After surgery, your body is healing-and that means your medications matter more than ever. Even short-term drugs like painkillers, antibiotics, or muscle relaxants can cause serious harm if used incorrectly. The truth? Medication errors are one of the leading causes of preventable harm after surgery. In fact, nearly 30% of all medication mistakes happen in surgical settings, and about 20% of those lead to patient injury. This isn’t about fear-it’s about knowing what to do so you don’t become a statistic.
Why Post-Surgery Medications Are Different
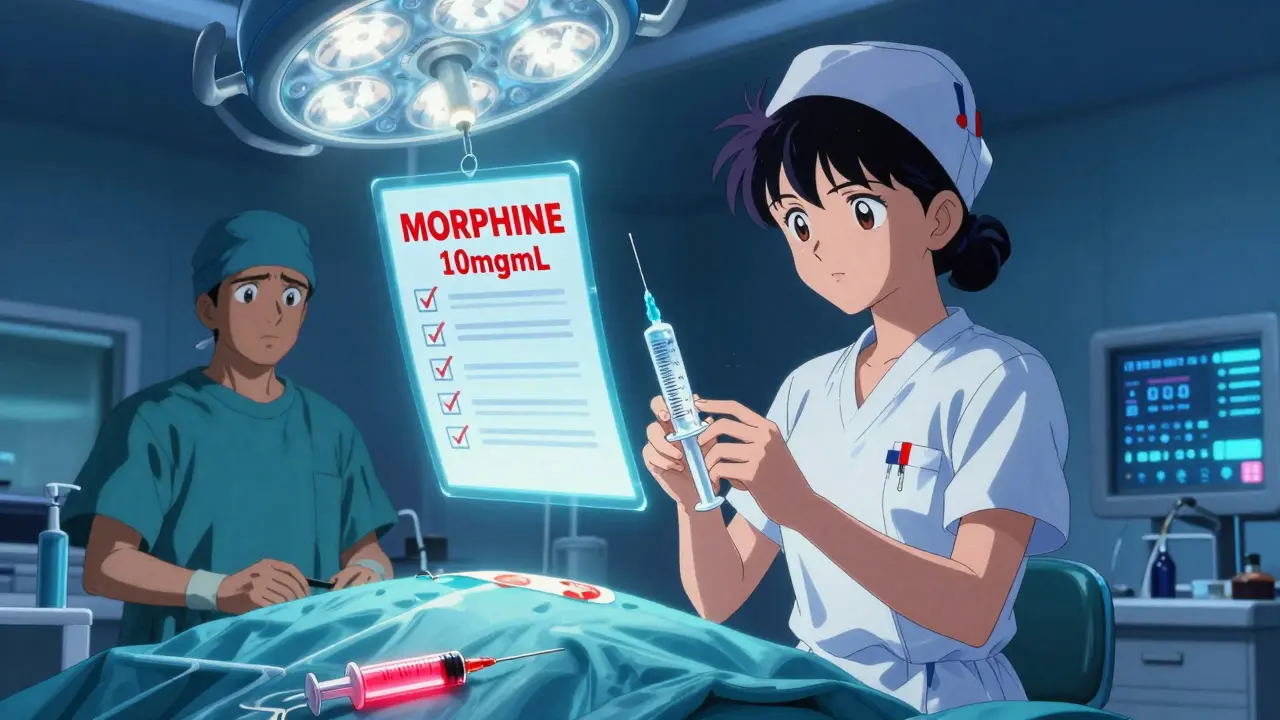
You wouldn’t take a prescription the same way after a knee replacement as you would for a cold. After surgery, your body is under stress, your metabolism changes, and your pain levels can shift fast. That’s why medications given right after surgery are often high-alert drugs: opioids like morphine, sedatives, antibiotics, blood thinners like heparin, and even insulin. These aren’t ordinary pills you pick up at the pharmacy. They’re given in hospitals, ambulatory centers, or even at home under strict protocols.The CDC says unsafe injection practices caused 44 outbreaks between 2001 and 2011, affecting over 14,000 patients. That’s not ancient history-it’s why every syringe used during surgery must be sterile, labeled, and discarded after use. Even one reused needle or unlabeled vial can cost someone their health.
The Five Rules of Safe Medication Use After Surgery
Following the guidelines from the Institute for Safe Medication Practices (ISMP) and the CDC, here’s what actually works:- Label everything, immediately. Any syringe, cup, or bowl with medication on the surgical field must be labeled with the drug name, concentration, and time it was prepared. No exceptions. Unlabeled containers? Throw them out. The Joint Commission requires this-and hospitals that skip it see 47% more errors.
- Never reuse syringes-even for the same patient. If a nurse draws up a second dose of painkiller during surgery, they must use a new syringe and needle. The CDC says syringes used during a procedure must be discarded immediately after use. Even if it’s just sitting on the table for five minutes, it’s contaminated.
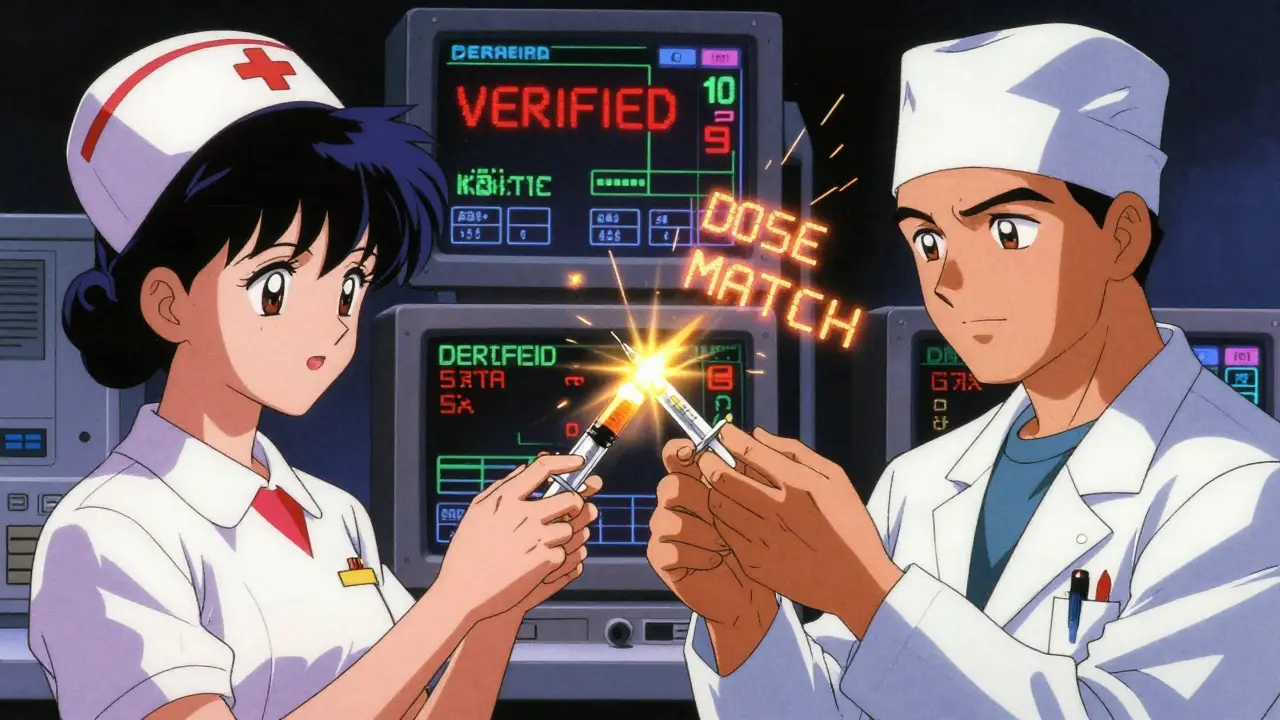
- Verify every dose out loud. In high-pressure moments, verbal orders are common. That’s why nurses and anesthesiologists use the "read-back" method: the person receiving the order repeats it back word-for-word. Studies show this cuts verbal errors by 55%. It’s not awkward-it’s lifesaving.
- Know your high-alert drugs. Opioids, heparin, insulin, and neuromuscular blockers are the most dangerous if misused. The American Society of Anesthesiologists requires these to be clearly labeled with concentration (e.g., 10 mg/mL vs. 1 mg/mL). One wrong decimal point can kill.
- Document everything. Electronic records cut documentation errors by 92% compared to paper. If your dose, time, or route isn’t recorded, it didn’t happen. That’s not bureaucracy-it’s accountability.
What Patients Can Do (Yes, You)
You might think medication safety is just the hospital’s job. But you’re the one taking the pills. Here’s how to protect yourself:- Ask: "What is this for?" If you’re given a new drug, even just one pill, ask why. Many patients don’t realize they’re being given a muscle relaxant instead of a painkiller.
- Check the label. When you get home with prescriptions, look at the name, dose, and instructions. Does it match what your surgeon said? If not, call the pharmacy.
- Don’t take leftover opioids. Opioid misuse after surgery is rising. The CDC recommends using the smallest effective dose for the shortest time. If you have leftover pills, return them to the pharmacy. Don’t store them.
- Speak up if something feels off. If you’re dizzy, nauseous, or confused after a dose, tell someone. Early signs of overdose or reaction are often ignored until it’s too late.
Common Mistakes-and How to Avoid Them
Real-world errors aren’t dramatic. They’re quiet. Here’s what goes wrong:- Wrong concentration. Epinephrine for a middle ear procedure is 1:1000, but for cardiac arrest it’s 1:10,000. Mixing them up can stop a heart. Surgical teams now use color-coded labels and separate storage.
- Time pressure. In emergencies, 15-20% of doses skip verification. The fix? Slowing down just long enough to say the name out loud. One extra second saves lives.
- Labeling delays. Nurses report it takes 27 seconds to label a syringe. In a rush, that gets skipped. But facilities that train staff and build labeling into workflow reduce errors by 63%.
- Discharge confusion. Over 67% of adverse drug events happen when patients leave the hospital. Medication reconciliation-comparing what you were on before surgery to what you’re going home with-cuts these errors dramatically.
What Hospitals Are Doing Right
Some places are turning the tide. Academic hospitals have 87% adoption of full medication safety protocols. They use:- Barcode scanning at the bedside (reduces errors by 39%)
- Smart syringes that auto-verify dose and drug type
- Standardized checklists for every procedure
- Regular staff training-CSTs (Certified Surgical Technologists) need 12-15 hours of dedicated safety training
One hospital cut errors by 63% just by requiring surgical techs to verbally confirm every drug before handing it to the surgeon. That’s not guesswork-that’s a system.
What Happens If You Don’t Follow These Rules?
The risks aren’t theoretical. From 2020 to 2022, over 1,200 medication errors were reported in surgical settings. The top causes:- 32%: Wrong drug selected
- 28%: Wrong dose given
- 19%: Unlabeled or mislabeled containers
These aren’t rare. They’re routine. And they’re preventable. The World Health Organization says medication reconciliation at discharge can reduce adverse events by two-thirds. That’s not a suggestion-it’s a proven solution.
Looking Ahead
The future of medication safety is here. Smart syringes that block wrong doses, barcode systems in ORs, and AI-assisted verification are being tested. But until those are everywhere, the old rules still work: label, verify, communicate, document.The system isn’t perfect. But you’re not powerless. Whether you’re a patient, a nurse, or a surgeon, your actions matter. One clear label. One verbal confirmation. One honest question. That’s how you stop a mistake before it becomes a tragedy.
Can I take leftover painkillers after surgery if I still feel pain?
It’s not recommended. Opioids prescribed after surgery are meant for short-term use-usually 3 to 7 days. Taking them longer increases the risk of dependence, especially if you didn’t have prior opioid use. If pain continues past the first week, contact your surgeon. There are safer, non-opioid options like NSAIDs, physical therapy, or nerve blocks that can help without the risks.
Why are syringes labeled with expiration times after surgery?
Medications in syringes can degrade or become contaminated if left unattended. For example, epinephrine loses potency after 24 hours outside refrigeration. The label with the time it was drawn ensures no one uses an outdated or unsafe dose. Even if it looks fine, it might not be safe. The Joint Commission requires this to prevent accidental overdose or ineffective treatment.
Is it safe to use someone else’s leftover medication after my surgery?
Absolutely not. Medications are prescribed based on weight, allergies, kidney function, and other personal factors. What’s safe for one person could be deadly for another. Even antibiotics or anti-inflammatories can cause serious reactions if not matched to your history. Never share or take medications not prescribed specifically for you.
What should I do if I think I received the wrong drug after surgery?
Speak up immediately. Tell a nurse or doctor-even if you’re not sure. Common signs of a wrong drug include sudden dizziness, nausea, rapid heartbeat, or confusion. Don’t wait. Most errors are caught before they cause harm if someone asks. You have the right to know what you’re being given and why.
Are electronic systems better than paper for medication records after surgery?
Yes. Facilities using electronic documentation have 92% fewer medication recording errors than those using paper. Digital systems reduce illegible handwriting, missed entries, and timing mistakes. They also flag potential drug interactions or incorrect doses before they’re given. While not perfect, they’re the most reliable method available today.