Why Older Bodies Handle Medicines Differently
When you’re 70, your body doesn’t process pills the same way it did at 40. That’s not just a guess-it’s science. As we age, our organs change. The liver slows down. Kidneys filter less. Fat increases, muscle decreases. These shifts mean drugs stay in your system longer, build up over time, and can turn harmless doses into dangerous ones.
Take gabapentin, a common nerve pain med. A healthy adult might start at 300 mg daily. But for someone over 65 with reduced kidney function? That same dose can cause dizziness, falls, or confusion. The right starting dose? Often 100 to 150 mg. It’s not about being weak-it’s about matching the medicine to the body.
This isn’t rare. Nearly 60% of medications prescribed to people over 65 need some kind of dosage tweak. And here’s the scary part: 35% of hospital visits by seniors are caused by bad drug reactions. Most of them? Could’ve been avoided with a simple dose adjustment.
The Four Ways Aging Changes How Drugs Work
Every drug goes through four steps in your body: absorption, distribution, metabolism, and excretion. Aging messes with all four.
- Absorption: Stomach acid drops by 20-30% as we age. That means some pills don’t dissolve as well. Iron, vitamin B12, and certain antibiotics absorb less efficiently.
- Distribution: Older adults tend to have more body fat and less muscle. Fat-soluble drugs like diazepam (Valium) stick around longer. Water-soluble drugs like lithium get concentrated faster because there’s less water in the body to dilute them.
- Metabolism: The liver shrinks and blood flow drops. That means drugs like warfarin, statins, and many antidepressants break down 30-50% slower. A normal dose can become toxic.
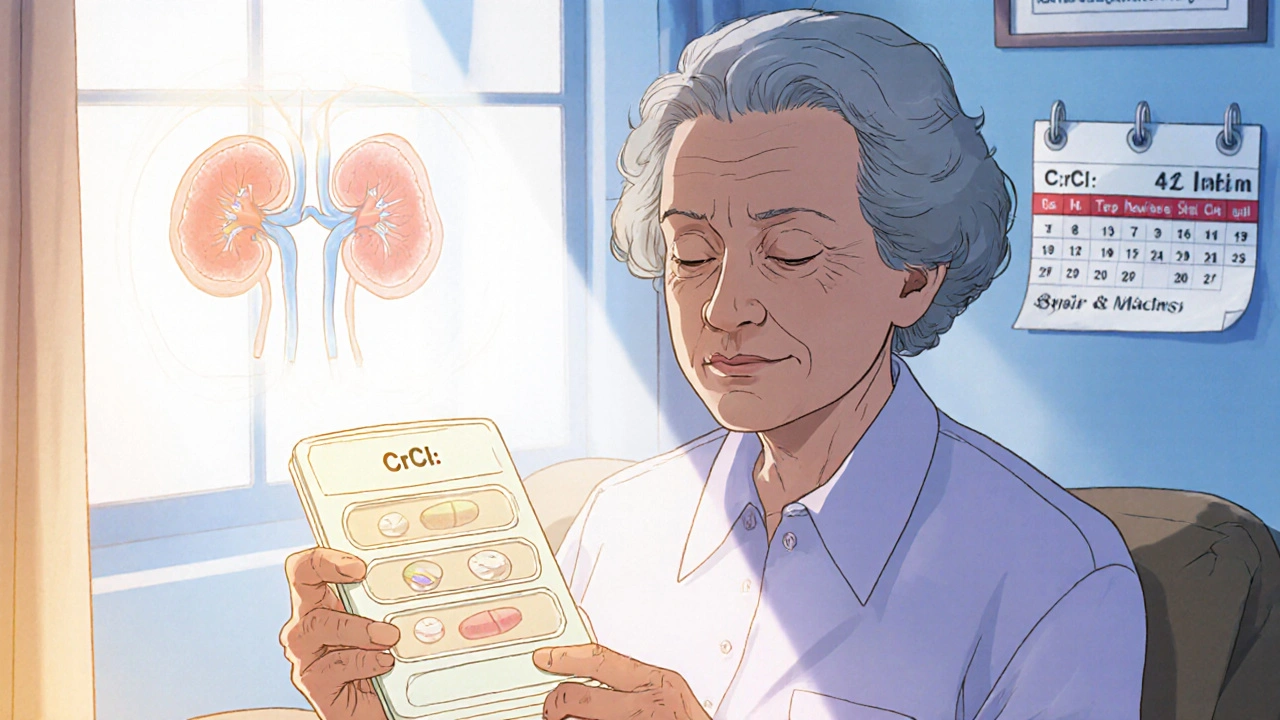
- Excretion: Kidneys are the biggest concern. After age 30, kidney function drops about 8 mL per minute every decade. By 70, many people have less than half the kidney filtering power they had in their 30s. Drugs like metformin, digoxin, and antibiotics cleared by the kidneys can pile up dangerously if not adjusted.
That’s why doctors don’t just look at age-they look at kidney function. The go-to test? Creatinine clearance. It’s calculated using age, weight, and a blood test. If your creatinine clearance is below 50 mL/min, most kidney-cleared drugs need a lower dose. Some, like metformin, shouldn’t be used at all if it’s below 30.
High-Risk Drugs for Seniors (And What to Do Instead)
The American Geriatrics Society updates its Beers Criteria® every two years. The 2023 list names 30 classes of drugs that are risky for older adults. Here are the top offenders:
- Benzodiazepines: Drugs like lorazepam (Ativan) and diazepam (Valium) increase fall risk by 50%. They’re often prescribed for anxiety or sleep, but safer alternatives include cognitive behavioral therapy or low-dose trazodone.
- NSAIDs: Ibuprofen, naproxen-even over-the-counter ones-raise the risk of stomach bleeding by 300% in seniors. Acetaminophen is usually safer, but watch liver function.
- Anticholinergics: Found in many sleep aids, bladder meds, and even some allergy pills, these drugs double dementia risk with long-term use. Check labels for ingredients like diphenhydramine or oxybutynin.
- Anticoagulants: Warfarin needs careful monitoring. Seniors often need 20-30% lower doses. Newer drugs like apixaban are often safer and don’t need constant blood tests.
- Hypoglycemics: Sulfonylureas like glyburide can cause dangerous low blood sugar. Metformin is preferred if kidneys allow. GLP-1 agonists like semaglutide are newer, safer options for type 2 diabetes.
It’s not about avoiding all these drugs. It’s about using them wisely. Sometimes, the right move is to stop one, lower the dose, or switch to something with fewer side effects.
How Dose Adjustments Are Calculated
Doctors don’t guess. They use formulas. The most common one is the Cockcroft-Gault equation:
CrCl = [(140 - age) × weight (kg)] ÷ [72 × serum creatinine (mg/dL)] × 0.85 (if female)
This gives an estimate of kidney function. If your result is below 50, most drugs cleared by the kidneys need a 25-50% reduction. For liver-metabolized drugs, doctors use the Child-Pugh score. A score of 7-9 means cut the dose in half. A score of 10-15? Avoid the drug entirely.
For drugs like digoxin, where the window between helpful and harmful is narrow, blood levels are checked. In seniors, the target range is 0.5-0.9 ng/mL. In younger people? 0.8-2.0. That’s a big difference.
But here’s the problem: only 15% of commonly prescribed drugs have blood tests like this. For the rest, doctors rely on experience, guidelines, and watching for side effects.
The Real-World Challenge: Too Many Pills, Too Little Time
More than half of seniors take five or more prescription drugs. That’s called polypharmacy. It’s not always wrong-many need them. But each new drug increases the chance of a bad reaction.
Doctors are stretched thin. A typical visit lasts 15-20 minutes. A full medication review? Takes 35 minutes on average. That’s why so many errors slip through.
But there are proven fixes:
- Brown bag review: Bring all your pills-prescriptions, OTC, supplements-to your appointment. Pharmacists see what’s really being taken.
- Electronic alerts: Many EHR systems now flag when a drug dose is too high for kidney function. One study showed this cuts errors by 53%.
- Pharmacist-led care: In programs like UNC’s Pharm400, pharmacists manage dosing, adjust meds weekly, and use blister packs. Hospital visits dropped by 22%.
- Family involvement: When a caregiver helps track doses and side effects, adherence improves by 37%.
The goal isn’t to cut every pill. It’s to make sure each one is still necessary, at the right dose, and not causing more harm than good.
What You Can Do Right Now
You don’t need to be a doctor to help manage medication safety. Here’s what works:
- Ask your doctor: “Is this medicine still right for me at my age?” and “Could this cause dizziness or confusion?”
- Check your kidney function: Ask for your eGFR or creatinine clearance number. Know what it is.
- Review your list: Every 6 months, sit down with a pharmacist and go over every pill you take. Don’t forget vitamins, herbal supplements, and OTC meds.
- Watch for red flags: New falls, memory lapses, loss of appetite, or extreme fatigue? These aren’t just “getting older.” They could be drug side effects.
- Use one pharmacy: It helps them spot dangerous interactions across all your meds.
Many seniors feel embarrassed to ask, “Is this still needed?” But the truth is, your body has changed. So should your meds.
The Future: Personalized Dosing Based on Function, Not Age
Age is just a number. What matters more is how your body works. Are you walking slowly? Struggling to get up from a chair? Having trouble remembering to take pills? These are signs of frailty-and they matter more than your birth year.
Researchers are now testing dosing based on functional age. The Timed Up and Go test (TUG), which measures how fast someone stands, walks 3 meters, turns, and sits down, is being added to dosing guidelines. If your TUG is over 12 seconds, you’re at higher risk for falls from meds-even if your kidneys look fine.
AI tools are also emerging. Johns Hopkins tested a program called MedAware that predicts dangerous doses. It cut errors by 47%. The NIH is investing $127 million to build models that predict how drugs behave in older bodies-not just averages, but for each person.
By 2030, personalized, kidney- and liver-adjusted dosing could be standard for 70% of high-risk medications. That means fewer hospital stays, fewer falls, and more years living well.
Final Thought: It’s Not About Cutting Doses-It’s About Getting It Right
Lowering a dose isn’t a step backward. It’s a step toward safety. A 75-year-old on the right dose of blood pressure medicine can live longer, stronger, and more independently than a 65-year-old on the “standard” dose that’s too high.
The system isn’t perfect. Too many clinical trials still leave out people over 75. Too many doctors haven’t been trained in geriatric pharmacology. But progress is happening. And you don’t have to wait for the system to catch up.
Start with one question: “Is this dose still right for me?” Then bring your pills. Talk to your pharmacist. Watch your body. You know it better than anyone.

Victoria Short
November 15, 2025 AT 22:00My grandma takes 12 pills a day and still says she's fine. I just nod and hide the list from her doctor.
Jessica M
November 16, 2025 AT 17:43It is imperative that healthcare providers prioritize individualized pharmacokinetic assessments in geriatric populations. The physiological changes associated with aging necessitate a departure from standardized dosing protocols, particularly with regard to renal clearance and hepatic metabolism. Adherence to the Beers Criteria and utilization of the Cockcroft-Gault equation are not merely best practices-they are ethical obligations.
Eric Gregorich
November 18, 2025 AT 00:27You know what really breaks my heart? The fact that we treat old people like broken machines that need tuning, not like humans who’ve lived decades and deserve dignity. My dad was on gabapentin for five years because the doctor didn’t bother to check his creatinine. He fell three times. Broke his hip. Then they said, ‘Well, he’s just getting old.’ No. He got old because we stopped listening. We don’t need more algorithms-we need more people who care enough to ask, ‘Is this really helping?’
I’ve sat in 17-minute doctor visits where the only question was, ‘Any new chest pain?’ Not a word about his meds. Not one. And now he’s on eight drugs that probably cause the fatigue he’s too tired to complain about. This isn’t medicine. It’s neglect dressed in white coats.
sara styles
November 19, 2025 AT 00:51Let me tell you something they don’t want you to know. The FDA and Big Pharma have been hiding this for decades. They know older bodies react differently, but they don’t want you to know because it cuts into profits. Why do you think they still test drugs on 25-year-olds? Because if they tested on real people-people over 70-they’d have to admit most pills are dangerous for seniors. So they keep selling the same doses, then charge you extra for the ER visits. It’s a racket. And your doctor? They’re just following the script. The real villains? The pharmaceutical lobbyists who wrote the guidelines. Google ‘Pharma Influence on Beers Criteria’ and see what comes up. They don’t want you to see the truth.
They say ‘check your kidney function’-but what if your doctor doesn’t order the test? What if they’re too lazy? What if they’re paid by drug reps? I’ve seen it. My aunt’s doctor prescribed her a drug that’s on the Beers list… and then told her it was ‘safe because she’s healthy.’ She’s 82 and walks with a cane. Healthy? No. She’s being poisoned slowly. And no one’s stopping it.
They want you to think it’s your fault if you get dizzy. That it’s ‘just aging.’ But it’s not. It’s corporate greed wrapped in medical jargon. The only way to fight this? Stop trusting doctors blindly. Bring every pill to every appointment. Record every side effect. And if they don’t listen? Change doctors. Find someone who actually reads the research. Or better yet-go to a pharmacist. They know more than you think.
And don’t even get me started on AI tools like MedAware. That’s just another way to make you feel safe while they keep selling the same toxic pills. AI doesn’t care if you fall. AI doesn’t care if you die. AI just wants to process more data. They’re using tech to cover up their negligence. It’s scary. And it’s all connected.
Koltin Hammer
November 20, 2025 AT 03:01I used to think aging was just about gray hair and stiff knees. Then I watched my uncle go from hiking the Rockies to needing help to get out of bed-all because of a cocktail of meds he didn’t even know he was on. Turns out, his ‘sleep aid’ was diphenhydramine. His ‘blood pressure pill’ was a beta-blocker that tanked his heart rate. His ‘arthritis painkiller’ was naproxen that gave him a GI bleed. He didn’t need more drugs-he needed fewer. And someone who actually sat down with him and asked, ‘What are you trying to fix?’
It’s not about age. It’s about function. My uncle’s TUG score was 18 seconds. That’s not ‘old.’ That’s ‘danger zone.’ But his doctor didn’t know what that meant. And that’s the real problem. We’ve turned medicine into a checklist, not a conversation. We measure life in lab results, not in how well you can hug your grandkid without falling.
There’s a quiet revolution happening in geriatric pharmacy. People like my aunt’s pharmacist-they’re the unsung heroes. She printed out his meds in color-coded pills. Made a chart. Called him every week. Said, ‘If you feel weird, call me. Even at 2 a.m.’ That’s care. Not algorithms. Not guidelines. A person who shows up.
Maybe the future isn’t AI. Maybe it’s just someone who remembers that your grandma isn’t a data point. She’s the woman who taught you how to bake pies. And she deserves to keep baking them.
Connor Moizer
November 21, 2025 AT 22:50I’ve been a caregiver for my mom for 7 years. I’ve learned one thing: if you don’t track every pill, someone will overdose her by accident. I keep a spreadsheet. I call the pharmacy every month. I’ve fired two doctors who didn’t listen. And I’ve learned to ask, ‘What happens if we stop this?’ Not ‘Can we add this?’
One time, I asked about her anxiety med. The doc said, ‘It’s fine.’ I said, ‘She’s been sleeping 16 hours a day.’ He said, ‘That’s normal for her age.’ I said, ‘No. That’s benzo toxicity.’ I pulled the paper. He changed it the next day. Don’t be polite. Be loud. Be annoying. Because if you don’t, no one will.
Phil Best
November 23, 2025 AT 06:12Let’s be real: if you’re over 70 and still taking 10 pills a day, you’re not surviving-you’re surviving *despite* the system. My uncle was on 14 meds. One was for constipation caused by another. Another was for the dizziness caused by a third. He was basically a human pharmacy experiment. Then he stopped all of them, one by one, with his pharmacist’s help. Within two weeks? He was walking his dog again. No falls. No confusion. Just… life.
The real tragedy? They told him he needed every pill. Turns out, 8 of them were prescribed for symptoms he didn’t even have anymore. That’s not medicine. That’s inertia. And it’s killing people slowly.
So if you’re reading this and you’re a senior? Go home. Grab your brown bag. Bring it to a pharmacist. Tell them: ‘I want to live, not just exist.’ And if they don’t get it? Find someone who does.
roy bradfield
November 24, 2025 AT 04:36They’re lying to you. The whole system is rigged. The WHO, the FDA, the AMA-they’re all in on it. They don’t want you to know that most elderly deaths from meds are preventable because they’re scared of the lawsuits. They’re using your parents and grandparents as test subjects. Look at the numbers: 35% of hospital visits? That’s not a statistic-that’s a massacre. And they’re still pushing these drugs because the money’s too good. They’ll keep doing it until the public wakes up. And you? You’re part of the problem if you don’t fight back.
I’ve got a friend whose mother died from a drug interaction. They told her it was ‘natural causes.’ But the autopsy said it was warfarin and ibuprofen. Two pills. One death. And the hospital never even asked if she was taking OTC meds. That’s not negligence. That’s malice. And they’ll keep doing it until someone stops them. So tell your friends. Tell your family. Don’t be quiet. They’re counting on you to stay silent.
Parv Trivedi
November 24, 2025 AT 06:21As someone from India, I’ve seen both sides. In rural areas, people take one or two medicines and trust their doctor completely. In cities, they take ten and never ask why. But here’s the truth: no matter where you are, the body doesn’t lie. If you feel weak, dizzy, or confused after starting a new pill, it’s not ‘just aging.’ It’s a signal.
My grandmother took metformin for 10 years. Her doctor never checked her kidneys. One day, she stopped eating. We rushed her. Her creatinine was 5.2. She was in kidney failure. We stopped the drug. She recovered. Now she takes half the dose. And she’s fine.
Don’t be afraid to ask. Don’t be ashamed to bring your pills. Your life matters more than the doctor’s schedule.
Liam Dunne
November 26, 2025 AT 00:19I’m a pharmacist. I’ve reviewed over 1,200 senior med lists. The most common mistake? Not the dose-it’s the *ghost pills*. Medications that were prescribed years ago, for a condition that’s gone, or symptoms that faded. People keep taking them because ‘it’s always been there.’ I’ve seen people on antihistamines for allergies they haven’t had since 2008. On statins because their cholesterol was high once. On sleeping pills because they had insomnia after their spouse died.
Most of these can be stopped safely-with guidance. You don’t need to be a genius. Just ask: ‘If I stop this, what’s the worst that could happen?’ Often? Nothing. And you’ll feel better.
And yes-use one pharmacy. It’s the single easiest thing you can do to avoid a deadly interaction.
Rebekah Kryger
November 27, 2025 AT 18:10Let’s be real-this whole post is just another way for pharma to sell more ‘geriatric-friendly’ drugs. They’re not reducing doses-they’re just rebranding old pills as ‘senior-safe.’ Metformin? Still toxic if your kidneys are bad. GLP-1 agonists? $1,000/month. Who’s gonna pay for that? The system wants you to think there’s a ‘better’ pill. There isn’t. There’s just more profit.
And don’t get me started on ‘functional age.’ That’s just code for ‘we’re too lazy to do proper lab tests.’ TUG score? Please. I’ve seen people who can walk fine but have zero kidney function. And others who shuffle but have perfect CrCl. You can’t reduce biology to a stopwatch.
Real solution? Stop prescribing so much in the first place. Not more tech. Not more scores. Less pills. Period.
Patrick Merk
November 29, 2025 AT 05:06I love this. My dad’s pharmacist is basically his personal medication therapist. She calls him every Tuesday. Asks if he’s feeling ‘off.’ Keeps a little notebook. She once caught that his blood pressure med was making him dizzy-because his dose hadn’t been adjusted since 2018. He’s 84. She didn’t wait for him to say anything. She just… cared.
That’s the kind of care we need more of. Not AI. Not guidelines. Just someone who shows up and listens.
Willie Randle
November 29, 2025 AT 15:25To every caregiver reading this: you are the most important person in your loved one’s healthcare team. You’re the one who notices the subtle changes-the hesitation before standing, the skipped meals, the confusion after a new prescription. No algorithm sees that. No doctor hears it unless you speak up.
Keep your list. Keep your questions. Keep your courage. You’re not being ‘difficult.’ You’re being their voice when they can’t find theirs.
And to the doctors reading this: if you’re not doing a full med review at least once a year with your older patients, you’re not doing your job. It’s not a luxury. It’s a duty.
kanishetti anusha
November 30, 2025 AT 00:02I’m a nurse in India. I’ve seen grandmas on 12 pills, and their kids don’t even know what half of them are for. I teach them to write down each pill’s name and why it’s taken. One grandma wrote: ‘Blue pill-doctor said for heart. But I think it makes me sleepy.’ That’s all it took. We stopped it. She slept 7 hours a night after.
You don’t need a PhD to help. Just curiosity. And courage.
Erika Lukacs
December 1, 2025 AT 19:49There is something profoundly melancholic about the modern medicalization of aging. We have turned the natural process of bodily decline into a problem to be corrected, rather than a condition to be understood. The obsession with dosage adjustments, biomarkers, and algorithmic safety reflects not a triumph of science, but a failure of imagination. We seek to engineer longevity, yet we forget to cultivate dignity. The real question is not whether the dose is correct-but whether the life being sustained is worth living.
Ann Klein
December 2, 2025 AT 15:33My dad died from a drug interaction. He was on 11 meds. The hospital said it was ‘natural causes.’ I got his records. Three of them shouldn’t have been prescribed together. The doctor never checked his kidney function. I’m still angry. If you’re reading this-don’t wait. Ask. Now. Before it’s too late.