Inflammatory Bowel Disease Reproductive Health
When working with Inflammatory Bowel Disease Reproductive Health, the ways IBD influences fertility, pregnancy, and postpartum outcomes. Also known as IBD reproductive health, it covers both the medical and lifestyle aspects that matter to anyone trying to conceive or stay pregnant while managing IBD.
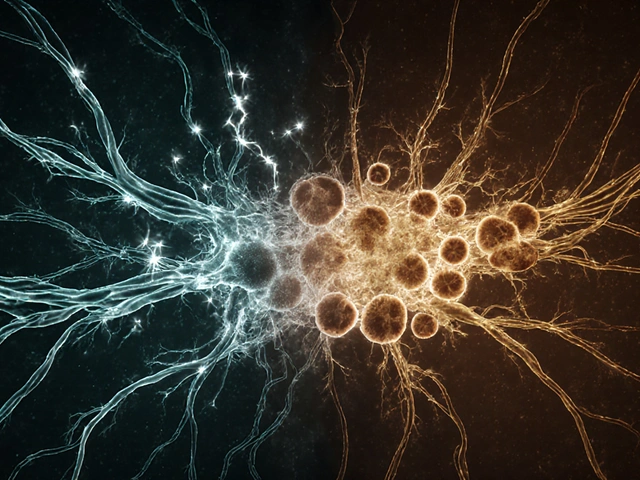
Two of the most common IBD subtypes are Crohn's disease, a chronic inflammation that can affect any part of the GI tract and ulcerative colitis, an ulcerating condition limited to the colon. Both conditions can disrupt hormone balance, alter nutrient absorption, and increase the risk of miscarriage. Understanding these differences is the first step toward planning a healthy pregnancy.
Key Topics Covered in This Collection
Inflammatory bowel disease reproductive health isn’t just a medical jargon phrase; it’s a guide to real‑world decisions. Fertility is often the first concern. Studies show that active disease lowers sperm count and ovulation quality, while surgery can improve outcomes if timing is right. Nutrition plays a huge role, too—low iron, folate, or vitamin D can stall conception. Fertility, the ability to conceive a child is directly linked to disease remission and adequate weight.
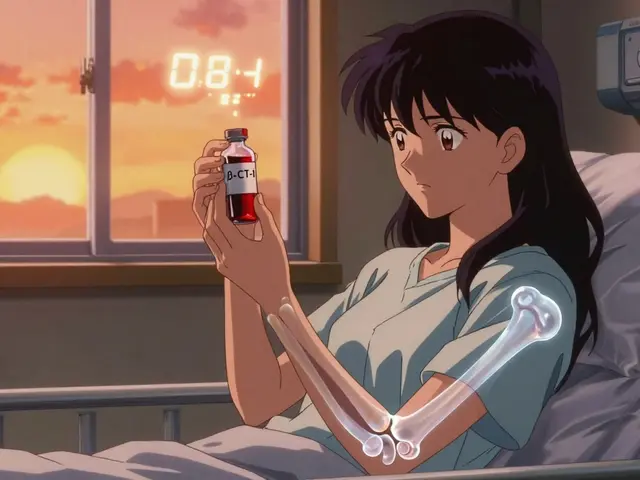
Pregnancy adds another layer. Medication safety becomes a tightrope walk—some biologics are considered low risk, while others are off‑limits after the first trimester. Medication management, adjusting IBD drugs for pregnancy often requires a collaborative approach between gastroenterologists and obstetricians. Women who stay in remission through the first two trimesters typically have full‑term births, whereas flare‑ups can lead to preterm delivery or low birth weight.
Genetics also matters. A family history of IBD raises the chance of passing the condition to the child, but genetic counseling can clarify risk percentages and help couples decide on prenatal testing. Genetic counseling, professional advice on inherited disease risk is especially valuable when both partners have IBD.
Beyond the medical side, lifestyle tweaks make a big difference. Stress reduction, balanced diet, and regular exercise support both disease control and reproductive health. Research links high‑fiber, low‑sugar meals to fewer flares, which in turn supports a stable hormonal environment. Breastfeeding after delivery is usually safe, though some medications may need to be paused to avoid infant exposure.
Putting it all together, the central idea is simple: successful family planning with IBD requires coordinated care, disease remission, and personalized nutrition. Below, you’ll find articles that break down each of these pieces—whether you’re looking for medication comparisons, diet tips, or step‑by‑step guides for pregnancy tracking while on IBD therapy. Dive in to get the practical insights you need to move forward confidently.
Colitis, Fertility & Reproductive Health: What You Need to Know
By Lindsey Smith On 8 Oct, 2025 Comments (19)

Learn how colitis influences fertility and pregnancy, discover management tips, medication safety, and a practical checklist for couples planning a family.
View More