When someone stops drinking after years of heavy alcohol use, their body doesn’t just feel shaky-it’s in crisis. The liver, which has been working overtime to break down alcohol every day, suddenly has to adjust to a new reality. This is where alcohol withdrawal and liver health collide. It’s not just about sweating through tremors or insomnia. It’s about whether your liver will heal-or suffer more damage during the very time it should be recovering.
What Happens to Your Liver When You Quit Drinking?
Your liver processes about 90% of the alcohol you drink. It turns ethanol into acetaldehyde, a toxic byproduct, then into acetate, which your body can use for energy. But when you stop drinking suddenly after long-term use, your liver doesn’t just rest. It goes into overdrive, scrambling to rebalance its metabolism. This can cause a spike in liver enzymes like AST and ALT-even though you’re no longer drinking.
Studies show that 32% of people who quit alcohol abruptly see a sharp rise in these enzymes within the first week. That doesn’t mean the liver is failing. It means it’s stressed. The AST:ALT ratio is a key clue: if it’s above 2:1, it’s a strong sign of alcohol-related liver damage. Normal is under 1:1. High AST and low ALT? That’s alcohol’s fingerprint.
But here’s the good news: your liver is one of the few organs that can regenerate. If the damage isn’t too far gone, stopping alcohol can reverse fatty liver in weeks. Even moderate alcoholic hepatitis can improve significantly after 4-8 weeks of abstinence. The key? No more alcohol. Ever.
The Real Danger: Withdrawal Isn’t Just Uncomfortable-It’s Deadly
Alcohol withdrawal isn’t like quitting coffee. It can kill you. Symptoms start 6-24 hours after your last drink. Nausea, tremors, anxiety, rapid heartbeat, high blood pressure-these are common. But in 5% of cases, things turn dangerous fast. Delirium tremens (DTs) can strike between 48-96 hours after stopping. Hallucinations, seizures, extreme confusion, fever-this is a medical emergency.
People with existing liver damage are at higher risk. Why? Because their bodies are already struggling to regulate fluids, electrolytes, and brain chemicals. A liver that’s been damaged by alcohol can’t buffer these changes well. That’s why unsupervised detox at home is risky. A 2022 meta-analysis found medically supervised detox is 95% safe. Unsupervised? Only 65%.
Doctors use benzodiazepines like chlordiazepoxide to prevent seizures and calm the nervous system. These aren’t addictive when used short-term under medical care. They’re the gold standard. Symptom-triggered dosing works for mild cases, but for anyone with liver disease, fixed-schedule dosing is safer.
What You Must Avoid During Detox-Even If It Seems Harmless
One of the biggest mistakes people make after quitting alcohol? Taking paracetamol (acetaminophen) for headaches or fever. It’s in every medicine cabinet. But during withdrawal, your liver is extra vulnerable. A 2002 study found that even small doses-just 1-2 grams a day-could cause massive liver enzyme spikes in people going through withdrawal. That’s the same dose you’d take for a bad migraine.
Don’t take NSAIDs like ibuprofen either. They can stress the kidneys and worsen fluid imbalances. Stick to non-medicated options: cold compresses, rest, hydration. If you need pain relief, talk to your doctor first. No exceptions.
Another hidden danger: alcohol-based hand sanitizers or mouthwashes. They’re not enough to cause intoxication, but for someone with a damaged liver, every bit of ethanol counts. Switch to alcohol-free versions during detox.

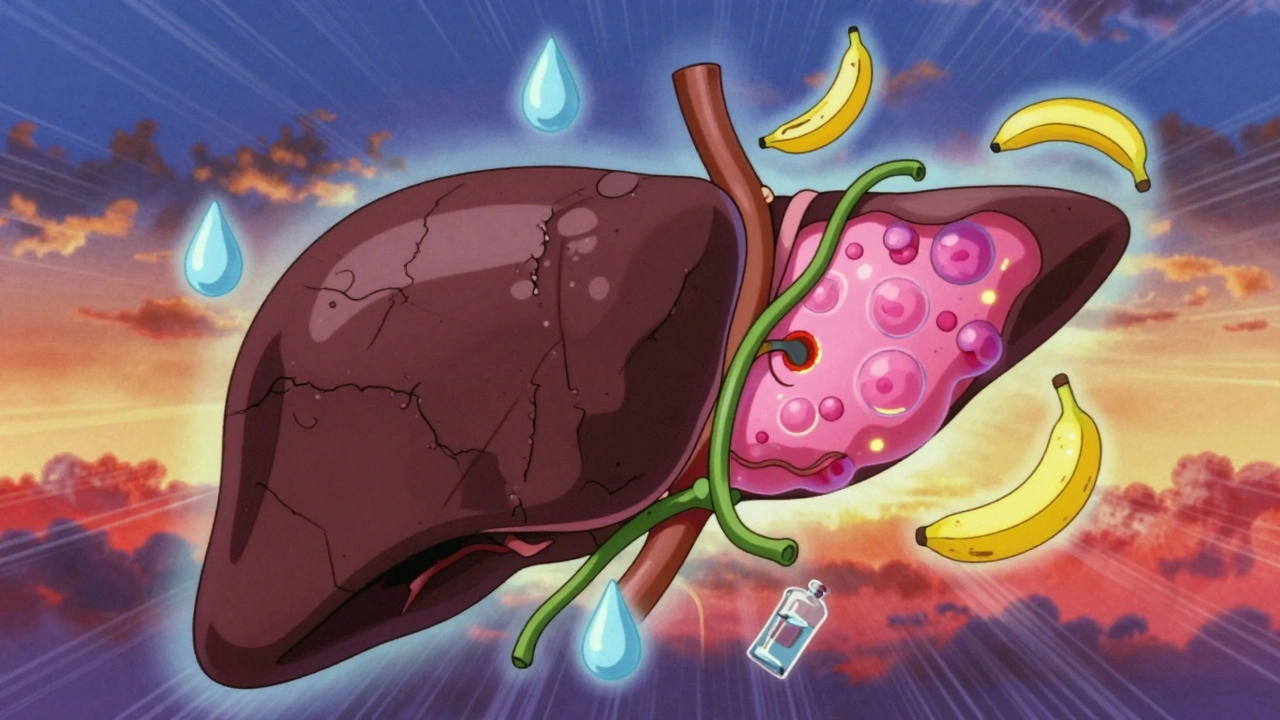
How to Support Your Liver While You Detox
Detox isn’t just about stopping alcohol. It’s about giving your liver what it needs to heal.
Thiamine (vitamin B1) is non-negotiable. Heavy drinkers are almost always deficient. Without it, you risk Wernicke-Korsakoff syndrome-a neurological condition that can cause permanent memory loss. Doctors give 500mg IV daily for the first 3-5 days. Oral supplements won’t cut it at this stage.
Protein intake matters too. Aim for 1.2-1.5 grams per kilogram of body weight. That’s about 80-100g of protein a day for a 70kg person. Eggs, lean meats, fish, lentils, tofu. Protein helps repair liver cells and prevents muscle wasting during withdrawal.
N-acetylcysteine (NAC) is a supplement that’s shown promise in studies. One trial found it reduced liver enzyme spikes by 30% compared to placebo. It helps restore glutathione, your liver’s main antioxidant. Talk to your doctor about adding it-especially if your enzymes are high.
Hydration and electrolytes are critical. Alcohol depletes sodium, potassium, magnesium. Drink water. Eat bananas, spinach, yogurt. Consider an oral rehydration solution if you’re vomiting or sweating heavily.
How Long Until Your Liver Recovers?
There’s no single timeline. It depends on how bad the damage was.
- Mild fatty liver: Enzymes drop in 7-14 days. Full recovery in 6 weeks with no alcohol.
- Alcoholic hepatitis: Improvement starts in 4-8 weeks. Some scarring may remain, but function improves dramatically.
- Cirrhosis: No reversal. But stopping alcohol can stop progression. Survival rates double if you quit before advanced cirrhosis.
Research published in Scientific Reports in 2021 showed that even after years of heavy drinking, the liver can show major healing within 3-12 months of complete abstinence. But if you drink again-even one drink-the healing stops. And the damage starts over.
One study found that people who relapsed within 6 months after detox had no improvement in liver fibrosis. Those who stayed sober? Fibrosis markers dropped. The liver was literally repairing itself.
What Doesn’t Work-And Why
Some people try to quit by slowly cutting back. Tapering. It sounds smart. But for moderate to severe dependence, it’s dangerous. You’re still exposing your liver to alcohol while your body is already stressed. A 2021 study found a 35% failure rate in moderate-severe cases. You’re not giving your liver a break-you’re dragging it through a longer, slower trauma.
Detox teas, liver cleanses, or juice fasts? They’re useless. Your liver doesn’t need a “cleanse.” It needs rest, protein, vitamins, and zero alcohol. No herb, no supplement, no detox drink replaces abstinence.
And don’t assume you’re fine just because you don’t have symptoms. You can have advanced liver damage with no pain, no jaundice, no swelling. That’s why blood tests are essential before and after detox.
When You Need Medical Help-No Excuses
If you’ve been drinking heavily for more than a year, don’t try to quit alone. If you’ve had withdrawal symptoms before-even mild ones-get help. If you have any of these, you need a doctor right away:
- Confusion or disorientation
- Seizures
- High fever
- Heart rate over 120 bpm
- Yellow skin or eyes
- Swelling in your belly or legs
Even if you’re in a rural area with limited access, telemedicine options exist. Many clinics now offer virtual monitoring with remote vital sign tracking. It’s not perfect, but it’s better than nothing.
Insurance often covers medically supervised detox. Private plans cover 85% of costs. Medicaid covers 45%. But if you wait until you’re in crisis, the cost skyrockets. Preventative care saves lives-and money.
What Comes After Detox?
Detox is just the first step. The real work starts after.
Seven out of ten people who finish detox relapse within six months if they don’t have ongoing support. That’s why recovery programs, counseling, and peer groups are part of the treatment-not an afterthought.
For liver health, you need to stay alcohol-free for life if you’ve had alcoholic hepatitis or cirrhosis. For mild fatty liver, some doctors may allow occasional drinking after 6 weeks-but only if you stick to NHS guidelines: no more than 14 units a week, spread out, with 2-3 alcohol-free days.
But here’s the truth: most people who resume drinking-even a little-end up back where they started. The liver remembers. So does your brain.
The goal isn’t just to survive withdrawal. It’s to rebuild. And that takes time, discipline, and support.
Can you reverse liver damage from alcohol?
Yes-if the damage hasn’t progressed to cirrhosis. Fatty liver and mild alcoholic hepatitis can improve significantly within weeks to months of stopping alcohol. The liver regenerates. But if scarring (fibrosis or cirrhosis) has formed, it can’t be undone. The goal then is to stop further damage. Abstinence is the only proven treatment.
Is it safe to detox from alcohol at home?
It’s risky. For mild cases with no history of seizures or delirium tremens, home detox might be possible with close monitoring. But if you’ve been drinking heavily for years, have liver disease, or have had withdrawal symptoms before, medical supervision is essential. Unsupervised detox has a 35% failure rate and carries a risk of death.
Can I take painkillers during alcohol withdrawal?
Avoid paracetamol (acetaminophen) entirely during withdrawal. Even small doses can cause dangerous liver enzyme spikes. Ibuprofen and other NSAIDs can stress your kidneys and worsen fluid imbalances. Only use medications approved by your doctor. For headaches, try rest, hydration, and cold compresses.
How long does alcohol withdrawal last?
Physical symptoms peak at 24-72 hours and usually fade within 5-7 days. But insomnia, anxiety, and cravings can last weeks or months. This is called post-acute withdrawal syndrome (PAWS). It’s not dangerous, but it’s why ongoing support is critical. Your brain is rewiring.
Do I need blood tests before quitting alcohol?
Yes. Blood tests for liver enzymes (AST, ALT), albumin, INR, and bilirubin tell your doctor how damaged your liver is. They also help determine your risk for severe withdrawal. You can’t treat what you don’t measure. Skipping tests is like driving blind.
Can alcohol withdrawal cause permanent liver damage?
Withdrawal itself doesn’t cause permanent damage. But if you have advanced liver disease and don’t stop drinking, you will. The real danger is continuing to drink after withdrawal. The liver can heal-if you give it the chance. But if you relapse, the damage returns faster than before.
If you’re reading this because you or someone you care about is thinking about quitting alcohol, don’t wait. The liver is resilient-but only if you give it a real chance. The first step isn’t a detox tea or a miracle supplement. It’s stopping. And the next step? Getting help.






olive ashley
December 6, 2025 AT 14:57So let me get this straight-you’re telling me if I just stop drinking, my liver magically heals like it’s some kind of superhero? Lol. What about all the glyphosate in your water, the 5G towers, and the fact that Big Pharma doesn’t want you to know about the real cure: colloidal silver? Your ‘science’ is a lie. I’ve seen people detox and die because they didn’t take ionic foot baths first. You’re not helping-you’re enabling the system.
Dan Cole
December 7, 2025 AT 20:07Let’s dismantle this piece of pseudo-medical propaganda with surgical precision. The notion that the liver ‘regenerates’ is a romanticized myth peddled by wellness influencers. Hepatocytes do proliferate-but only if the extracellular matrix remains intact. In chronic alcoholism, stellate cells deposit collagen, creating fibrotic scars that are *irreversible*-not ‘partially reversible’ as this article implies. And don’t get me started on the ‘NAC reduces enzyme spikes by 30%’ claim. That’s a single-center, underpowered RCT with publication bias. The real answer? Zero alcohol. Everything else is noise.
Billy Schimmel
December 8, 2025 AT 14:13Man, I’ve been there. Quit cold turkey after 12 years. Tremors, nightmares, felt like my bones were vibrating. Took me six months to stop wanting a drink at 3 a.m. But I’m alive. My AST/ALT ratio went from 3.1 to 0.8. No magic. Just time. And not taking Tylenol. That part? Crucial. You don’t need a PhD to get this right. Just don’t drink. And maybe call someone.
Inna Borovik
December 8, 2025 AT 16:47Wow. So the author thinks we’re all just one detox away from a liver reboot? What about the people who’ve been drinking for 30 years and have cirrhosis? They’re just supposed to ‘stop’ and wait for the magic? And then there’s the ‘don’t use hand sanitizer’ thing-like we’re all living in a biohazard zone now? This reads like a pharmaceutical ad disguised as harm reduction. The real problem? No one talks about trauma. You don’t quit drinking because you ‘know better.’ You quit because you’re tired of being dead inside. And this article doesn’t even mention that.
Rashmi Gupta
December 8, 2025 AT 22:52Why is everyone so obsessed with Western medicine? In India, we’ve been using neem, amla, and turmeric for liver detox for centuries. No benzodiazepines. No IV thiamine. Just nature. Your liver doesn’t need chemicals-it needs balance. This whole article is colonial nonsense. You think your science is better? Look at your obesity rates, your opioid crisis, your broken healthcare system. We don’t need your ‘gold standard.’ We need our traditions.
Andrew Frazier
December 10, 2025 AT 00:10Ugh. Another liberal ‘you must go to a doctor’ lecture. I’m American. I don’t need some bureaucrat telling me how to quit drinking. I quit cold turkey in my garage with a bottle of water and a baseball bat. No meds. No tests. Just grit. And guess what? My liver’s fine. You think your ‘65% safety rate’ applies to real people? Nah. Real men don’t need IV thiamine. They just stop. Period. And if you can’t? You’re weak. Not sick.
Mayur Panchamia
December 11, 2025 AT 23:53HAHAHAHA! This is the most ridiculous thing I’ve read this week! ‘Avoid alcohol-based hand sanitizer’? So now I can’t wipe my hands after using the toilet? What’s next? Don’t breathe near a wine bar? Don’t kiss your spouse if they had a glass of wine? This article is a joke. I’ve been drinking for 20 years. My liver? Still working. My wife? Still kissing me. My kids? Still calling me Dad. You want to scare people? Fine. But don’t pretend you’re helping. You’re just selling fear.
Karen Mitchell
December 12, 2025 AT 08:28It is, regrettably, imperative to note that the author’s conflation of ‘healing’ with ‘reversal’ constitutes a fundamental misrepresentation of hepatological pathophysiology. The liver’s regenerative capacity is neither infinite nor universally applicable. To suggest that ‘mild alcoholic hepatitis can improve significantly’ without emphasizing the statistical probability of relapse-approximately 70% within six months-is not merely irresponsible; it is ethically indefensible. Furthermore, the omission of socioeconomic determinants-such as housing instability and food insecurity-as critical co-factors in recovery renders this entire discourse dangerously incomplete.
Nava Jothy
December 13, 2025 AT 13:04My heart goes out to anyone reading this and feeling alone. 💔 I’ve been there. I cried for three weeks after I quit. I thought I’d never feel joy again. But I found a group-real people, no judgment. We text at 2 a.m. when the cravings hit. I take NAC now. I eat eggs. I drink water. And guess what? I’m not ‘cured.’ But I’m alive. And that’s enough. You’re not broken. You’re becoming. 🌱