What Happens After a Stroke?
When a stroke happens, the brain loses blood flow to part of its tissue. That part can’t send signals anymore. Muscles go weak. Speech gets fuzzy. Walking becomes hard. But here’s the truth: stroke rehabilitation doesn’t just help you recover-it rebuilds your brain.
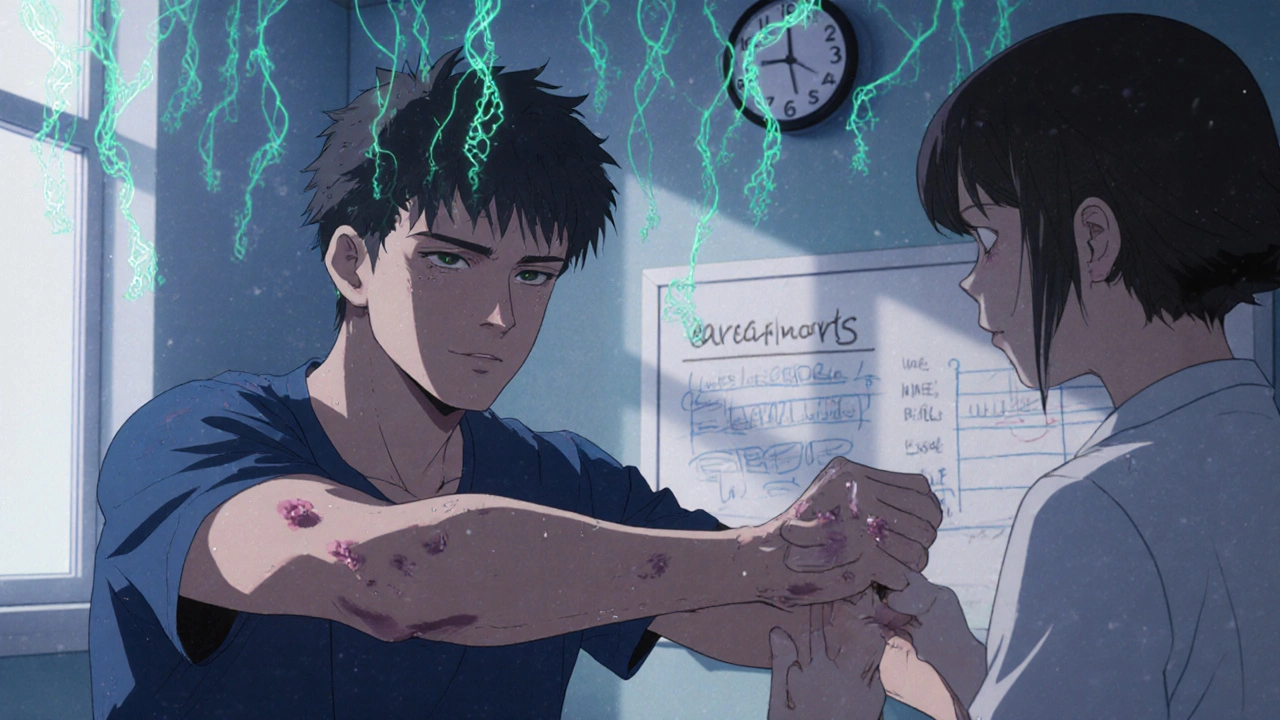
It’s not magic. It’s science. The brain isn’t a fixed machine. It rewires itself. This is called neuroplasticity. Damaged areas don’t come back to life, but healthy parts learn to take over. Think of it like rerouting traffic after a road closes. The brain finds new paths. And with the right therapy, those paths get stronger.
The Three Stages of Recovery
Recovery doesn’t happen all at once. It comes in three clear stages, each with its own focus.
Stage 1: Recovery and Natural Healing - This starts in the first days after the stroke. Swelling goes down. Some movement returns on its own. You might sit up. Move a finger. This isn’t therapy yet-it’s your body’s first response. But even now, therapists are working behind the scenes. They position your limbs to prevent stiffness. They move your joints gently. Why? Because if you don’t, muscles tighten. Joints lock. That’s called contracture. It affects 30-50% of people who skip this step.
Stage 2: Retraining - This is where real progress begins. Weeks to months after the stroke, you start doing things over and over. Sitting up. Reaching for a cup. Taking a step. Therapists use cues-pointing to a wheelchair brake, showing you how to grip a spoon. Repetition builds new neural connections. Studies show that doing these tasks 3 hours a day, 5 days a week, leads to the best results. And starting within 24 hours? That boosts mobility gains by 35%.
Stage 3: Adaptation - Not everyone gets all their abilities back. That’s okay. This stage is about learning to live with what’s left. Maybe your arm doesn’t lift fully. Maybe you need help speaking. Therapists teach you workarounds. A longer-handled brush. A voice-controlled light switch. A speech app. And family? They’re part of this. People with family support stick to therapy 37% longer. That’s huge.
The Team Behind Your Recovery
No single person can do this alone. Recovery needs a team.
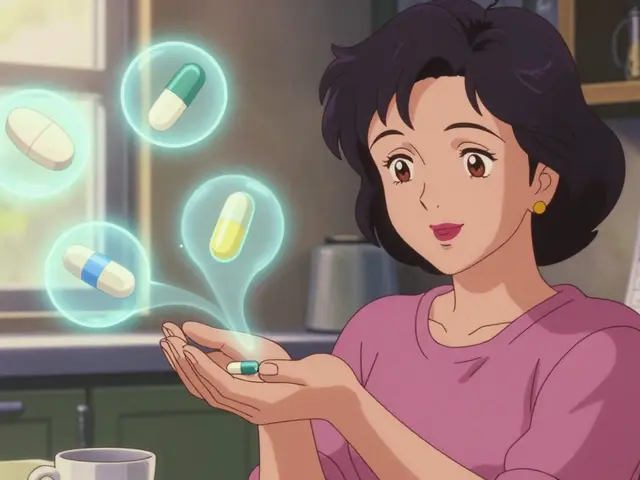
Physiatrists-doctors who specialize in rehab-lead the group. They set goals. Physical therapists work on walking, balance, strength. Occupational therapists help you dress, cook, brush your teeth again. Speech-language pathologists fix swallowing and talking. Psychologists help with the emotional toll-depression hits 30-35% of stroke survivors. Nutritionists make sure you’re eating right. Social workers connect you to home care or support groups.
And here’s the kicker: clinics with regular team meetings see 22% better outcomes. Why? Because everyone talks. The physical therapist tells the speech therapist that you’re struggling to hold a spoon. The psychologist tells the social worker you’re afraid to go out. That coordination saves time. It saves frustration. It saves your life.
Therapies That Actually Work
Not all therapy is the same. Some methods are backed by hard data.
- Motor-skill exercises - Repeating arm lifts, leg kicks, finger taps. After 12 weeks, most people gain 40-60% faster walking speed.
- Constraint-induced therapy - You wear a mitt on your good hand for 90% of the day. You have to use the weak one. Mayo Clinic studies show 30% more improvement than standard care.
- Functional electrical stimulation - Small electric pulses make weak muscles twitch. This helps wrist and hand function improve by 25-45%.
- Robotic devices - Machines guide your leg or arm through walking or reaching motions. Lokomat robots improve walking speed by 50% more than traditional therapy.
- Virtual reality - You play games that make you reach, grab, step. It boosts upper limb function by 28% compared to regular exercises.
- Balance training - 60% of stroke survivors lose balance. Simple drills-standing on one foot, shifting weight-cut fall risk in half.
Even simple tech helps. Wireless step counters? They push people to walk 32% more. That’s not a gadget-it’s a lifeline.

Timing Is Everything
Waiting to start rehab? That’s dangerous.
Every day you delay, muscles weaken. Joints stiffen. Your confidence drops. Depression creeps in. The American Stroke Association says: as soon as you’re medically stable, therapy starts. That could be hours after the stroke. Not days. Not weeks.
And intensity matters. Three hours a day, five days a week, in a rehab facility is the gold standard. If you’re home, you need the same energy. That means daily exercises, not just “I’ll do it when I feel like it.”
Studies show motivation is the biggest predictor of success. It accounts for up to 40% of how well you recover. That’s more than age, more than stroke severity. If you’re willing to try, your brain will meet you halfway.
What Happens After You Leave Rehab?
Most people leave rehab after 2-8 weeks. But recovery doesn’t stop.
Seven out of ten stroke survivors need ongoing therapy. That’s where community programs and telerehabilitation come in. Video calls with therapists. Apps that track your progress. Home exercise plans sent to your phone. Research shows telerehab is 85% as effective as in-person visits.
Don’t stop. Don’t assume you’re “done.” Your brain is still rewiring. Keep moving. Keep practicing. Even small daily efforts-ten minutes of stretching, five minutes of naming objects-add up over months.
What’s New in Recovery?
Science is moving fast.
Transcranial magnetic stimulation (TMS) uses magnets to stimulate brain areas. When paired with therapy, it boosts motor recovery by 15-20%.
Artificial intelligence is starting to personalize rehab. It looks at your brain scans, your movement patterns, your progress-and adjusts your exercises in real time.
And in some cases, surgery helps. Cranioplasty-fixing a skull fracture after trauma-has been shown to improve cognition by 25% when combined with rehab.
These aren’t sci-fi. They’re happening now. In hospitals in Bristol, London, and beyond.

Key Factors That Make Recovery Work
Success isn’t random. It’s built on nine things:
- Your overall health before the stroke
- How much movement you have left
- Your muscle strength
- Control over bladder and bowel
- What you could do before the stroke
- Your home support system
- How you learn best
- Your motivation
- Your ability to cope with change
Two stand out: motivation and support. If you believe you can get better, you will. If someone’s there to remind you, cheer you on, or help you do your exercises-you’re twice as likely to stick with it.
How to Stay on Track
Recovery isn’t a sprint. It’s a marathon with ups and downs.
Balance your day: 40-50% on therapy, 30-40% resting, 20-30% socializing. Too much exercise? You burn out. Too little? You lose ground. Too isolated? Depression wins.
Set tiny goals. Move your fingers 5 degrees more this week. Stand for 30 seconds longer. Celebrate those wins. They matter.
And remember: you’re not broken. You’re rebuilding. Every rep. Every step. Every word you try to say. That’s your brain learning. That’s progress.
How long does stroke recovery take?
Recovery happens in stages. Most people see the biggest gains in the first 3-6 months. But the brain can keep rewiring for years. Some patients improve even after 2-3 years with consistent therapy. There’s no finish line-just progress.
Can you recover fully after a stroke?
Some people do. Others learn to live with lasting changes. The goal isn’t always to go back to exactly how you were before. It’s to regain as much independence and quality of life as possible. Many return to work, drive, travel, and enjoy hobbies-even with some limitations.
Is it too late to start rehab if it’s been months since my stroke?
No. While early rehab gives the best results, neuroplasticity doesn’t shut off. Studies show people still improve with therapy even 1-2 years after a stroke. The key is consistency. Daily practice, even for short periods, keeps your brain adapting.
What’s the most important part of stroke rehab?
Motivation. You can have the best therapist, the most advanced tech, and the perfect plan-but if you don’t show up, nothing works. Your willingness to try, to fail, to try again, is what drives recovery. Support from family and friends helps keep that motivation alive.
Can technology replace human therapists?
No. Robots, apps, and virtual reality are tools-they enhance therapy, not replace it. A therapist reads your body language, adjusts your effort, encourages you when you’re frustrated, and knows when to push or rest. Tech helps you practice more. But human connection keeps you going.
How do I know if my rehab program is working?
Look for small wins: Can you hold a cup without spilling? Walk to the kitchen without help? Say your name clearly? These are signs your brain is rewiring. Your therapist should track progress with tests every 4-6 weeks. If you’re not improving after 8-12 weeks, ask for a plan review.
What should I avoid during recovery?
Don’t overdo it-fatigue slows healing. Don’t isolate yourself-loneliness worsens depression. Don’t skip therapy because you’re frustrated. And don’t assume you’re “fine” just because you can walk. Balance, strength, and coordination need ongoing attention. Recovery is a long game.
Final Thought
Stroke doesn’t define you. How you rebuild does. Every step, every word, every attempt-those are your brain’s way of saying it hasn’t given up. And neither should you.





Kristina Williams
November 17, 2025 AT 15:13Louie Amour
November 18, 2025 AT 01:40Holly Powell
November 19, 2025 AT 13:22Christine Eslinger
November 21, 2025 AT 07:24Emanuel Jalba
November 21, 2025 AT 13:15Heidi R
November 22, 2025 AT 15:27Brenda Kuter
November 24, 2025 AT 06:17Shilpi Tiwari
November 24, 2025 AT 18:05Shaun Barratt
November 25, 2025 AT 20:24Iska Ede
November 27, 2025 AT 10:07Gabriella Jayne Bosticco
November 27, 2025 AT 11:45Sarah Frey
November 29, 2025 AT 00:24