Every year, thousands of people end up in the hospital because of something they didn’t tell their doctor: the vitamins, herbs, or painkillers they’re taking without a prescription. It’s not that they’re hiding anything on purpose. Most just don’t think it matters. But here’s the truth: over-the-counter medications and dietary supplements aren’t harmless. They can change how your prescriptions work, damage your liver, or even cause bleeding when mixed with blood thinners. If you’re taking anything outside of your prescription list-whether it’s fish oil, melatonin, turmeric, or ibuprofen-you need to share it accurately. Not just mention it. Not just say ‘I take vitamins.’ Say exactly what, how much, and why.
Why This Isn’t Just a Good Idea-It’s a Safety Must
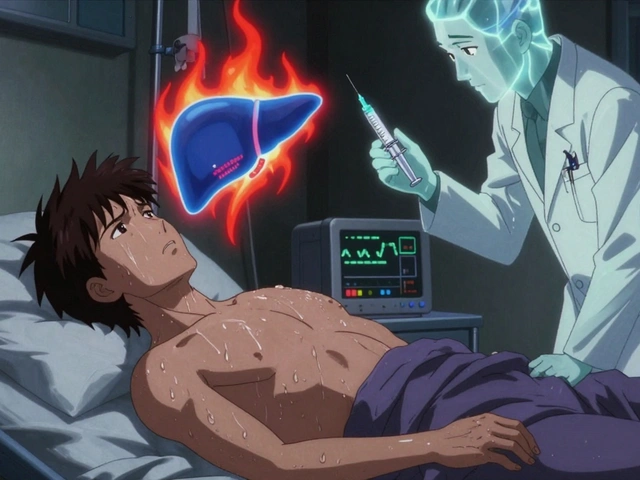
The FDA logged over 1,000 adverse events linked to dietary supplements in 2022, including 52 deaths. Many of these cases involved people who didn’t tell their doctors what they were taking. One woman took kava for anxiety while on antipsychotic medication. She never mentioned the supplement. She died of acute liver failure. Her providers didn’t know until it was too late. That’s not rare. Studies show that 23% of hospital patients have potential interactions between their prescriptions and supplements they didn’t disclose. Of those, nearly 8% were severe enough to require emergency care. Why does this happen? Because most people don’t realize supplements are medicines in disguise. They think ‘natural’ means ‘safe.’ But St. John’s Wort-a common herb for mood-can make birth control, antidepressants, and even heart medications stop working. Green tea extract, often taken for weight loss, has caused liver failure when combined with acetaminophen. These aren’t myths. These are documented cases, tracked by the FDA and published in peer-reviewed journals.What Counts as a Supplement? (And Why You’re Probably Missing Some)
Many people think supplements only mean pills in a bottle. They forget about gummies, powders, teas, and even energy bars labeled as ‘nutritional support.’ If it has a Supplement Facts label, it’s a supplement. That includes:- Vitamins and minerals (like vitamin D, magnesium, iron)
- Herbs and botanicals (like echinacea, ginseng, turmeric)
- Probiotics and omega-3s (fish oil, flaxseed)
- Weight loss or sports performance products (creatine, collagen, fat burners)
- Sleep aids (melatonin, valerian root)
The Exact Way to Document What You’re Taking
Don’t just say, ‘I take fish oil.’ Say: ‘I take Nature Made Fish Oil 1,000 mg, one capsule twice a day, for joint pain.’ The difference matters. Here’s the full checklist for accurate documentation:- Product name-Use the full brand name, not just ‘vitamin B12.’
- Dosage-Write the exact amount: ‘500 mg,’ not ‘a pill.’
- Frequency-‘Once daily,’ ‘every other day,’ ‘as needed.’
- Purpose-‘For sleep,’ ‘for immune support,’ ‘for my cholesterol.’
- Where you bought it-Was it from a pharmacy, Amazon, or a health food store? Some brands have contamination issues.

Why Your Doctor Might Not Ask-And What to Do About It
Only 22% of healthcare providers routinely screen for supplement use. That’s not because they don’t care. It’s because they’re overwhelmed. Most electronic health records don’t have a dedicated field for supplements. So if you don’t bring it up, it gets missed. A 2022 study found that 53% of patients who didn’t disclose supplements said their provider never asked. Another 28% thought their provider didn’t need to know. That’s the biggest barrier: misunderstanding. You don’t need permission to speak up. You don’t need to wait to be asked. Here’s what to say: ‘I want to make sure everything I’m taking is safe with my other meds. Here’s what I use.’ Then hand them the list. If they brush you off, say: ‘I’ve read that supplements can interact with prescriptions. I’d feel better if we checked.’ Providers who ask about supplements get 4.7 out of 5 in patient satisfaction scores. Those who don’t? 3.2. Your voice matters.Pharmacists Are Your Secret Weapon
If you’re unsure whether your supplement is safe, talk to your pharmacist. Not your doctor. Not your nurse. Your pharmacist. They’re trained to catch interactions. A 2021 study found pharmacists identify 3.2 times more supplement-drug interactions than physicians during medication reviews. Why? Because they see the full picture-every pill, every dose, every label. When you pick up a prescription, ask: ‘I also take fish oil and magnesium. Are these okay with this new medicine?’ Most pharmacies offer free med reviews. Use them. You’re not bothering them. You’re helping them protect you.
What Happens When You Get It Right
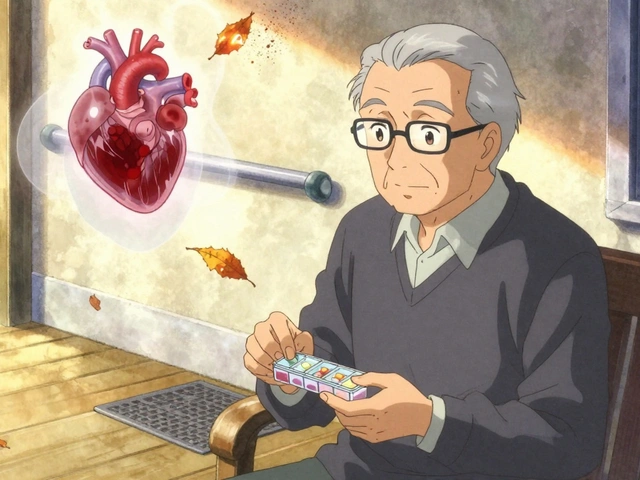
A 68-year-old woman in Texas took 1,000 mg of fish oil daily for her arthritis. She never mentioned it. Her blood thinner, warfarin, was dosed based on her INR levels-until her INR spiked dangerously high. Her doctor finally asked about supplements. Turns out, the fish oil was thinning her blood too. They cut the dose to 500 mg. Her INR stabilized. She avoided a hospital stay. That’s not luck. That’s communication. When you share exactly what you’re taking, your provider can adjust your treatment. They can spot hidden risks. They can help you use supplements safely-or tell you to stop.What’s Changing-And Why It Matters
In 2024, the FDA is rolling out new rules requiring supplement manufacturers to report adverse events within 15 days (down from 30). They’re also pushing for digital product IDs on labels-like barcodes you can scan to see ingredients and warnings. Epic Systems, the biggest EHR platform in the U.S., just added AI-powered screening in 2024 that checks your supplement list against 14,700 products and your prescriptions. But none of this matters if you don’t speak up. Technology can flag risks. But only you know what’s in your medicine cabinet.Start Today: Your 5-Minute Action Plan
You don’t need to wait for your next appointment. Do this now:- Go through your cabinets. Collect every bottle, box, or packet of OTC meds or supplements.
- Write down the name, dose, frequency, and reason for each one.
- Download the NIH’s free My Dietary Supplement and Medicine Record form and fill it out.
- Bring it to your next visit-even if it’s just a checkup.
- Next time you refill a prescription, ask your pharmacist: ‘Does this interact with anything I’m taking?’
Do I need to tell my doctor about vitamins and minerals?
Yes. Vitamins and minerals are dietary supplements, and they can interact with medications. For example, vitamin K can reduce the effect of blood thinners like warfarin. Iron can interfere with thyroid medication and antibiotics. Even something as simple as calcium can block absorption of some drugs. Always list them by name and dose.
Can I just say ‘I take supplements’ without listing them?
No. Saying ‘I take supplements’ is too vague. A provider can’t check for interactions if they don’t know what you’re taking. ‘Fish oil’ and ‘krill oil’ are different. ‘500 mg’ and ‘1,000 mg’ have different risks. Exact details are the only way to stay safe.
Why don’t doctors ask about supplements more often?
Many providers don’t have time, and most electronic health records don’t have a dedicated field for supplements. Some assume patients will mention them. Others don’t realize how common supplement use is-78% of Americans take them. The responsibility falls on you to bring it up. Don’t wait to be asked.
Are natural supplements safer than prescription drugs?
No. ‘Natural’ doesn’t mean safe. Kava, comfrey, and green tea extract have caused liver failure. St. John’s Wort can make your birth control or antidepressant useless. Supplements aren’t tested for safety the way prescription drugs are. They’re regulated differently, which means the burden is on you to disclose them.
Should I stop taking supplements before surgery?
Many should be stopped at least 1-2 weeks before surgery. Fish oil, garlic, ginkgo, and high-dose vitamin E can increase bleeding risk. Turmeric and ginger can affect blood sugar. Always tell your surgeon and anesthesiologist about everything you take-even if they don’t ask. They’ll tell you what to pause and when.
Can I trust the label on my supplement bottle?
Not always. A 2022 Government Accountability Office report found 23% of supplement labels had inaccurate ingredient lists. Some contain hidden drugs, others have less or more than stated. That’s why you need to tell your provider the exact product name and brand-not just the ingredient. They can look up known issues with that specific product.
Is it okay to take supplements with my prescriptions if I space them out?
Not necessarily. Some interactions happen in your liver, not your stomach. For example, St. John’s Wort changes how your body breaks down medications, no matter when you take them. Spacing doses won’t prevent that. Only your provider can tell you if it’s safe based on your full health picture.





Theo Newbold
December 21, 2025 AT 16:19Just had my third liver enzyme test this year because I didn’t mention the turmeric capsules I was taking for ‘joint support.’ Turned out they were 800mg each, not the 250mg I thought. My PCP didn’t even blink when I said ‘I take herbs.’ That’s the problem. We treat supplements like candy. They’re not. The FDA data isn’t scare tactics-it’s a logbook of people who thought they were being careful and weren’t.
Cara C
December 23, 2025 AT 00:12This is so important. I used to say ‘I take vitamins’ too-until my mom had a bad reaction to her blood thinner after starting a new magnesium supplement. We didn’t realize it was the combo. Now I have a little notepad in my wallet with everything I take, brand and dose. I hand it to every provider. No one’s ever said ‘that’s unnecessary.’ They’ve all said ‘thank you.’
Michael Ochieng
December 24, 2025 AT 14:23As someone who’s lived in four countries, I can tell you this isn’t just an American issue. In Kenya, people use moringa like it’s water. In Germany, they pop St. John’s Wort like aspirin. In Japan, they drink green tea extract powders daily. No one thinks twice. But here’s the kicker: pharmacists everywhere are the real MVPs. I always ask mine. They’ve caught three interactions I didn’t even know existed. Your doctor’s busy. Your pharmacist? They’re literally paid to catch this stuff.
Erika Putri Aldana
December 26, 2025 AT 08:17Ugh. I’m so tired of being guilt-tripped into being a ‘responsible adult.’ I take melatonin because I can’t sleep. I take omega-3 because I hate fish. If my doctor wants to know, they can ASK. I’m not your personal pharmacy assistant. Also, ‘natural’ doesn’t mean safe? Tell that to the 10,000-year-old tradition of herbal medicine. 🤦♀️
Siobhan K.
December 27, 2025 AT 13:41Oh, so now we’re supposed to become full-time pharmacists just because our doctors refuse to update their 1998 EHR systems? Brilliant. Let’s just blame the patient for the system’s failure. And yes, I’ve documented everything. I even have a spreadsheet with batch numbers and expiration dates. And yet, my last doctor still said ‘I don’t really care about supplements unless you’re taking something like kava.’ So what’s the point? The system is broken. But I’ll keep documenting anyway-because I’m not dying because someone didn’t bother to ask.
Ben Warren
December 28, 2025 AT 07:57It is a matter of profound clinical significance that a significant proportion of the American populace continues to conflate the regulatory status of dietary supplements with that of pharmaceutical agents. The Food and Drug Administration, under Title 21 of the Code of Federal Regulations, explicitly delineates a distinction in pre-market scrutiny; however, consumer perception remains catastrophically misaligned with this legal reality. The anecdotal evidence presented herein is corroborated by peer-reviewed literature from the Journal of the American Medical Association and the New England Journal of Medicine, which collectively demonstrate a statistically significant correlation between undisclosed supplement use and preventable adverse drug events. It is therefore not merely prudent, but ethically incumbent upon the patient to provide a complete, itemized, and verifiable inventory of all ingestible substances-regardless of perceived innocuousness-to ensure the integrity of the therapeutic regimen.
Teya Derksen Friesen
December 29, 2025 AT 04:13Just downloaded the NIH form. Took me 4 minutes. Listed everything: my magnesium, my collagen, my CBD gummies (yes, those count), even the ginger chews I chew when I’m nauseous. I’m bringing it to my next appointment. I’m not waiting to be asked. I’m not apologizing for being thorough. This isn’t about being ‘overly cautious.’ It’s about being alive.
Sandy Crux
December 29, 2025 AT 12:43...And yet... the NIH form... is... still... a PDF...? ...In 2024? ...No mobile-friendly version? ...No API integration with Apple Health? ...No QR code linking to batch-specific safety data? ...How is this acceptable? ...I’m not even mad... I’m just... disappointed... in the entire system... and... also... I still take fish oil... because... I’m... not... a... robot... and... I... like... my... joints...