Many heart patients take digoxin to manage heart failure or irregular heartbeats like atrial fibrillation. It’s been used for nearly a century, and it still works - but only if you know what to watch for. The difference between it helping you and harming you often comes down to one thing: interactions. Not just with other pills, but with food, supplements, and even everyday habits. This isn’t theoretical. People end up in the ER because they didn’t realize their morning oatmeal or over-the-counter antacid was messing with their digoxin levels.
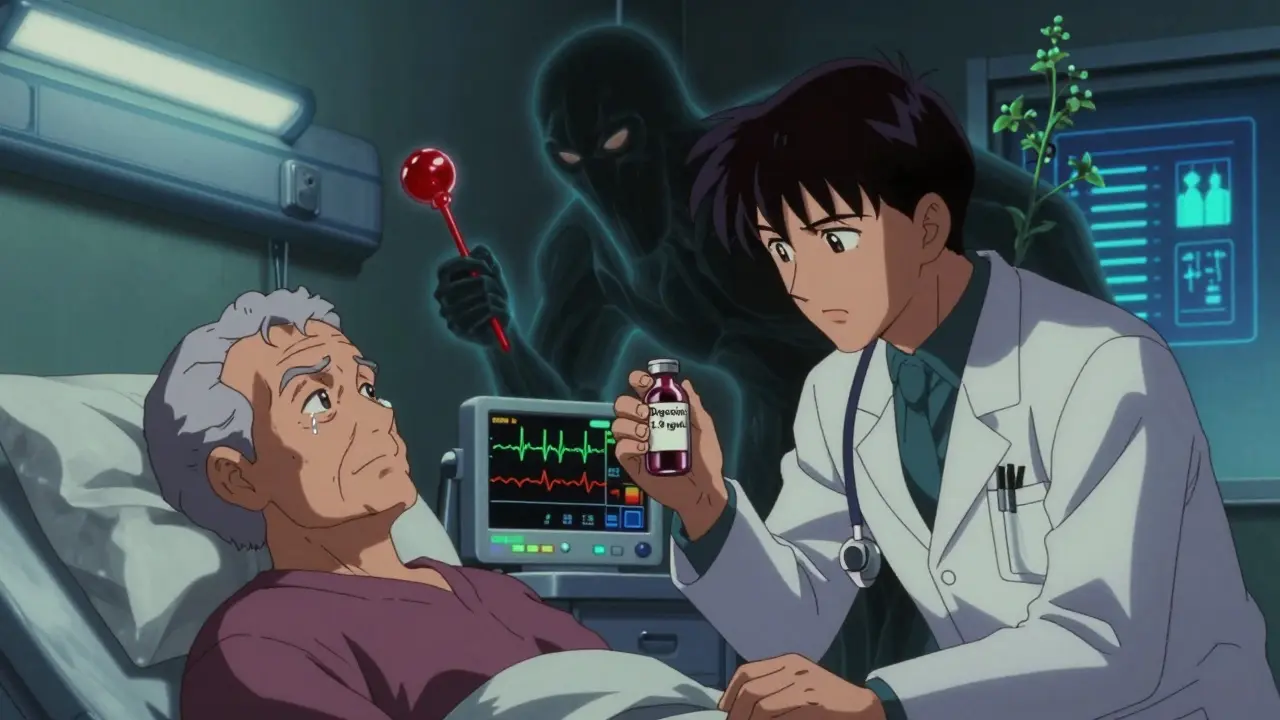
Why Digoxin Is Tricky
Digoxin doesn’t need a high dose to work. In fact, too much can be deadly. The safe range is tiny: between 0.5 and 0.9 nanograms per milliliter in your blood. Go above 2.0, and your risk of serious side effects - like dangerous heart rhythms, nausea, vision changes, or even cardiac arrest - jumps sharply. That’s why doctors call it a drug with a narrow therapeutic index. One small change in how your body handles it, and you’re out of that safe zone.
It’s also not broken down the same way in everyone. Your kidneys clear most of it. So if you have even mild kidney trouble - which is common in older adults with heart disease - digoxin builds up. Age over 65, low body weight, or a creatinine clearance below 50 mL/min? You’re already at higher risk. Add in the wrong medication or food, and you’re playing with fire.
Medications That Can Raise Digoxin Levels
Some drugs make your body hold onto digoxin longer, pushing levels into the danger zone. The biggest offenders:
- Dronedarone (used for atrial fibrillation): This one’s especially dangerous. Studies show it can spike digoxin levels by more than 50%. The 2012 PALLAS trial found patients on both drugs had a 2.5 times higher risk of sudden death. If you’re prescribed dronedarone, your digoxin dose must be cut in half - and your blood levels checked weekly for at least two weeks.
- Verapamil and diltiazem (calcium channel blockers): These are common for high blood pressure and chest pain. But together with digoxin, they can cause your heart rate to drop below 40 beats per minute. That’s not just slow - it’s life-threatening.
- Amiodarone: Another antiarrhythmic. One patient on Reddit described how their digoxin level jumped from 0.8 to 1.9 ng/mL within two weeks of starting amiodarone. They ended up with blurred vision and constant nausea. Their doctor had to slash the digoxin dose by half.
- Erythromycin and tetracycline: These antibiotics aren’t just for infections. They change the gut bacteria that normally break down digoxin. Result? Up to a 40% increase in digoxin concentration.
- Quinidine: Rarely used now, but still around. It can double digoxin levels by blocking kidney clearance.
Even carvedilol, a beta-blocker many heart patients take, can bump digoxin levels by about 16%. It’s not as dramatic as dronedarone, but it’s enough to matter - especially if you’re already near the top of the safe range.
Medications That Can Lower Digoxin Levels
Not all interactions make digoxin stronger. Some make it weaker - and that’s dangerous too. If your levels drop below 0.5 ng/mL, the drug stops working. You might feel your heart racing again, or your swelling come back.
- St. John’s wort: This popular herbal supplement for depression activates a protein called P-glycoprotein that flushes digoxin out of your body. Studies show it can drop digoxin levels by 25%. If you’re taking it, your heart failure symptoms could return - even if you’re taking your pill every day.
- Rifampin: An antibiotic used for tuberculosis. It speeds up how fast your liver clears digoxin. Levels can drop by 35-45%. This isn’t just a theory - it’s been documented in hospital cases where patients lost symptom control after starting rifampin.
- Thyroid medications: If you’re on levothyroxine for hypothyroidism, it can increase how fast your body breaks down digoxin. That’s why your doctor should check your digoxin level after adjusting your thyroid dose.
Food, Supplements, and Lifestyle Traps
Digoxin doesn’t just interact with pills. Your diet can mess with it too.
- High-fiber foods: Oatmeal, bran, whole grains - all of them can reduce digoxin absorption by 20-25%. One patient on Mayo Clinic’s forum said their levels stayed low until they stopped eating oatmeal with their pill. They now take digoxin two hours before breakfast. Simple fix. Big difference.
- Black licorice: Yes, really. The glycyrrhizin in licorice causes your body to lose potassium. Low potassium + digoxin = a recipe for deadly heart rhythms. The Heart and Stroke Foundation of Canada warns patients to avoid it entirely. Even a few pieces a week can be risky.
- Antacids: Those Tums or Maalox you take for heartburn? They contain aluminum or magnesium. Studies show they can cut digoxin absorption by up to 30%. If you need an antacid, take it at least four hours after your digoxin.
- Psyllium fiber supplements: Metamucil, Konsyl - these can knock digoxin absorption down by 30-40% if taken within two hours. Same rule: space them out.
- Hawthorn: Often sold as a natural heart remedy. But it can prolong your QT interval, just like digoxin. Together, they raise the risk of torsades de pointes - a chaotic, life-threatening rhythm.
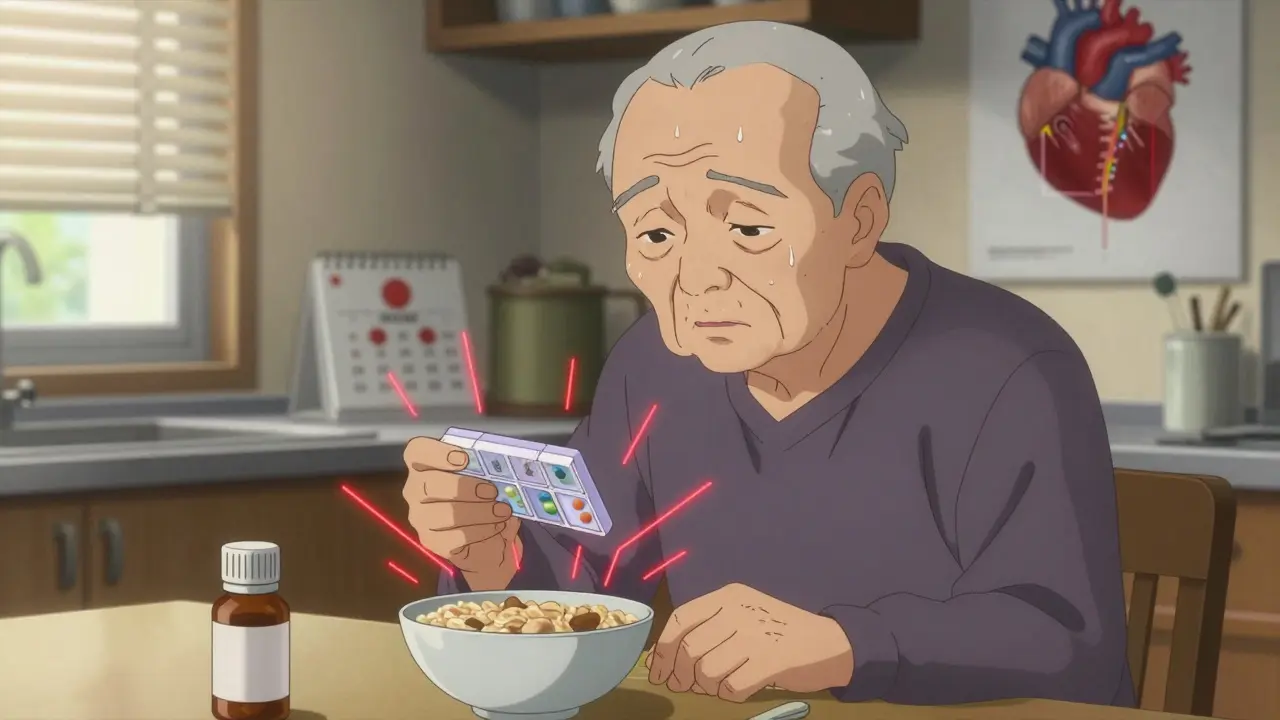
What You Need to Monitor
Monitoring isn’t optional. It’s your safety net.
- Check your potassium: Hypokalemia (low potassium) is one of the top triggers for digoxin toxicity. Keep it above 4.0 mmol/L. Diuretics like furosemide or hydrochlorothiazide can drain potassium fast. Your doctor should test your levels at least once a month.
- Track your digoxin blood level: If you’re stable, get tested every 3-6 months. But if you start a new drug, change your dose, or have kidney issues, get tested weekly until things settle.
- Watch for symptoms: Nausea, vomiting, loss of appetite, blurred vision, yellow-green halos around lights, confusion, or an unusually slow heartbeat? Don’t wait. Call your doctor. These aren’t just side effects - they’re red flags.
- Use a pill organizer: Digoxin works best when taken at the same time every day. Missing a dose or doubling up can throw off your levels.
The American College of Cardiology now has a simple risk score for digoxin toxicity. If you’re over 75, have low potassium, poor kidney function, take more than 0.25 mg daily, or are on verapamil or amiodarone - you’re at high risk. If your score is 5 or higher, you need weekly blood tests until things stabilize.

What to Do If You’re on Digoxin
Here’s the real-world checklist:
- Take digoxin at the same time every day - preferably in the morning.
- Avoid high-fiber meals, oatmeal, and fiber supplements for at least two hours before and after your dose.
- Never take antacids within four hours of digoxin.
- Stop eating black licorice - all forms, including candy and tea.
- Tell every doctor, pharmacist, and even your dentist you’re on digoxin before they prescribe anything.
- Keep a list of all your meds and supplements - including herbal ones - and review it with your cardiologist every 3 months.
- Know your potassium level. Ask for it at every blood test.
- If you feel sick, dizzy, or see strange colors, don’t ignore it. Call your doctor immediately.
Digoxin isn’t going away. Even though newer drugs are available, it’s still used in about 12% of heart failure patients in the U.S. - and nearly a quarter of those over 80. Why? Because it works. And when used carefully, it can improve quality of life. But it’s not a drug you can take on autopilot. It demands attention, awareness, and communication.
What’s Changing in 2025
There’s new hope on the horizon. The DIG-FAST trial is testing an extended-release version of digoxin that smooths out the peaks and valleys in blood levels. Early results suggest it could reduce interaction risks by 30%. If approved, it could be available by late 2025.
Meanwhile, more hospitals are using point-of-care digoxin tests - a quick finger-prick test that gives results in under 15 minutes. That means doctors can adjust doses faster, especially in older patients who can’t wait days for lab results.
For now, though, the rules haven’t changed: know your interactions, monitor your levels, and speak up. Your heart depends on it.
Can I take digoxin with my multivitamin?
Most multivitamins are fine, but check the label. If it contains calcium, magnesium, or iron, take it at least 2 hours after your digoxin. These minerals can bind to digoxin and reduce absorption. Also avoid multivitamins with fiber or herbal extracts like St. John’s wort.
How often should I get my digoxin level checked?
If you’re stable and not starting new meds, every 3 to 6 months is standard. But if you begin a new drug, change your dose, or have kidney problems, get tested weekly for the first 2 weeks. Your doctor should also check your potassium monthly, especially if you’re on diuretics.
Is digoxin safe for elderly patients?
It can be - but only with careful monitoring. Patients over 75 are nearly 3 times more likely to experience toxicity. Kidney function declines with age, and body weight is often lower. Doctors usually start with a lower dose (0.125 mg daily) and check levels more often. Never assume a lower dose is automatically safe - interactions still apply.
Can I drink alcohol while taking digoxin?
Moderate alcohol (one drink a day) is usually okay, but heavy drinking can worsen heart failure and trigger irregular rhythms. Alcohol also dehydrates you and can lower potassium - both of which increase digoxin toxicity risk. If you drink, keep it light and talk to your doctor about your habits.
What should I do if I miss a dose of digoxin?
If you miss a dose and remember within 12 hours, take it right away. If it’s been more than 12 hours, skip it and take your next dose at the regular time. Never double up. Missing a dose won’t hurt much, but doubling up can push your levels into the toxic range.
Are there any new alternatives to digoxin?
Yes - drugs like sacubitril/valsartan (Entresto), SGLT2 inhibitors (Farxiga, Jardiance), and vericiguat are now preferred for heart failure. But digoxin still has a role - especially for patients with persistent symptoms despite these newer drugs, or those with atrial fibrillation needing rate control. It’s cheaper, too - often under $6 a month. The goal isn’t to replace it everywhere, but to use it smarter.
Can I take digoxin if I have kidney disease?
Yes, but your dose must be lowered. If your creatinine clearance is below 50 mL/min, your doctor will reduce the dose. If it’s below 15 mL/min, the European Medicines Agency recommends avoiding digoxin entirely. Always get your kidney function checked before starting and every few months after.





Rulich Pretorius
December 15, 2025 AT 06:57Digoxin is one of those drugs that feels like it belongs in a museum - ancient, effective, and dangerously easy to mess up. I’ve seen patients on it for decades, and the ones who survive are the ones who treat it like a live wire, not a pill. Kidney function, potassium, timing - skip any one of those and you’re gambling with your heartbeat.
Dwayne hiers
December 16, 2025 AT 23:16From a pharmacokinetic standpoint, digoxin’s narrow therapeutic index (NTI) is compounded by its reliance on renal excretion and P-glycoprotein-mediated efflux. Concomitant administration of P-gp inhibitors like dronedarone or amiodarone significantly reduces clearance, elevating serum concentrations beyond the therapeutic window (0.5–0.9 ng/mL). Concurrent hypokalemia further potentiates cardiotoxicity via enhanced myocyte binding. Routine TDM is non-negotiable.
Sarthak Jain
December 17, 2025 AT 04:05bro i was on digoxin for afib and my doc never told me about the oatmeal thing. i ate it every morning with my pill. one day i started seeing yellow rings around lights and thought i was going crazy. turned out my level was 1.8. they cut my dose in half and told me to take it 2 hours before breakfast. life changed. also no licorice. ever.
Edward Stevens
December 17, 2025 AT 14:57So let me get this straight. You’re telling me the same drug that’s been around since 1785 is still the go-to for heart failure because… it’s cheap? And we’re just hoping people don’t eat fiber or drink tea or take a Tums? This isn’t medicine. This is a survival game with a 19th-century rulebook.
Daniel Thompson
December 19, 2025 AT 07:08I’ve been on digoxin for 11 years. I take it at 7 a.m. sharp. I never eat breakfast until 9:30. I avoid all antacids. I get my potassium checked every 28 days. I have a printed list of every drug I’ve ever taken, signed by my cardiologist. If you’re not this meticulous, you shouldn’t be on it. This isn’t a suggestion - it’s a requirement for staying alive.
Alexis Wright
December 21, 2025 AT 06:19Let’s be honest - digoxin is a relic that should’ve been buried with penicillin. It’s like giving a toddler a loaded pistol and saying "be careful." The fact that 12% of heart failure patients are still on this is a indictment of modern cardiology. We have ENTRESTO, SGLT2 inhibitors, vericiguat - all proven to reduce mortality - and we’re still clinging to a drug that requires a PhD in pharmacokinetics just to not die? Pathetic.
Rich Robertson
December 22, 2025 AT 17:15In India, we call digoxin "the silent heartkeeper." Older folks take it without knowing half the risks - they trust their doctor, their pharmacy, their grandmother’s advice. I’ve seen patients on it for 20 years, never checked a level, and still feel fine. But when they start on an antibiotic or switch to a different brand of multivitamin? Boom. ER visit. The system fails them because no one explains it in language they understand. This post? This is the kind of clarity that saves lives.
Thomas Anderson
December 22, 2025 AT 23:07Just take it at the same time every day. Don’t eat fiber for 2 hours before or after. No licorice. Tell every doctor you’re on it. Check your potassium. That’s it. You don’t need to be a scientist. Just be consistent and speak up. Simple stuff, but most people skip it. Don’t be most people.
Tim Bartik
December 24, 2025 AT 01:40So let me get this straight - the FDA lets this dinosaur drug stay on the market because it’s cheap? Meanwhile, some pharma bro is making millions on a new pill that does the same damn thing? And we’re supposed to be grateful because it’s under $6 a month? This ain’t healthcare. This is corporate greed wrapped in a white coat.
Natalie Koeber
December 25, 2025 AT 04:02They don’t want you to know this - but digoxin is a tool used to control the elderly population. The real reason it’s still around? Because it makes people dependent. Watch your labs. Watch your meds. Watch your food. They want you scared, doc-dependent, and obedient. That’s why they don’t push the new drugs - they’re too expensive for the system. This isn’t medicine. It’s control.
Wade Mercer
December 25, 2025 AT 13:57If you’re taking digoxin and you’re not monitoring your levels religiously, you’re not just risking your life - you’re being irresponsible to everyone who loves you. Your family shouldn’t have to bury you because you took a Tums with your pill. This isn’t a suggestion. It’s a moral obligation.
Jonny Moran
December 26, 2025 AT 22:23My mom’s been on digoxin for 15 years. She’s 82. She takes it at 8 a.m., eats oatmeal at 10, and never misses a potassium test. She doesn’t know the science - but she knows the rules. And she’s still here. It’s not magic. It’s discipline. You don’t need to be a genius. You just need to be consistent.
Sinéad Griffin
December 27, 2025 AT 06:48NO LICORICE. EVER. 🚫🍬 I had a friend who ate black licorice candy every day because "it’s natural." She ended up in the ICU with torsades. They had to shock her twice. Don’t be her. Don’t be stupid. Your heart isn’t a snack.
jeremy carroll
December 27, 2025 AT 11:44hey i was scared to even ask my doc about digoxin because i thought i’d sound dumb. but i wrote down all my meds and questions and brought it in. he was like "this is why you’re still alive." you don’t have to be perfect. just show up and care. that’s enough.
Daniel Wevik
December 28, 2025 AT 10:34Extended-release digoxin in 2025? Finally. The current formulation is a pharmacokinetic nightmare - peaks, valleys, interactions galore. The DIG-FAST trial’s early data is promising. Smoother levels mean fewer ER visits, fewer deaths. This isn’t innovation for profit - it’s innovation for survival. Let’s hope the FDA doesn’t drag its feet.