder Can Sometimes Make Relapse More Likely
People with Alcohol Use Disorder (AUD) often turn to medication hoping it will finally help them stay sober. But here’s the uncomfortable truth: taking these drugs without the right support, timing, or understanding can actually increase your chance of relapse.
Three FDA-approved medications - acamprosate, naltrexone, and disulfiram - are meant to reduce cravings and prevent drinking. But they’re not magic pills. They work best when used with counseling, structure, and commitment. Skip those pieces, and the meds can backfire.
How Each Medication Works - and Where It Can Go Wrong
Acamprosate (brand name Campral) helps stabilize brain chemistry after you stop drinking. It doesn’t block alcohol or make you sick. Instead, it tries to calm the nervous system after withdrawal. But here’s the catch: you have to be completely sober for at least 3 to 5 days before starting it. If you take it while still drinking, or if you slip and drink while on it, your brain doesn’t get the benefit. Worse, some people feel discouraged when they realize it doesn’t stop them from wanting a drink - it just makes the discomfort after quitting easier. That can lead to quitting the med too soon.
Naltrexone (Revia or Vivitrol) works differently. It blocks the pleasurable effects of alcohol. If you drink while on naltrexone, you won’t feel the usual high. That sounds good - until you realize it doesn’t stop you from drinking at all. Some people think, “I can still have a few drinks, I just won’t enjoy them.” That mindset is dangerous. It turns the medication into a permission slip to drink lightly, which often leads back to heavy use. Studies show naltrexone reduces heavy drinking days, but not total abstinence. If your goal is complete sobriety, and you’re not ready to fully commit, naltrexone might give you a false sense of control.
Disulfiram (Antabuse) is the oldest and most extreme option. It makes you violently ill if you drink alcohol - flushing, nausea, vomiting, even heart problems. It sounds like a deterrent, and for some, it is. But it only works if you take it every day and avoid alcohol completely. If you miss a dose, or think you can “outsmart” it by drinking after the drug wears off, you’re playing Russian roulette. Many people stop taking it because the side effects - metallic taste, drowsiness, anxiety - are constant, even when sober. And if you do drink while on disulfiram, the reaction can be life-threatening. For many, the fear of this reaction becomes so overwhelming that they quit the med entirely… and then drink again.
The Hidden Problem: Timing and Preparation
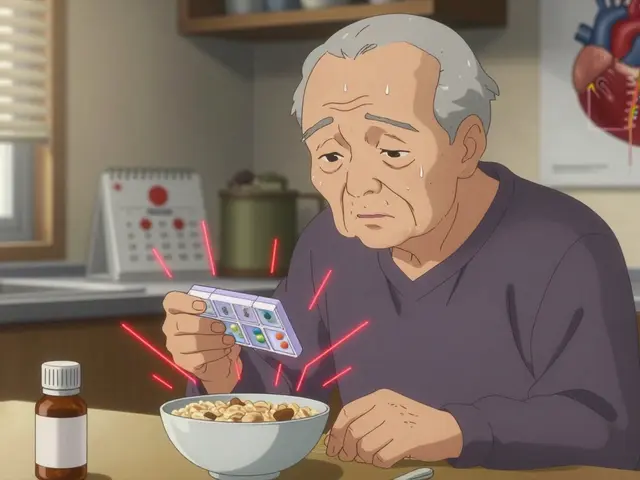
One of the biggest reasons medications fail is because they’re started too early or without proper support. You can’t just walk into a doctor’s office, get a prescription, and expect to be cured.
Acamprosate requires a clean break from alcohol before it can help. If you’re still drinking daily and suddenly stop cold turkey, your brain is in chaos. Starting acamprosate during this unstable period won’t fix the underlying damage - it just adds another layer of stress. Many patients quit because they don’t feel better right away and assume the drug isn’t working.
Naltrexone needs a 7- to 10-day washout period if you’ve been on opioids. But many people with AUD also use painkillers or other substances. If they don’t disclose this, or if their doctor doesn’t ask, they risk serious withdrawal symptoms or even overdose when starting naltrexone.
Disulfiram? It’s often prescribed without a full discussion of what happens if you drink. Patients aren’t told that even a sip of mouthwash, cough syrup, or perfume with alcohol can trigger a reaction. That kind of ignorance leads to panic, guilt, and relapse.

Why People Stop Taking Their Medication - And What Happens After
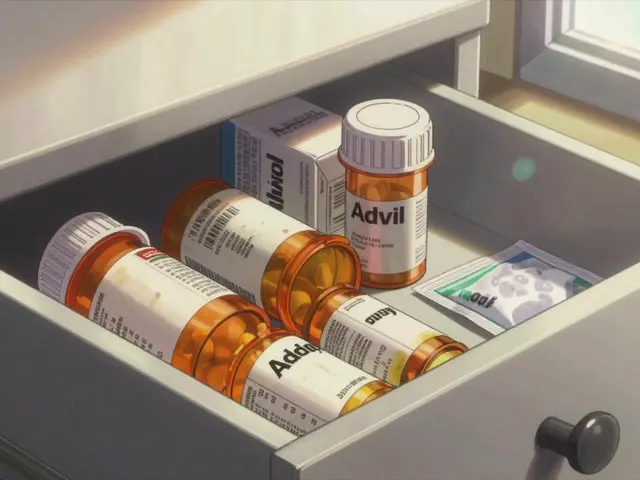
Real-world data shows only about 35% of people prescribed AUD meds keep taking them past three months. Why?
- Side effects: Diarrhea and nausea from acamprosate. Dizziness and fatigue from naltrexone. Metallic taste and drowsiness from disulfiram.
- Cost: Even generic versions cost $200-$400 a month. Many patients can’t afford it, especially without insurance.
- Lack of results: If you don’t feel immediate change, you assume it’s not working. But these drugs don’t create euphoria or quick fixes. Their benefit is quiet - fewer cravings, less bingeing, more stability over time.
- Isolation: Most people take these meds without therapy. No one checks in. No one holds them accountable. When cravings hit, they’re alone with the pill bottle - and often, they choose the drink.
When people stop taking their meds, relapse rates jump. One study found that patients who stopped naltrexone after 12 weeks were three times more likely to return to heavy drinking than those who continued. The medication wasn’t the problem - the lack of ongoing support was.
Who Benefits Most - And Who Should Avoid These Drugs
Not everyone responds the same way. Your biology, history, and goals matter.
If your main goal is total abstinence and you’ve already detoxed, acamprosate is your best bet. It’s gentle, doesn’t interact badly with other meds, and works best over months.
If you struggle with heavy drinking episodes - say, binging on weekends - naltrexone might help. But only if you’re willing to accept that it won’t stop you from drinking entirely. You need to be okay with reducing harm, not just stopping.
If you’re highly motivated, have a strong support system, and are terrified of drinking again, disulfiram can work. But if you’re unsure, impulsive, or live alone, it’s a ticking time bomb.
And if you have liver disease? Avoid naltrexone and disulfiram. They can worsen liver damage. Gabapentin, though not FDA-approved for AUD, is now being used off-label for patients with cirrhosis - and studies show it reduces liver decompensation by 37%. It’s safer, but still requires kidney function checks.
What Actually Works: The Missing Piece
Here’s what the data says clearly: medications alone don’t prevent relapse. They’re tools - not solutions.
The landmark COMBINE study found no extra benefit from combining acamprosate and naltrexone. But it did find that patients who got counseling - even just 10 sessions of motivational enhancement therapy - had significantly better outcomes than those who only took pills.
Patients who attended weekly group therapy, tracked their triggers in a journal, and had a sponsor or coach were far more likely to stay sober than those who just filled a prescription.
It’s not about the drug. It’s about building a new life. Medications can take the edge off cravings. But only you can choose not to drink - and that choice needs support, structure, and repetition.
What to Do If You’re on Medication and Feeling Trapped
If you’re taking one of these drugs and feel like it’s not helping - or worse, making you want to drink more - you’re not failing. The system is.
Here’s what to do:
- Don’t quit cold turkey. Stopping suddenly can trigger withdrawal or rebound cravings. Talk to your doctor.
- Ask about alternatives. Gabapentin, topiramate, or even off-label options like nalmefene might suit you better.
- Find therapy. Even one session a week with a counselor who specializes in addiction makes a measurable difference.
- Check your environment. Are you surrounded by people who drink? Do you have alcohol in your home? Your surroundings matter more than your prescription.
- Track your progress. Use an app or journal to record cravings, triggers, and days sober. Data beats guesswork.
Relapse isn’t the end. It’s feedback. If you drank while on naltrexone, maybe you need more counseling. If you stopped acamprosate because you felt no change, maybe you need more time - or a different approach. There’s no shame in adjusting your plan.
Future Hope: Personalized Treatment Is Coming
Science is moving beyond one-size-fits-all. New research uses brain scans to predict who will respond to acamprosate - based on white matter integrity. Genetic tests can spot people with serotonin transporter mutations who respond 2.3 times better to ondansetron.
Long-acting naltrexone implants (6-month doses) are in trials and show 78% adherence versus 42% for monthly shots. Digital apps that track cravings in real time and offer coping strategies have reduced relapse by 33% in recent studies.
But none of this matters if we keep treating AUD like a simple pill problem. It’s a complex brain disorder - and recovery needs more than chemistry. It needs connection, patience, and courage.
Can I drink while taking naltrexone or acamprosate?
Technically, yes - but it’s not safe or smart. Naltrexone blocks the high from alcohol, but doesn’t stop you from drinking. Many people end up drinking more because they think they’re “protected.” Acamprosate doesn’t react with alcohol, but it only works if you’re sober. Drinking while on it means the medication won’t help your brain heal. Both drugs lose effectiveness if you’re not fully committed to abstinence.
Why do some people relapse even when they take their medication?
Medications reduce cravings and heavy drinking, but they don’t remove the emotional triggers, stress, trauma, or loneliness that often drive relapse. If you’re taking the pill but not working through those deeper issues - through therapy, support groups, or lifestyle changes - you’re fighting the battle with one hand tied behind your back. The drug helps, but it doesn’t heal.
Is disulfiram worth the risk?
Only for a very specific group: highly motivated individuals with strong support systems who understand the consequences and avoid all alcohol sources - including perfumes, mouthwashes, and sauces with alcohol. For most people, the risk of accidental exposure, side effects, and psychological burden outweighs the benefit. It’s not the first-line choice for good reason.
How long should I stay on AUD medication?
Most studies show benefits last 6 to 12 months. But AUD is a chronic condition, like hypertension or diabetes. Many people need to stay on medication longer - even years. The key is not how long you take it, but whether it’s helping you live a better life. If you’re stable, sober, and thriving, staying on it is smart. If you’re struggling, talk to your doctor about adjusting your plan.
Are there cheaper alternatives to these medications?
Disulfiram is the cheapest - often under $50 a month. But cost isn’t everything. Gabapentin, used off-label, is affordable and safer for people with liver disease. Some clinics offer sliding-scale fees or free counseling alongside medication. The real cost is not the pill - it’s the hospital visits, lost jobs, and broken relationships that come with untreated AUD. Investing in treatment saves money long-term.




Darragh McNulty
November 20, 2025 AT 17:46Willie Doherty
November 22, 2025 AT 01:53David Cusack
November 23, 2025 AT 00:24Elaina Cronin
November 24, 2025 AT 23:56Noah Fitzsimmons
November 25, 2025 AT 13:10Eliza Oakes
November 27, 2025 AT 08:51Clifford Temple
November 28, 2025 AT 18:28Shawn Sakura
November 30, 2025 AT 11:05jim cerqua
December 2, 2025 AT 05:19Donald Frantz
December 3, 2025 AT 01:14Erika Sta. Maria
December 4, 2025 AT 09:59Debanjan Banerjee
December 4, 2025 AT 13:09Steve Harris
December 5, 2025 AT 08:35Michael Marrale
December 6, 2025 AT 10:13David vaughan
December 8, 2025 AT 05:18