When a pill turns yellow, a cream separates into layers, or a liquid smells off, it’s not just old-it could be dangerous. Expired drugs don’t just lose effectiveness; they can physically break down in ways that make them unsafe to use. You don’t need a lab to spot these changes. With a little knowledge and careful observation, you can tell if a medication has gone bad before you take it.
What to Look for in Expired Medications
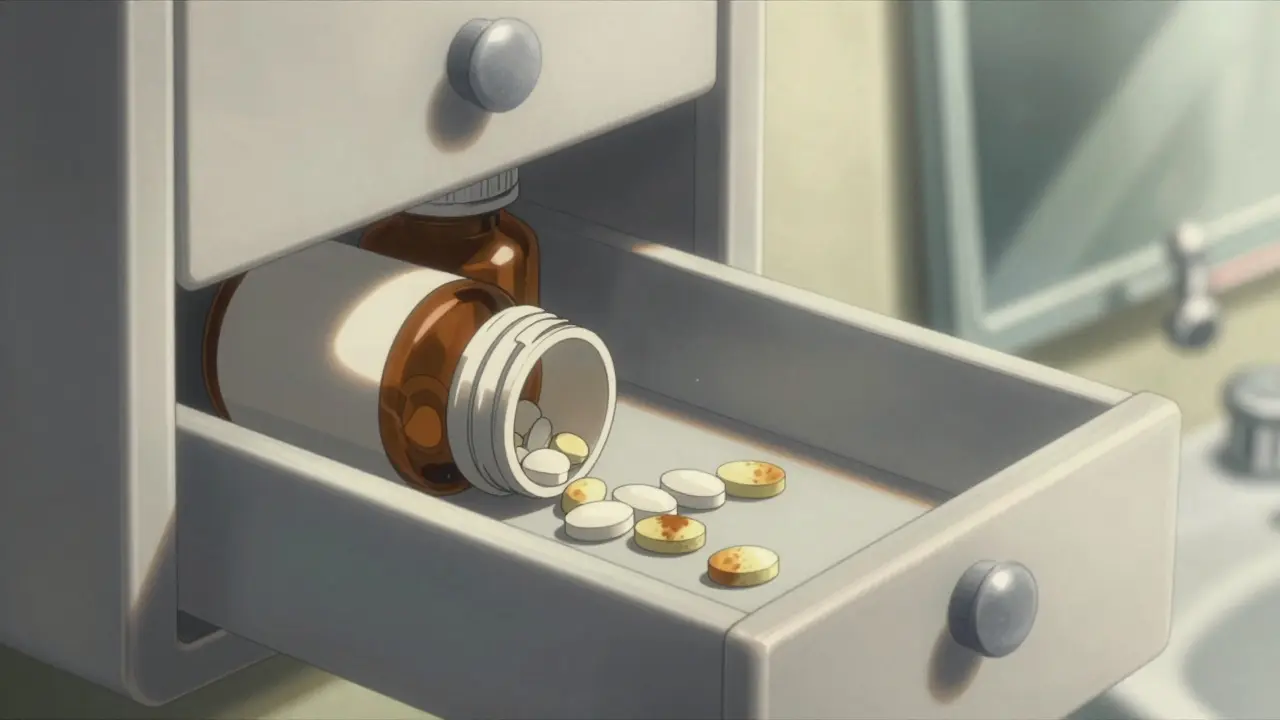
The most common sign that a drug has degraded is a change in color. Tablets and capsules that were once white or off-white may turn yellow, brown, or even develop dark spots. Antibiotics like tetracycline are especially prone to this-they often darken from pale yellow to deep brown as they break down. If you see any discoloration that wasn’t there before, don’t risk it.
Liquids are just as telling. Clear solutions like eye drops or cough syrup that turn cloudy or develop floating particles are a red flag. The U.S. Pharmacopeia (USP) sets strict limits on particles in liquids: more than 6,000 particles larger than 10 micrometers per container means the product is no longer safe. You don’t need a microscope to see this. Hold the bottle up to a bright light. If you notice specks, strings, or haze, throw it out.
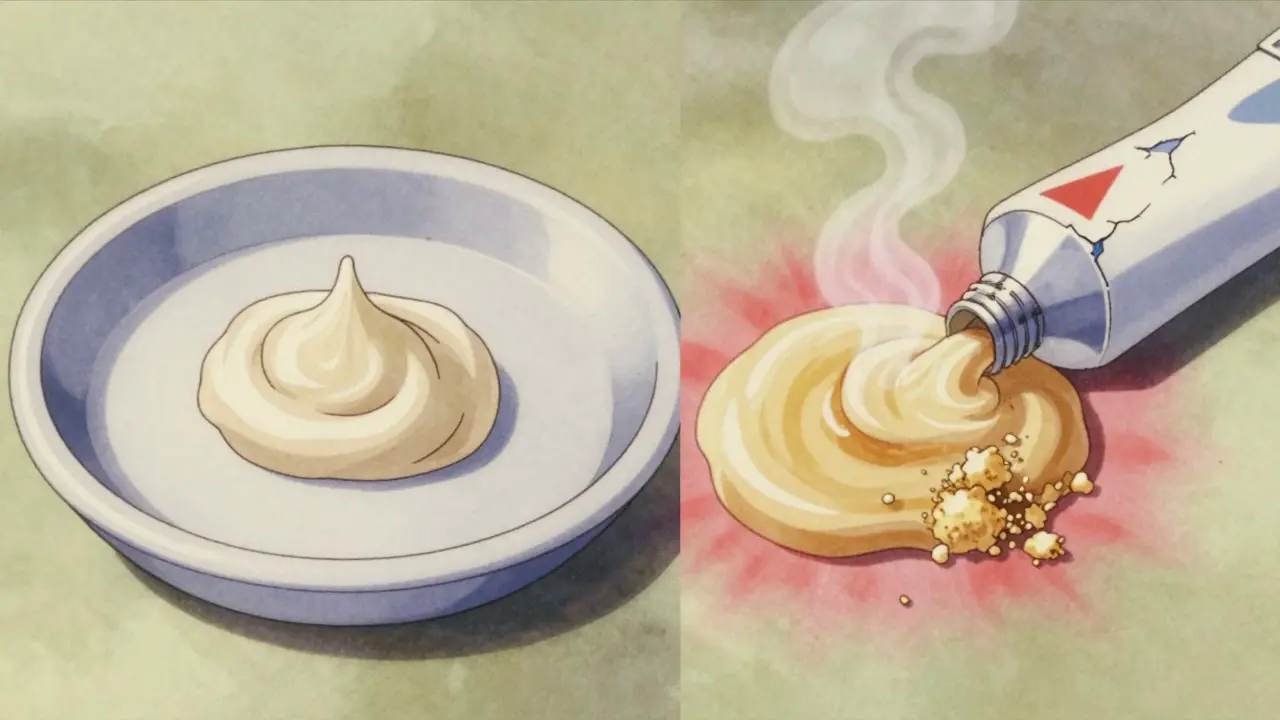
Creams and ointments can separate into oily and watery layers. This is called phase separation. If you squeeze out a dollop and it looks like oil floating on top of a watery gel, or if it’s become grainy or hard instead of smooth, it’s degraded. Ciprofloxacin ointment, for example, has been shown to liquefy after just 880 days past its expiration date. That’s not normal-it’s a sign the formulation has broken down.
Smell and Texture Tell the Real Story
Odor is another strong indicator. Most medications have little to no smell. If your pills or capsules suddenly smell rancid, sour, or like chemicals, that’s not normal. Amoxicillin capsules, for instance, are known to absorb moisture from the air. When they do, they can develop a musty or moldy odor. That’s not just unpleasant-it means the drug has likely started to degrade chemically.
Texture changes are often missed. Tablets that crumble easily, capsules that feel sticky or brittle, or powders that clump together are all signs of moisture damage. A tablet that used to be hard and smooth now feels soft or powdery? That’s a problem. The ideal hardness for most immediate-release tablets is between 4 and 10 kiloponds. If you can crush one between your fingers, it’s no longer stable.
For liquid medications, check the consistency. If a syrup that used to be thick now flows too easily, or if an injection feels thinner than it should, the active ingredient may have broken down. This isn’t just about potency-it’s about safety. Degraded drugs can cause unexpected side effects or allergic reactions.
Why These Changes Happen
Drugs break down because of heat, humidity, light, and time. Even if the bottle says “store at room temperature,” that doesn’t mean your bathroom cabinet is safe. Humidity levels above 60% can cause tablets to absorb moisture and swell. Temperatures above 25°C (77°F) can speed up degradation by more than twice as fast.
Some drugs are more sensitive than others. Light-sensitive medications like nitroglycerin or tetracycline degrade quickly when exposed to sunlight-even through clear bottles. That’s why they often come in dark glass or opaque packaging. If the original packaging is damaged or the bottle was left on a windowsill, the drug inside may be compromised-even if it’s not expired yet.
Manufacturers test drugs under controlled conditions to determine their expiration date. But real-world storage? That’s a different story. A study by NASA found that 68.3% of expired medications showed visible discoloration. That’s more than two out of three. And in some cases, like PMZ injections, the drug became unsafe long before any color change was visible. That’s why you can’t rely on expiration dates alone.

What You Shouldn’t Rely On
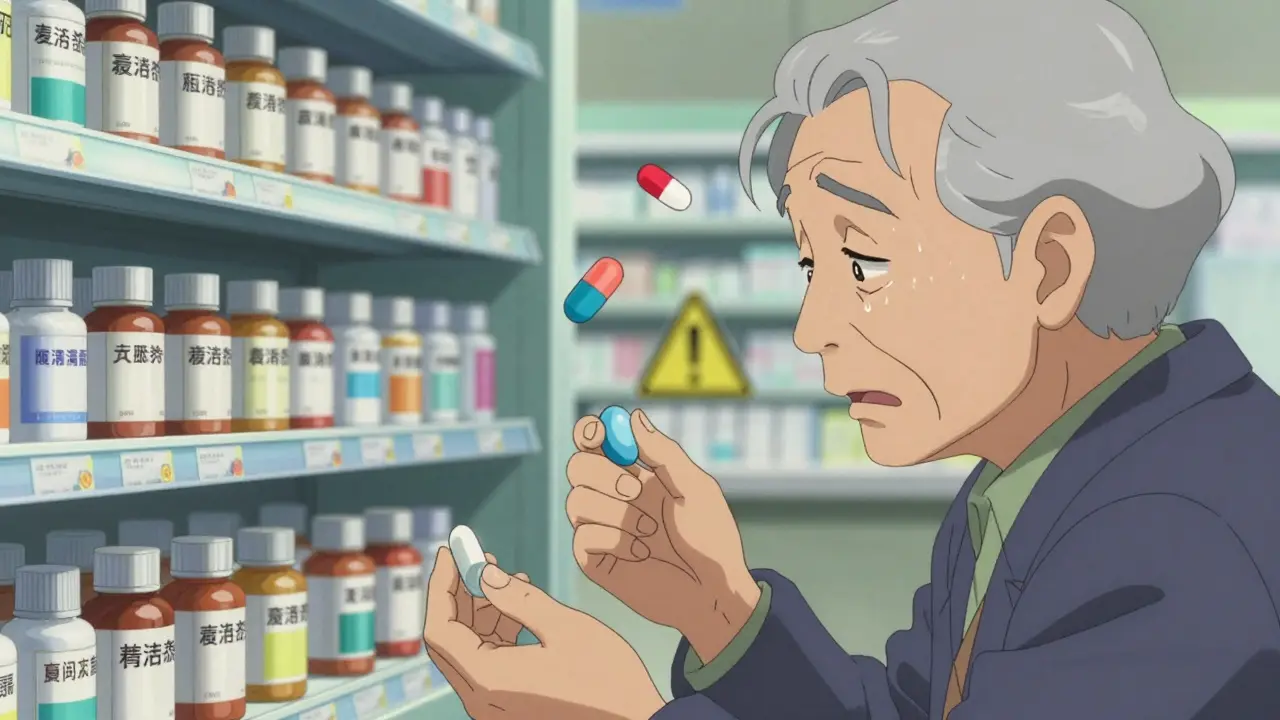
Just because a pill looks fine doesn’t mean it’s safe. The National Institute of Justice found that human visual assessment of drug color is only 65.2% accurate compared to instruments. That means nearly one in three times, you’ll miss a change. Some drugs, like aspirin, can turn slightly yellow without losing potency. Others, like insulin or epinephrine, can look perfectly clear but lose effectiveness rapidly.
Don’t assume that if it’s still in the original packaging, it’s good. Blister packs can leak. Bottles can be left open. Pills can be exposed to moisture from your hands. Even if the bottle says “keep tightly closed,” if the cap was loose for months, the drug inside may be ruined.
Also, don’t trust online forums or anecdotal advice. Reddit users report seeing “brown spots on white pills” and wondering if it’s safe. The answer is almost always no. What looks like a manufacturing flaw might actually be chemical breakdown. And what looks like normal aging might be a sign of dangerous degradation.
How to Check Your Medications Properly
Here’s how to do a proper visual check:
- Work in good lighting-natural daylight or a 500-lux lamp is ideal.
- Place the medication on a clean white surface to see color changes clearly.
- For tablets and capsules: look for discoloration, cracking, or crumbling. Compare to a new bottle if possible.
- For creams and ointments: squeeze out a small amount. Is it smooth? Or separated? Does it smell off?
- For liquids: hold it up to the light. Look for cloudiness, particles, or sediment. Shake gently-does it stay clear?
- Check the smell. If it smells unusual, discard it.
Some pharmacies and hospitals use color charts like the Munsell system to standardize assessments. You don’t need one at home, but if you’re unsure, take a photo and compare it to the manufacturer’s reference image. Many drug manufacturers now provide degradation examples on their websites.
What to Do When You Find a Problem
If you spot any of these changes, stop using the medication immediately. Don’t flush it down the toilet or throw it in the trash. Many communities have drug take-back programs. Pharmacies often accept expired medications for safe disposal. The FDA recommends using a drug disposal bag or mixing pills with coffee grounds or cat litter before throwing them away to prevent accidental ingestion.
If you’ve already taken a degraded drug and feel unwell-nausea, dizziness, rash, or unusual symptoms-seek medical help right away. Degraded antibiotics can cause allergic reactions. Degraded heart medications can fail when you need them most.
When to Replace Expired Drugs
Some medications are more critical than others. Never use expired insulin, epinephrine, nitroglycerin, or seizure medications. Even a small drop in potency can be life-threatening. For pain relievers or antihistamines, the risk is lower-but still not zero. A study by the FDA showed that 86% of expired drugs retained at least 90% potency. But that’s an average. Some dropped below 70%.
If you rely on a medication daily, replace it before it expires. Don’t wait until the last month. Store medications in a cool, dry place-like a bedroom drawer, not the bathroom. Keep them in their original containers with the label intact. That way, you can always check the expiration date and batch number.
The Bigger Picture
The global pharmaceutical stability testing market is worth over $3 billion. Hospitals, labs, and even NASA have strict protocols for checking drug integrity. But for most people, the system relies on you-the patient-to be the first line of defense.
Regulators like the FDA and WHO emphasize that visual inspection remains the most accessible tool for spotting degraded drugs, especially in places without labs or power. That’s why learning to recognize these changes matters. It’s not just about saving money. It’s about staying safe.
Next time you reach for a bottle, take a second to look. Smell. Feel. You might just prevent a bad reaction-or worse.
Can expired drugs still be effective?
Some expired drugs may still work, but it’s unpredictable. Studies show that 86% retain at least 90% potency past their expiration date, but this varies by drug type, storage conditions, and formulation. Critical medications like insulin, epinephrine, or antibiotics should never be used past expiration-even if they look fine.
Is it safe to use a pill that changed color?
No. Discoloration is the most common sign of degradation. Pills that turn yellow, brown, or develop spots have likely undergone chemical changes that can reduce effectiveness or create harmful byproducts. Never take a discolored pill, even if it’s just one or two.
Why do some medications smell bad after expiration?
Moisture and heat cause chemical breakdown in medications. Antibiotics like amoxicillin absorb water from the air, leading to moldy or sour odors. This indicates microbial growth or decomposition of the active ingredient. A foul smell means the drug is no longer safe.
Can I tell if a cream has gone bad just by looking?
Yes. Look for separation-oil floating on top of water, or a grainy texture instead of smooth cream. If it’s dried out, cracked, or smells rancid, it’s degraded. Creams like hydrocortisone or clotrimazole often fail this way after expiration.
Should I keep expired drugs just in case?
No. Keeping expired drugs creates a false sense of security. They may not work when you need them, and using them can be dangerous. Dispose of them properly and replace them with fresh ones. Emergency situations are not the time to guess.
How should I store medications to make them last?
Keep them in a cool, dry place away from sunlight and moisture. A bedroom drawer is better than a bathroom cabinet. Always keep them in their original containers with the label. Avoid leaving them in hot cars or near windows. Temperature and humidity are the biggest enemies of drug stability.
Do all expired drugs become dangerous?
Not all become dangerous, but many can. Some degrade slowly and lose potency. Others break down into toxic compounds. Since you can’t tell which is which by sight alone, the safest rule is: if it’s expired and shows any physical change, don’t use it.
Always consult your pharmacist if you’re unsure. They can help you identify changes and safely dispose of old medications. Your health isn’t worth the risk.



Mike Rengifo
December 20, 2025 AT 07:40I once kept a bottle of amoxicillin past its date because I was too lazy to go to the pharmacy. Smelled like old bread when I opened it. Didn't take it. Best decision ever.
Isabel Rábago
December 22, 2025 AT 02:14People still keep expired meds like they’re heirlooms? This isn’t a vintage wine collection. A yellow pill isn’t "interesting," it’s a chemical time bomb. If you can’t throw something away that might kill you, you don’t deserve to be healthy.
Dev Sawner
December 23, 2025 AT 05:35According to the United States Pharmacopeial Convention, the threshold for particulate matter in parenteral solutions is 6,000 particles per container above 10 micrometers. Any deviation constitutes a violation of USP <788> standards. Visual inspection alone is insufficient for clinical-grade assurance.
William Liu
December 23, 2025 AT 15:07Good to know. I always just check the date and assume it’s fine. Guess I’ll start actually looking at the pills now. Better safe than sorry.
Dikshita Mehta
December 25, 2025 AT 08:15My grandma used to say, "If it looks wrong, it is wrong." She never took a pill past its date. She lived to 92. Maybe she knew something we forgot.
Kitt Eliz
December 26, 2025 AT 22:08STOP BEING LAZY. 🚨 Your bathroom is a HUMIDITY HELLHOLE. 🌫️ That bottle on the counter? It’s a chemical disaster waiting to happen. 🧪 Store meds in a DARK, DRY drawer like your life depends on it - because it does. 🏥 #MedSafety #DontBeAnIdiot
Alex Curran
December 27, 2025 AT 14:54Had a friend take degraded ibuprofen once. Said it gave him a weird tingling in his gums. No one believed him until he showed the pill-it was cracked and had a weird sheen. Took him to the ER. Turned out the batch had absorbed moisture and formed acetic acid derivatives. Not a joke. Always check the texture.
Ashley Bliss
December 28, 2025 AT 20:32Every time I see someone say "it’s just one pill" I want to scream. You’re not a hero for risking your liver. You’re a statistic waiting to happen. That bottle isn’t just expired-it’s a betrayal of your own body. You trusted a label. The label didn’t lie. You lied to yourself. Wake up.