Optic Neuritis: What You Need to Know
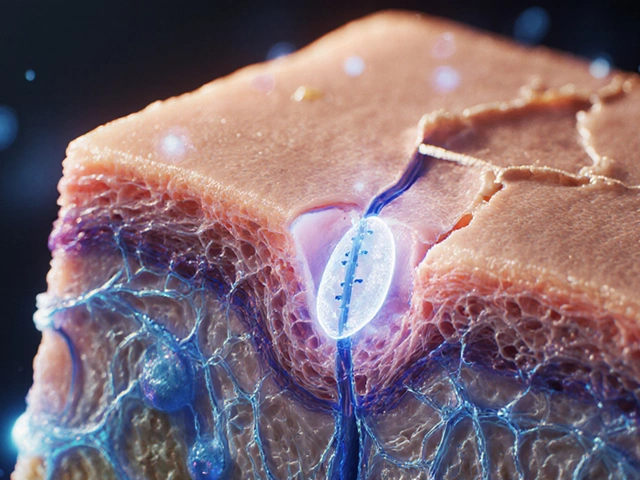
Seeing flashes, blurred spots, or a sudden dip in vision can be scary. In many cases, the culprit is optic neuritis – an inflammation of the optic nerve that carries visual info from your eyes to the brain. It often hits one eye, sometimes both, and can happen to anyone, though it’s more common in young adults.
Most people notice vision changes over a few days. Pain behind the eye, especially when moving it, is another red flag. If you feel these symptoms, don’t ignore them; early evaluation can speed up recovery and prevent lasting damage.
Why Does Optic Neuritis Occur?
Inflammation can be triggered by several things. Autoimmune disorders like multiple sclerosis (MS) are the top suspects – the immune system mistakenly attacks the optic nerve. Infections, including viral or bacterial illnesses, can also set off inflammation. Less often, certain medications or vitamin deficiencies play a role.
Because the exact cause isn’t always clear, doctors often run a battery of tests. An MRI of the brain and eyes helps spot lesions linked to MS. Blood work checks for infections or autoimmune markers. A visual evoked potential test measures how fast signals travel from the eye to the brain, confirming nerve slowdown.
How Is Optic Neuritis Treated?
Most doctors start with high‑dose steroids, either IV or oral, to melt the inflammation quickly. Steroids don’t cure the condition but can shorten the recovery window from weeks to days. After the steroid burst, a tapering schedule helps avoid rebound symptoms.
If steroids aren’t an option or the inflammation persists, plasma exchange (PLEX) or IVIG may be considered. Physical therapy isn’t typical, but vision rehabilitation exercises can help the brain rewire around any residual visual gaps.
Recovery varies. Many regain near‑normal vision within a month, while others keep mild deficits. Keeping regular follow‑ups with a neurologist or ophthalmologist ensures any underlying disease, like MS, gets caught early.
Below are some of the latest articles on our site that touch on topics you might find useful while navigating optic neuritis:
- Xanthan Gum in Supplements – Learn about safe ingredient swaps if you’re taking oral steroids.
- How to Safely and Easily Buy Adalat Online – Guides you on purchasing blood‑pressure meds, which sometimes help manage optic nerve swelling.
- Pravachol: Everything You Need to Know – Cholesterol meds can affect overall vascular health, a factor in optic nerve health.
- Rizact Uses, Dosage, Side Effects – Migraine treatments may overlap with eye‑pain management.
- Proton Pump Inhibitor Side Effects – Long‑term PPI use can alter vitamin B12 levels, relevant for nerve health.
- Burning Sensation and Anxiety – Anxiety can amplify visual disturbances; this article offers coping tips.
- Top Over‑the‑Counter Vertigo Meds – When dizziness accompanies optic neuritis, these options might help.
Remember, optic neuritis isn’t something you should self‑diagnose. If you notice vision changes or eye pain, book an eye‑doctor or neurologist appointment right away. Early treatment boosts the chances of a full comeback and helps catch any hidden conditions early.
Stay informed, keep track of any new symptoms, and don’t hesitate to ask your doctor about the best treatment plan for you.
Nitrofurantoin Eye Problems: Symptoms, Risks, and When to Seek Help
By Lindsey Smith On 5 Sep, 2025 Comments (9)

Worried about eye issues on nitrofurantoin? Learn rare risks, red flags, who’s at risk, and what to do-grounded in BNF, FDA labels, and UK guidance.
View More