Every day, pharmacists in the UK and around the world dispense millions of generic medications. They’re cheaper, widely available, and just as effective as brand-name drugs-when everything goes right. But when things go wrong, the consequences aren’t theoretical. A patient gets the wrong dose because the pill looks different. Someone stops taking their medicine because they think the new tablet isn’t the same. A nurse administers a drug twice daily instead of twice weekly because the label was misprinted. These aren’t rare mistakes. They’re systemic risks built into how generics are made, labeled, and handed out.
Why Generics Are More Prone to Errors
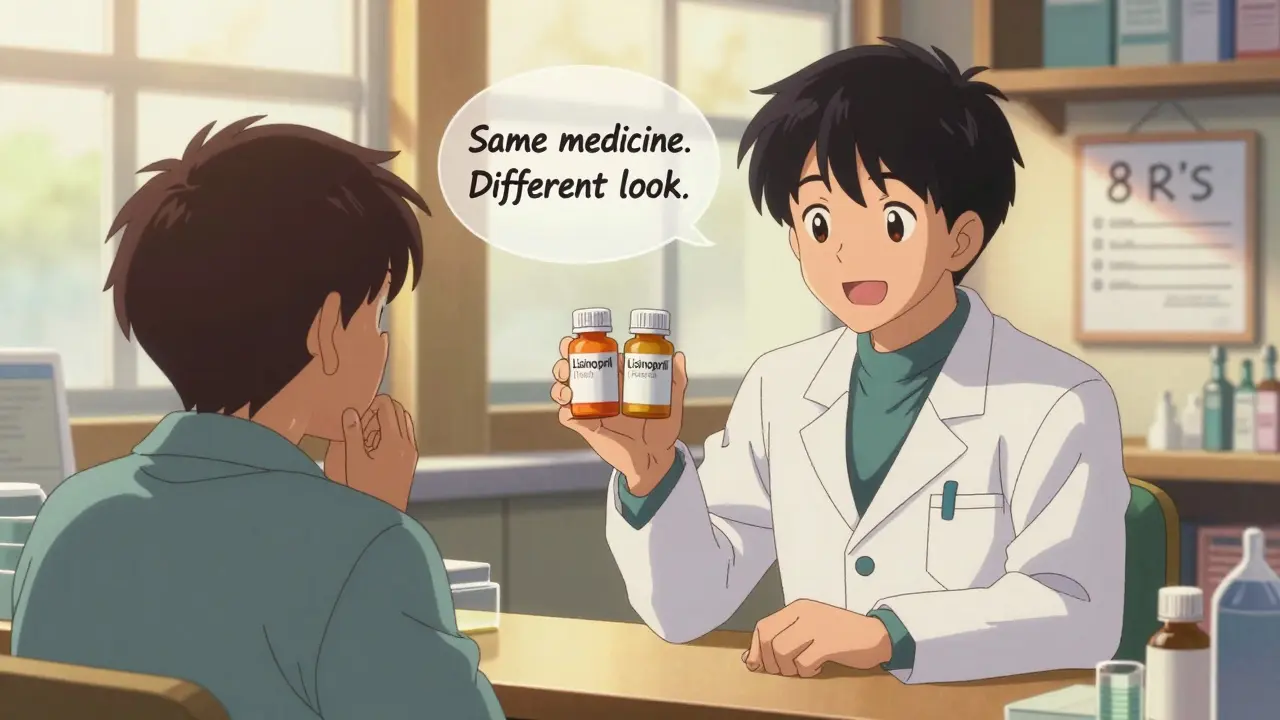
Generics aren’t just copies of brand-name drugs. They’re chemically identical in active ingredients, but they can differ in color, shape, size, taste, and even the non-active ingredients (excipients) used. That’s not a flaw-it’s legal. The FDA and MHRA allow generic manufacturers to produce the same drug with different appearances as long as the active ingredient is within 80-125% of the brand’s absorption rate. That’s a wide range. And it’s where errors start.Picture this: a patient has been taking a white, oval pill for high blood pressure for two years. One day, they pick up their refill and get a blue, round tablet. Same name on the bottle. Same dosage. But they panic. They think it’s a different drug. They skip doses. Or worse-they take both pills, thinking the new one is an extra. This happens more often than you’d think. In community pharmacies, 14.4% of all dispensing corrections are due to issues with the physical form of the medication. Generics make this worse because there are often three or four different versions of the same drug on the shelf, each from a different manufacturer.
Then there’s the naming problem. Look-alike, sound-alike (LASA) drugs are a nightmare. Take Hydralazine and Hydroxyzine. One treats high blood pressure. The other is an antihistamine. Sounds similar. Looks similar on paper. If a pharmacist misreads the script, the patient gets the wrong drug. Generics amplify this because multiple companies produce them under different brand names for the same generic compound. One pharmacy might get the generic from Actavis. Another from Teva. The bottle says the same thing-but the pill inside looks completely different.
Where Errors Happen: The Most Common Mistakes
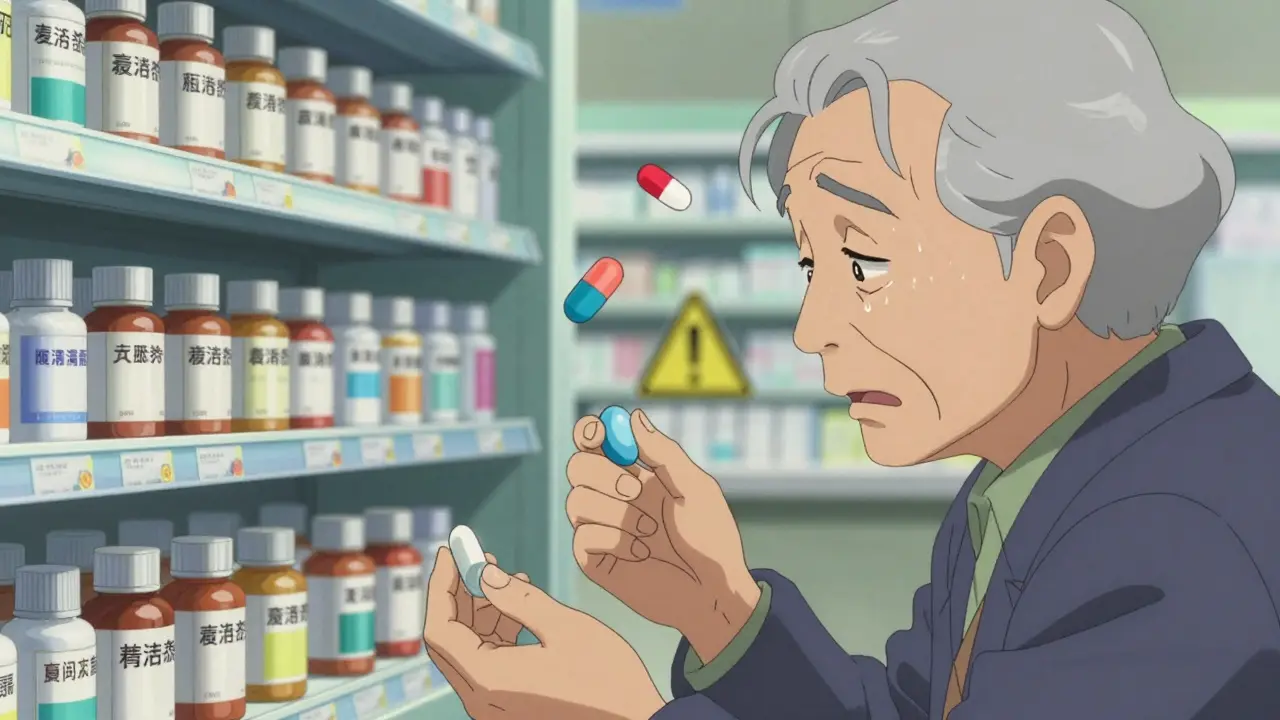
Most pharmacy errors don’t come from laziness or incompetence. They come from systems that don’t account for the complexity of generics. Here’s what goes wrong most often:- Dosage errors (37.4%): A script says “take 5 mg daily,” but the generic available is only in 10 mg tablets. The pharmacist splits it without double-checking if the patient can safely take half. Or worse-they assume the prescriber meant 10 mg.
- Strength discrepancies (19.2%): A patient’s prescription is for 20 mg of lisinopril. The pharmacy dispenses 40 mg because the label on the bottle was misread. The bottle says “Lisinopril 40 mg,” but the script says 20. The pharmacist didn’t cross-check the actual tablet.
- Dispensing form issues (14.4%): The patient’s last refill was a capsule. This time, it’s a tablet. No warning was given. The patient thinks it’s a different drug and refuses to take it.
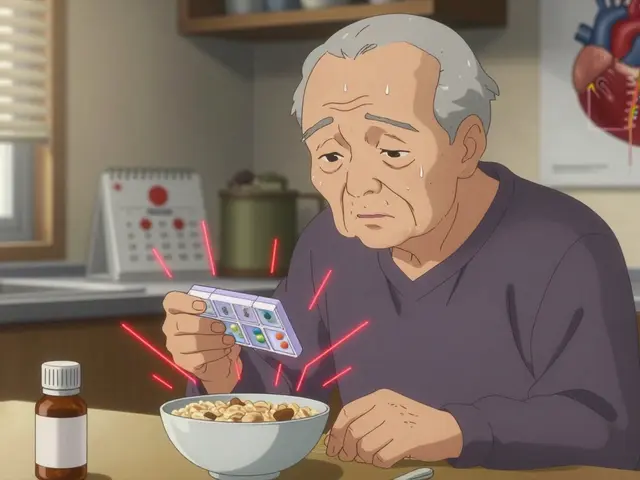
- Quantity mistakes (11.3%): A script calls for 30 tablets. The system auto-fills 90 because the pharmacy’s software defaults to a 90-day supply for generics. The patient ends up with too much-and accidentally overdoses.
- Administrative errors: Wrong patient name, wrong date, wrong prescriber. These make up nearly half of all corrections. Simple, but deadly when paired with generics.
And here’s the hidden danger: patients don’t always tell you they’re confused. They assume the pharmacist knows what they’re doing. So they take the wrong pill. Or they stop taking it. Or they go to the emergency room because they feel “different.”
Technology That Actually Works
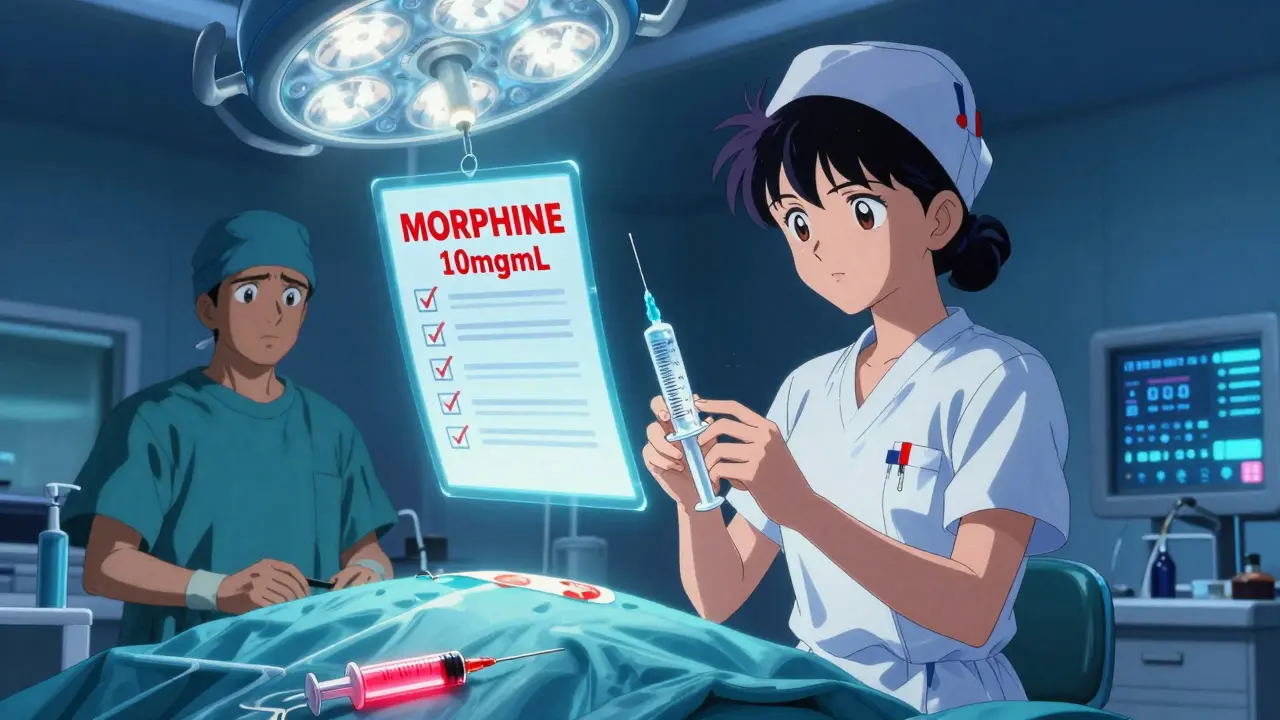
You can’t fix this with better memory or more caffeine. You need systems that catch mistakes before they reach the patient.Bar code medication administration (BCMA) reduces adverse drug events by 50%. That’s not a guess. It’s from the Leapfrog Group’s data. When a pharmacist scans the prescription, the system checks the drug name, strength, quantity, and patient ID against the electronic record. If the generic version doesn’t match the prescriber’s intent-or if it’s a look-alike drug-it flags it. Simple. Effective.
Computerized Physician Order Entry (CPOE) cuts errors by 55% in hospitals and 48% in primary care. Why? Because it removes handwriting. No more “is that a 5 or a 9?” No more “is that HCTZ or HCTZ 25?” It forces the prescriber to pick from a dropdown menu. And if they pick a generic that’s not on the formulary, the system asks: “Are you sure? This version has a different excipient profile.”
Clinical Decision Support Systems (CDSS) are even smarter. They don’t just check for interactions. They check for substitution risks. If a patient has had a reaction to a generic from a specific manufacturer before, the system remembers. If the new prescription is for a different generic version, it warns the pharmacist: “Patient previously reported nausea with Teva’s metformin. This is a different formulation.”
But here’s the catch: 35-40% of community pharmacies in the UK still don’t use these systems. Many rely on paper scripts, manual checks, and memory. That’s not enough.

Human Checks: The Last Line of Defense
Technology helps-but it doesn’t replace the pharmacist. The “8 R’s” still matter: Right patient, right drug, right dose, right time, right route, right documentation, right reason, right response. But they’re useless if you’re rushing through 80 prescriptions an hour.The most powerful human tool? Mandatory counseling for first-fill generics. It adds 3-5 minutes per patient. But it catches 12-15% of errors. That’s not a small number. That’s one in eight mistakes stopped before the patient walks out.
What do you say? “This is the same medicine as before, but made by a different company. It looks different, but it works the same. If you’ve had any side effects with your last refill, let me know.” That’s it. No jargon. No lecturing. Just a quick, clear conversation.
And if the patient says, “I don’t feel the same on this one”? Don’t dismiss it. Even if the bioequivalence is within range, some people react to different excipients-lactose, dyes, fillers. One patient might be fine with one generic. Another might get a rash or stomach upset. That’s not “in their head.” It’s real. And it’s documented.
What Pharmacists Can Do Today
You don’t need a million-dollar system to reduce errors. Start here:- Update your drug references. 42% of pharmacists use outdated databases. Use Drug Facts and Comparisons or Epocrates. Update them yearly. It costs less than £300.
- Label clearly. Always write the generic name AND the manufacturer on the bottle. “Lisinopril (Teva)” not just “Lisinopril.”
- Train your team. Spend 1-2 hours a month reviewing common LASA errors. Show pictures of different generic versions of the same drug. Make it visual.
- Ask patients. “Have you taken this medication before? Did you ever feel different when the pill changed?” That one question catches more errors than any software.
- Track your errors. Only 28% of community pharmacies do this. Start a simple log: what happened, how it was caught, how to prevent it next time. You’ll see patterns.
The Bigger Picture: Why This Matters
Medication errors cost the NHS and healthcare systems billions. In the U.S., they cost $77 billion a year. In the UK, it’s harder to pin down exact numbers, but the scale is similar. Every error is a patient who didn’t get better. Or got worse. Or ended up in hospital.Generics are essential. They make healthcare affordable. But they’re not risk-free. The goal isn’t to stop generics. It’s to make them safer. To make sure the patient gets the right drug, in the right form, with the right information.
The future is coming. AI-powered systems are being tested to predict which patients might react to specific generic formulations based on their genetics. Pilot programs show a 22% drop in errors beyond standard systems. But that’s years away. Right now, the tools we have are simple, proven, and underused.
Pharmacists are the last checkpoint. Don’t let the system fail them. Don’t let the patient pay the price.
Are generic medications less safe than brand-name drugs?
No, generic medications are not less safe. They must meet the same strict standards for active ingredients, strength, and absorption as brand-name drugs. The Medicines and Healthcare products Regulatory Agency (MHRA) and the FDA require generics to be bioequivalent-meaning they deliver the same amount of active ingredient into the bloodstream within a narrow range (80-125%). The difference lies in non-active ingredients, size, color, or shape, which can cause confusion but not reduced effectiveness or safety when used correctly.
Why do generic pills look different each time I refill?
Different manufacturers produce the same generic drug, and each has its own design for the pill-color, shape, imprint. This is allowed under regulations. Your pharmacy may switch suppliers based on cost or availability. It doesn’t mean the medicine changed. But if you notice a change, always ask your pharmacist to confirm it’s the same medication. Never assume.
Can generic substitutions cause side effects?
Yes, sometimes. While the active ingredient is the same, the fillers, dyes, or preservatives in generics can differ. Some patients are sensitive to lactose, gluten, or artificial colors. If you notice new side effects after switching to a different generic version, tell your pharmacist. They can check the manufacturer’s ingredients and request a switch back to the previous version if needed.
What should I do if I think I received the wrong generic medication?
Don’t take it. Call your pharmacy immediately. Bring the bottle with you if possible. Compare the pill to your last refill using a reliable source like the NHS medicines finder or Epocrates. If you’re unsure, ask the pharmacist to verify the drug and manufacturer. Never guess. It’s better to be safe than sorry.
How can I help prevent errors when picking up my generics?
Always check the pill against your last refill. Note the color, shape, and imprint. Ask the pharmacist: “Is this the same as before?” If it looks different, ask why. Read the label carefully. If you’re unsure about the dose or frequency, ask again. Don’t be shy-your safety matters more than saving time.
Next Steps: What to Do Now
If you’re a pharmacist: Start with one change this week. Update your drug database. Add manufacturer names to labels. Train your team on one common LASA error. Track one error this month. Small steps add up.If you’re a patient: Don’t accept a pill you don’t recognize. Ask questions. Keep a list of your meds, including the manufacturer. Bring it to every appointment.
Generics saved healthcare money. But they didn’t fix the system. The system still fails people. You can change that. One check. One question. One conversation at a time.






James Rayner
December 16, 2025 AT 20:37It’s funny-how something so simple, like a pill’s color, can trigger full-blown panic in someone who’s been stable for years. I’ve seen it with my grandma: she’d stare at the new tablet like it was a foreign object, whispering, ‘This isn’t the one…’ And yet, it was. Same active ingredient. Same effect. Just… different packaging. It’s not the medicine that’s broken. It’s the system that treats patients like they’re machines who shouldn’t notice change.
Maybe we need a ‘pill ID’ card-like a QR code on the bottle that links to a 30-second video of the pill spinning, explaining what it is, why it looks different, and that it’s safe. Just a little human touch. Would cost nothing to implement. Would mean everything to someone scared they’re being poisoned by their own prescription.
Kayleigh Campbell
December 18, 2025 AT 08:44So let me get this straight-we’ve got a healthcare system that can land robots on Mars, but can’t make a pill that doesn’t look like it came from a 90s cereal box?
Also, why do we still use ‘Lisinopril’ as if it’s a secret code? Just write ‘blood pressure pill (Teva)’ on the bottle. People aren’t pharmacists. They’re tired humans who just want to feel better without doing a CSI investigation on their own medicine.
And can we please stop pretending generics are ‘just as good’? They’re chemically identical, sure. But if my stomach throws a tantrum every time I switch manufacturers, that’s not ‘in my head.’ That’s biology. And it deserves respect, not a shrug.
Ron Williams
December 19, 2025 AT 17:34As someone who’s worked in rural pharmacies for 18 years, I’ve seen the same thing over and over: patients don’t trust the new pill because they’ve never been told it’s the same. We don’t need fancy AI. We need five extra minutes per refill. A smile. A ‘Hey, this one’s blue now, but it’s still the same drug-your last one was from Actavis, this is Teva.’
And honestly? Most people just want to feel heard. Not lectured. Not scanned. Just… seen.
One time, a woman cried because she thought her anxiety meds changed. Turned out she’d been on the wrong dose for two years. We caught it because she asked. That’s the real tech right there.
Billy Poling
December 20, 2025 AT 13:26It is, of course, a matter of profound systemic failure that pharmaceutical regulatory bodies permit the proliferation of non-uniform physical characteristics in generic medications, despite the demonstrable increase in patient confusion, non-adherence, and subsequent adverse events. The FDA’s 80–125% bioequivalence window, while statistically defensible, is clinically irresponsible when applied to vulnerable populations-particularly the elderly, those with cognitive impairment, or those on polypharmacy regimens. The notion that a patient should be expected to discern between six visually distinct formulations of metformin, each bearing a different imprint and color, is not merely impractical-it is ethically indefensible.
Furthermore, the failure to mandate standardized pill design across manufacturers constitutes a de facto privatization of medication identity, wherein corporate branding supersedes patient safety. This is not innovation; it is negligence dressed in the language of cost-efficiency. Until regulators enforce uniformity in shape, size, and color for therapeutically equivalent agents, we are not improving healthcare-we are commodifying risk.
Josias Ariel Mahlangu
December 21, 2025 AT 17:29They let anyone make pills now. No oversight. No accountability. I’ve seen pills that look like candy. That’s not medicine. That’s a lottery. And now they want us to trust these color-changing tablets like they’re some kind of miracle? No. This is corporate greed wrapped in a white coat. Someone’s making money off people’s confusion. Someone’s profiting from the fear of the elderly. Someone’s laughing all the way to the bank while grandma skips her meds because the pill’s blue now.
It’s not a ‘systemic issue.’ It’s corruption. And it’s going to kill someone. Soon.
Souhardya Paul
December 21, 2025 AT 23:57Love the emphasis on the 8 R’s. But here’s a thought: what if we made the pharmacist’s job easier by giving patients a simple, printable ‘Medication Change Checklist’ to bring to the pharmacy? Like: ‘Is this the same as last time? Did the color/shape change? Is the manufacturer listed? Did I feel different on the last one?’
It’s not just about training pharmacists-it’s about empowering patients as partners. I’ve given this to my mom. She now asks, ‘Who made this?’ like it’s a normal question. And guess what? The pharmacist started smiling. Now they both know each other’s names. That’s the real win.
Small things. Big impact. We don’t need AI to fix this. We need a little more humanity in the process.
Mike Smith
December 22, 2025 AT 01:59Pharmacists are the unsung heroes of healthcare-and they’re being asked to do the impossible. Eighty prescriptions an hour. No time to counsel. No time to double-check. No time to breathe.
Let’s stop blaming individuals and start fixing the system. Fund the tech. Reduce the workload. Pay them what they’re worth. And if you’re a patient? Thank your pharmacist. Seriously. Write them a note. Buy them coffee. They’re holding the line between you and disaster-and most days, they’re doing it with zero fanfare.
Change starts with respect. Not just policy. Not just software. Respect.
Cassandra Collins
December 22, 2025 AT 17:01Okay but what if the pills are being switched on purpose? Like… what if the government is replacing them with cheaper versions that have weird fillers to make people sick so they buy more drugs later? I heard a guy on a podcast say the dyes in generics are linked to ADHD spikes. And why do all the blue pills come from the same factory? Coincidence? I don’t think so. 🤔💊 #PharmaCoverup
Kitty Price
December 24, 2025 AT 03:13My mom switched to a new generic and got a rash. She didn’t say anything for weeks because she didn’t want to ‘be a bother.’
Then I found her Googling ‘is this pill poison?’ at 2 a.m.
Just… ask. Always ask. Even if it feels silly. Even if you’re embarrassed.
It’s not silly. It’s survival. ❤️