Rescue Inhaler Comparison Tool
Select Medications to Compare
Quick Medication Facts
| Medication | Onset Time | Duration | Common Side Effects |
|---|
Quick snapshot
- Albuterol inhaler (Salbutamol): fast‑acting SABA, works in 5‑15min, lasts 4‑6h.
- Levalbuterol inhaler: stereoisomer of albuterol, slightly fewer heart‑beat side effects.
- Ipratropium inhaler: anticholinergic bronchodilator, works slower but adds extra relief for COPD.
- Montelukast (tablet): leukotriene receptor antagonist, not a rescue inhaler but useful for prevention.
- Theophylline (oral): old‑school bronchodilator, requires blood‑level monitoring.
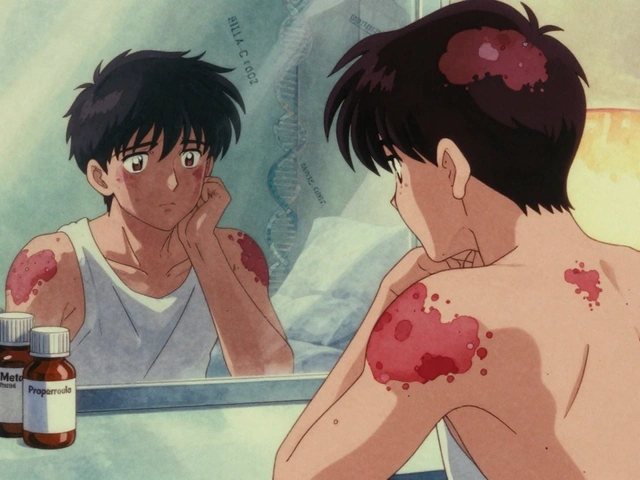
Albuterol inhaler is a short‑acting β2‑agonist (SABA) medication, known internationally as Salbutamol, that relaxes airway smooth muscle to quickly relieve asthma or COPD symptoms.
How albuterol works
When you press the canister, albuterol molecules bind to β2‑adrenergic receptors on bronchial smooth muscle. This triggers a cascade that increases cyclic AMP, causing the muscle to relax. The result is a rapid widening of the airway, usually noticeable within minutes. Because it targets receptors directly, the effect peaks fast and fades within a handful of hours, making it ideal for sudden wheezing or breathlessness.
Key attributes of the albuterol inhaler
- Onset: 5-15minutes
- Peak effect: 30-60minutes
- Duration: 4-6hours
- Typical dose: 90‑100µg per puff; 1-2 puffs as needed
- Common side effects: trembling, tachycardia, mild headache
- Prescription status: prescription‑only in most countries, over‑the‑counter in some regions
Popular alternatives
Not every patient tolerates albuterol or needs a SABA. Below are the most frequently prescribed options, each with its own strengths and drawbacks.
Levalbuterol inhaler is a single‑enantiomer form of albuterol that delivers the same bronchodilation with a slightly lower incidence of heart‑related side effects.
Ipratropium inhaler is a short‑acting anticholinergic bronchodilator that blocks muscarinic receptors, making it especially helpful for COPD patients who need additional airway opening.
Montelukast is a leukotriene receptor antagonist taken as a tablet; it does not provide immediate relief but reduces inflammation and can cut down the frequency of rescue inhaler use.
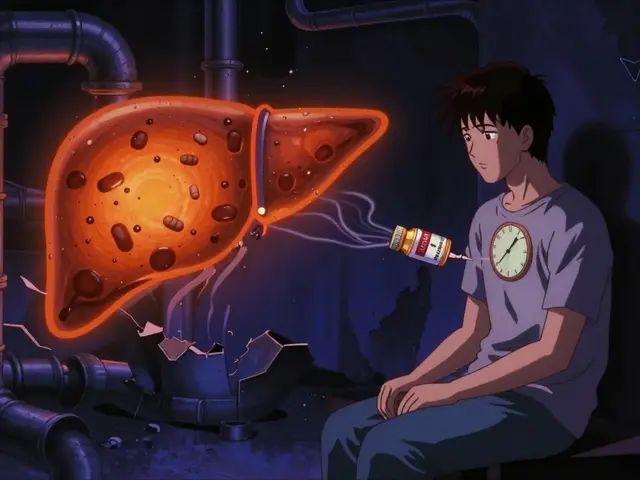
Theophylline is an older oral bronchodilator that works by inhibiting phosphodiesterase, requiring regular blood‑level checks to stay within a therapeutic window.
Omalizumab is a monoclonal antibody that binds IgE, used for severe allergic asthma; it’s not a rescue drug but can dramatically lower the need for inhalers.
Side‑by‑side comparison
| Medication | Onset | Duration | Dose Frequency | Typical Cost (US$ per month) | Prescription? |
|---|---|---|---|---|---|
| Albuterol | 5‑15min | 4‑6h | As needed (≤6puffs/day) | ≈20‑35 | Yes |
| Levalbuterol | 5‑15min | 4‑6h | As needed (≤6puffs/day) | ≈30‑45 | Yes |
| Ipratropium | 15‑30min | 4‑6h | Every 4‑6h | ≈25‑40 | Yes |
| Montelukast | 4‑6h (indirect) | 24h | Once daily | ≈15‑30 | Yes |
| Theophylline | 30‑60min | 6‑12h | 2‑3×/day (blood‑level monitoring) | ≈10‑20 | Yes |

Choosing the right rescue medication
Think of your airway needs as a toolbox. If you need instant relief, a SABA like albuterol or levalbuterol is the go‑to. If you have a mixed asthma‑COPD picture, adding ipratropium can give extra opening power because it works via a different pathway (muscarinic blockade). For people who experience frequent tremor or palpitations from albuterol, levalbuterol’s cleaner side‑effect profile may be preferable.
When cost is a major factor, generic albuterol is usually the cheapest, but insurance formularies sometimes push patients toward branded levalbuterol or combination inhalers. Oral options such as montelukast or theophylline are useful when inhaler technique is a barrier-think elderly patients who struggle with metered‑dose inhalers (MDIs) or dry‑powder inhalers (DPIs). However, these oral agents don’t replace a rescue inhaler; they’re adjuncts that reduce the frequency of attacks.
Practical tips for safe inhaler use
- Technique matters: Shake the canister, exhale fully, then press while inhaling slowly. Hold breath for 10seconds before exhaling.
- Storage: Keep inhalers at room temperature, away from direct heat. A canister can lose potency after 12months of use.
- Spacer use: Adding a spacer reduces oropharyngeal deposition, easing throat irritation, especially for kids.
- Tracking usage: Most modern inhalers have dose counters; if yours doesn’t, mark a calendar to avoid running out during an attack.
- Insurance navigation: Check formulary tiers; generic albuterol often sits on Tier1, while levalbuterol may be Tier2 or higher.
Related concepts you’ll run into
Understanding albuterol’s place in therapy is easier when you see the bigger picture. Asthma is a chronic inflammatory disease that typically requires a combination of controller (e.g., inhaled corticosteroids) and rescue (e.g., SABAs) medications. COPD (chronic obstructive pulmonary disease) often needs both a SABA and an anticholinergic like ipratropium for optimal relief.
Another key term is Bronchodilator, a broad class that includes SABAs, long‑acting β2‑agonists (LABAs), and anticholinergics. Knowing whether a drug is short‑acting or long‑acting guides how often you can safely use it. Inhaler device type also matters-MDIs deliver medication via a propellant spray, while DPIs rely on the patient’s own inhalation flow. Some patients have a preference because of ease of use or portability.
Bottom line
If you need rapid relief from sudden wheezing, the albuterol inhaler remains the gold standard. It’s cheap, fast, and widely available. For those who experience side effects, levalbuterol offers a smoother ride. Adding an anticholinergic like ipratropium gives extra coverage for COPD or severe asthma attacks, while oral agents such as montelukast or theophylline serve as adjuncts that may lower overall inhaler reliance. The best choice always balances speed of action, side‑effect tolerance, insurance cost, and personal inhaler technique.
Frequently Asked Questions
Can I use albuterol and levalbuterol together?
Mixing two SABAs isn’t recommended because they act on the same receptors, offering no extra benefit and increasing the risk of tachycardia. If albuterol isn’t tolerable, switch to levalbuterol under doctor supervision.
Why does my inhaler feel empty before the dose counter hits zero?
Spray canisters can lose pressure over time, especially if stored in heat. Even with a few doses left, the aerosol may be weak, making it feel empty. Replace the inhaler if you notice a drastic drop in force.
Is ipratropium suitable for children with asthma?
Ipratropium is approved for children 6years and older, mainly for COPD‑like symptoms. For pure asthma, SABAs remain first‑line; ipratropium is added only when a child’s asthma overlaps with COPD features.
How often can I safely use my albuterol inhaler?
Most guidelines say no more than 6puffs (usually 2puffs per dose) in 24hours. Exceeding this signals poorly controlled asthma and warrants a doctor visit.
What are the main side effects of theophylline?
Theophylline can cause nausea, insomnia, and narrow‑range cardiac arrhythmias if blood levels get too high. Regular blood monitoring keeps it within a therapeutic window (10‑20µg/mL).




Chris Fulmer
September 25, 2025 AT 17:29I've been digging through the albuterol guide and it's clear how fast it works, but the side‑effect profile can be a bit of a trade‑off for some patients. When you compare it side‑by‑side with levalbuterol, the onset is identical while the heart‑racing tremor tends to be milder with levalbuterol. For COPD folks, adding ipratropium gives that extra bronchodilation boost because it targets a different receptor pathway. It's also worth noting that generic albuterol stays the cheapest option in most formularies, so insurance cost can be a deciding factor. Overall, the choice often balances speed, side effects, and your personal inhaler technique.
William Pitt
October 5, 2025 AT 06:39Great summary, but remember to check your spacer technique!
Jeff Hershberger
October 14, 2025 AT 19:49The article paints albuterol as the superhero of bronchodilators, swooping in within minutes to vanquish wheeze. Yet, lurking behind that cape are tremors and a racing heart that can make you feel like a jittery squirrel.
Jesse Najarro
October 24, 2025 AT 08:59Spot on, the side‑effects can feel like an unwanted side‑kick, especially for patients sensitive to tachycardia. Pairing it with a low‑dose steroid can sometimes smooth out the ride.
Dan Dawson
November 2, 2025 AT 21:09Albuterol’s quick onset makes it a go‑to for sudden attacks, but keep an eye on usage limits to avoid over‑reliance.
Lawrence Jones II
November 12, 2025 AT 10:19Indeed, the pharmacodynamics of albuterol involve β2‑adrenergic receptor agonism, leading to increased cAMP and smooth‑muscle relaxation 😊. For patients on multiple inhalers, checking compatibility is key 🚀.
Robert Frith
November 21, 2025 AT 23:29Listen up lads, this albuterol stuff is the real deal, not some foreign fancy‑pills they push overseas. If you want proper relief, stick with the tried‑and‑true SABA, no nonsense.
Albert Gesierich
December 1, 2025 AT 12:39While the guide is generally accurate, there are several grammatical inconsistencies that need correction: “its” should be “it’s” in the sentence about inhaler technique, and “you” should be capitalized at the start of a new sentence. Moreover, the dosage recommendations must adhere to the latest GINA guidelines, which explicitly limit albuterol to a maximum of six puffs per 24‑hour period.
Brad Tollefson
December 11, 2025 AT 01:49The spacing tip is solid, but remember to replace your inhaler before the canister gets too cold; low temperature can affect the spray force.
Paul van de Runstraat
December 20, 2025 AT 14:59Oh sure, because reading a table about onset times is exactly what my grandma needs before she fumbles with her spacer-thanks for the riveting data, really.
Suraj Midya
December 30, 2025 AT 04:09Honestly this guide ignores the fact that many of our local pharmacies overcharge for levalbuterol, pushing people to stick with the cheap albuterol even when they might benefit from the cleaner side‑effect profile.
ashish ghone
January 8, 2026 AT 17:19It's great that the guide highlights the rapid onset of albuterol, because in acute asthma attacks every minute counts.
However, many patients forget that proper inhaler technique can dramatically affect drug delivery, especially if they skip the breath‑hold step.
Using a spacer not only reduces oropharyngeal deposition but also lessens the tremor some experience with high‑dose puffs.
For those concerned about tachycardia, switching to levalbuterol can be a sensible compromise, as clinical studies show a modest reduction in heart‑rate spikes.
In COPD management, adding ipratropium provides an anticholinergic pathway that synergizes with SABAs, offering broader bronchodilation.
Cost considerations are also vital; while generic albuterol is often Tier 1, insurance formularies sometimes steer patients toward pricier branded options.
Monitoring usage patterns through dose counters or smartphone apps can alert clinicians when a patient's rescue inhaler use is creeping up, indicating poor control.
Moreover, educating patients about the maximum of six puffs per day is essential to prevent overuse and potential side‑effects.
Theophylline, though older, still has a place for patients who struggle with inhaler technique, but it requires regular serum level checks.
Montelukast, being a leukotriene receptor antagonist, doesn't provide immediate relief but can reduce overall exacerbation frequency, complementing rescue inhalers.
Remember to store inhalers at room temperature; exposure to extreme heat can degrade the propellant and reduce efficacy.
If an inhaler feels weak before the dose counter reaches zero, it's usually a sign of pressure loss, and a replacement should be obtained promptly.
For children, using age‑appropriate devices like valved holding chambers can improve drug deposition and ease of use.
Lastly, consistency in follow‑up appointments allows healthcare providers to tailor the rescue regimen based on real‑world usage data.
In summary, a balanced approach that considers onset speed, side‑effect profile, cost, and patient technique will yield the best outcomes for both asthma and COPD sufferers.
steph carr
January 18, 2026 AT 06:29Thanks for the thorough rundown; it's reassuring to see both the fast-acting options and the longer-term strategies laid out clearly.
Vera Barnwell
January 27, 2026 AT 19:39Honestly, some of the “official” side‑effect stats are probably downplayed to keep pharmaceutical profits soaring.