When your period hits hard and nothing seems to ease the cramps, you might reach for Ponstel. It’s a brand name for mefenamic acid, a painkiller that’s been around for decades and still shows up on prescriptions for menstrual pain, headaches, and muscle aches. But is it the best option? Are there safer, cheaper, or more effective alternatives out there? If you’ve been wondering whether to stick with Ponstel or try something else, you’re not alone.
What is Ponstel (mefenamic acid) really doing?
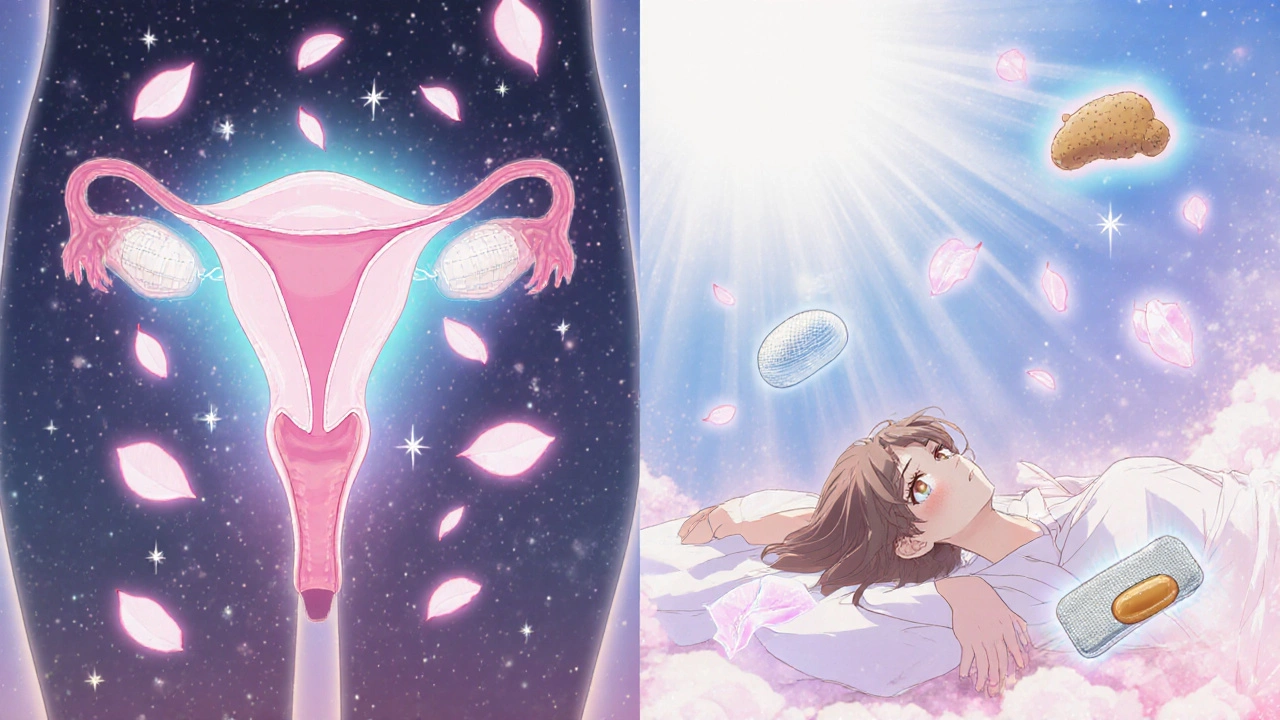
Ponstel works by blocking enzymes called COX-1 and COX-2, which your body uses to make prostaglandins. These are chemicals that cause inflammation, pain, and fever. In menstrual cramps, high levels of prostaglandins make the uterus contract too hard and too often. Mefenamic acid cuts those levels, reducing both pain and heavy bleeding. It’s not a muscle relaxant or a hormone-just a straightforward NSAID.
Most people take 500 mg at the first sign of pain, then 250 mg every 6 hours as needed. It’s not meant for daily use over weeks. The UK’s NHS and the FDA both warn against using it for more than 7 days without medical advice. Side effects? Stomach upset, dizziness, and nausea are common. Rarely, it can cause ulcers, kidney issues, or raise blood pressure. If you have a history of stomach bleeding, asthma triggered by NSAIDs, or heart disease, you should avoid it.
How does mefenamic acid stack up against ibuprofen?
Ibuprofen is the go-to OTC painkiller for most people. It’s cheaper, widely available, and has decades of safety data. Both drugs work the same way-blocking prostaglandins. But here’s the difference: studies show ibuprofen works faster. One 2020 trial in the British Journal of Clinical Pharmacology found that ibuprofen reduced menstrual pain by 50% within 30 minutes for 68% of users. Mefenamic acid took closer to 60 minutes to hit that same mark.
But mefenamic acid might last longer. In the same study, 40% of women using mefenamic acid reported pain relief lasting over 8 hours, compared to 30% on ibuprofen. That’s useful if you’re stuck at work or traveling and can’t take pills every few hours.
For stomach safety, ibuprofen wins. Mefenamic acid is harder on the gut. A 2019 meta-analysis in BMJ Open showed mefenamic acid had a 22% higher risk of gastrointestinal side effects than ibuprofen. If you’ve ever gotten heartburn after taking Ponstel, you’re not imagining it.
What about naproxen? Is it better for heavy periods?
Naproxen is another NSAID, sold as Naprosyn or generic. It’s longer-acting than both ibuprofen and mefenamic acid. A single 500 mg dose can last 12 hours. That’s why many doctors recommend it for heavy menstrual bleeding-not just pain.
A 2021 study in Obstetrics & Gynecology tracked 400 women with heavy periods. Those on naproxen reduced bleeding by 35% on average over three cycles. Mefenamic acid reduced it by 28%. Not a huge gap, but naproxen’s longer duration meant fewer pills per day. It’s also available as a 250 mg tablet, so you can start low and adjust.
But naproxen isn’t for everyone. It carries a slightly higher risk of cardiovascular events than ibuprofen in long-term users. If you’re under 30 and only use it for a few days a month, the risk is tiny. But if you’re over 50 or have high blood pressure, talk to your doctor first.
Paracetamol: is it worth trying?
Paracetamol (acetaminophen) doesn’t touch prostaglandins. It works in the brain to reduce pain signals. That means it’s gentler on your stomach and kidneys. If you’ve had stomach ulcers or take blood thinners, paracetamol is often the safest first choice.
But here’s the catch: it doesn’t work as well for cramps. A 2022 Cochrane review found that while paracetamol helped mild menstrual pain, it was significantly less effective than NSAIDs like mefenamic acid or ibuprofen for moderate to severe cramps. If your pain is light and you just need something gentle, go for paracetamol. If you’re doubled over, you’ll probably need something stronger.

Are there non-NSAID options?
Yes-and they’re worth considering if NSAIDs aren’t working or cause side effects.
Combined oral contraceptives (COCs) are the most studied alternative. They stop ovulation, which drops prostaglandin production. A 2023 review in Fertility and Sterility showed that women on COCs reported 60% less menstrual pain after three months. Plus, they reduce bleeding and can help with acne or PMS. But they’re not for everyone-especially if you smoke, are over 35, or have migraines with aura.
Progestogen-only pills or IUDs like Mirena can also help. Mirena releases levonorgestrel directly into the uterus, thinning the lining and reducing pain. Studies show up to 80% of users report lighter, less painful periods after one year. It’s a long-term solution, not a quick fix.
Heat therapy isn’t a pill, but it’s backed by solid science. A 2020 trial in BJOG found that a heating pad applied for 30 minutes was as effective as ibuprofen for cramp relief. Many women use both together: heat for immediate comfort, and a pill for longer-lasting control.
What about natural or herbal options?
People swear by ginger, turmeric, or magnesium. Some studies back them up. Ginger capsules (250 mg four times a day) were shown in a 2015 trial to reduce menstrual pain as effectively as mefenamic acid. Magnesium (360 mg daily) helped in another study, especially for women with low levels.
But here’s the problem: supplements aren’t regulated like drugs. The amount of active ingredient can vary wildly between brands. A 2024 UK study found that 38% of herbal products labeled as "ginger extract" contained less than half the claimed dose. If you try them, choose brands with a BPA or GMP certification. Don’t skip your doctor’s advice just because something’s "natural."
Who should avoid mefenamic acid?
Don’t take Ponstel if you:
- Have had stomach ulcers or bleeding from NSAIDs
- Are allergic to aspirin or other NSAIDs
- Have severe heart failure, kidney disease, or uncontrolled high blood pressure
- Are pregnant after 30 weeks (it can harm the baby’s heart)
- Are breastfeeding (small amounts pass into milk)
If you’re over 60 or take blood thinners like warfarin, the risk of bleeding goes up. Always check with your GP or pharmacist before starting any new painkiller.
Bottom line: Which one should you choose?
There’s no single "best" painkiller for everyone. It depends on your body, your symptoms, and your medical history.
Choose mefenamic acid (Ponstel) if:
- Your cramps are severe and last longer than 8 hours
- You’ve tried ibuprofen and it didn’t help enough
- You don’t have stomach or heart issues
Choose ibuprofen if:
- You want fast relief and are on a budget
- You’re concerned about stomach side effects
- You’re using it occasionally, not long-term
Choose naproxen if:
- You have heavy bleeding along with pain
- You need fewer doses per day
- You’re healthy and under 50
Choose paracetamol if:
- You can’t take NSAIDs
- Your pain is mild
- You’re pregnant (first and second trimester)
Consider hormonal options if:
- You’ve tried painkillers and still suffer
- You want to reduce bleeding long-term
- You’re open to birth control methods
And don’t forget heat. It’s free, safe, and works. Combine it with any of the above, and you’re stacking your chances of relief.
Frequently Asked Questions
Is Ponstel stronger than ibuprofen?
Ponstel (mefenamic acid) isn’t necessarily stronger-it works differently. It may last longer and help more with heavy bleeding, but ibuprofen kicks in faster and is gentler on the stomach. For most people, ibuprofen is the better first choice unless it doesn’t work.
Can I take Ponstel and paracetamol together?
Yes, it’s safe to combine mefenamic acid and paracetamol. They work in different ways, so together they can offer better pain control. Just stick to the recommended doses: no more than 500 mg of mefenamic acid every 6 hours and no more than 1,000 mg of paracetamol every 6 hours.
How long does mefenamic acid stay in your system?
Mefenamic acid has a half-life of about 2 hours, meaning half of it leaves your body in that time. But its pain-relieving effects last 6-8 hours. Most of it is cleared within 24 hours. Don’t take it more than 7 days in a row without medical advice.
Is mefenamic acid safe for long-term use?
No. Mefenamic acid is meant for short-term relief, usually 3-7 days. Long-term use increases the risk of stomach ulcers, kidney damage, and high blood pressure. If you need pain relief every month, talk to your doctor about hormonal options or other long-term strategies.
Can I buy Ponstel over the counter in the UK?
No, mefenamic acid is a prescription-only medicine in the UK. You can’t buy Ponstel off the shelf. But ibuprofen and naproxen are available without a prescription at pharmacies. If Ponstel works for you, ask your GP for a repeat prescription.
Next steps
If you’re still in pain after trying different painkillers, don’t just keep increasing the dose. Talk to your GP. You might have endometriosis, fibroids, or another condition that needs a different approach. Keep a pain diary: note when the pain starts, how bad it is (1-10 scale), what you took, and what helped. That’s the best way to find what works for you.
And if you’re considering hormonal options, don’t assume birth control is the only path. The Mirena IUD, for example, can be inserted in under 10 minutes and lasts up to five years. Many women say it changed their lives.
There’s no shame in asking for help. Severe period pain isn’t normal-and you don’t have to live with it.





Susan Karabin
October 28, 2025 AT 17:19Heat works better than half the pills people take for cramps honestly I keep a heating pad next to my bed and just let it run all night no side effects no weird chemistry just warmth and peace
Jen Taylor
October 30, 2025 AT 10:49As someone who’s tried every NSAID under the sun-ibuprofen made me feel like I swallowed glass, naproxen gave me brain fog, but mefenamic acid? It’s the only one that lets me function without crying into my coffee. I take it with food, always, and never exceed the 7-day window. Also-magnesium glycinate at night? Game-changer for muscle tension. Don’t knock the supplements until you’ve tried a reputable brand with GMP certification. Your body isn’t a lab rat.
Shilah Lala
October 31, 2025 AT 17:19Why are we even talking about pills? The real solution is just… stop having periods. Birth control isn’t a ‘option’-it’s basic self-preservation. Also, why is everyone acting like mefenamic acid is some magic potion? It’s just another NSAID with a fancy name and a higher price tag. We’re being sold fear and confusion by Big Pharma.
Christy Tomerlin
November 2, 2025 AT 10:39Paracetamol is for people who don’t want to feel anything. If your cramps are bad enough to need meds, you owe it to yourself to go hard. Mefenamic acid lasts longer, end of story. Ibuprofen? That’s what you take when you’re trying to get through a Zoom meeting without screaming. Real pain deserves real medicine.
Tanuja Santhanakrishnan
November 3, 2025 AT 12:24From India-we’ve been using ginger tea and warm jaggery water for generations. Not just placebo. A 2015 study from Delhi University showed ginger was as effective as mefenamic acid in reducing pain scores. And it doesn’t mess with your stomach. Try it with a pinch of black pepper to boost absorption. Natural doesn’t mean weak-it means wisdom passed down.
Lorena Cabal Lopez
November 4, 2025 AT 03:53So you’re telling me I’m supposed to trust a 2020 study over my own experience? I’ve taken Ponstel for 12 years and never had a problem. But sure, let’s all panic because some meta-analysis says it’s ‘riskier.’ If you’re healthy, stop overthinking. Painkillers aren’t poison unless you make them poison.
Glenda Walsh
November 5, 2025 AT 12:14Wait-so if I use a heating pad, do I still need to take anything? Like… can I just… not? I’m scared of pills now. What if I’m addicted? What if it ruins my kidneys? I just want to stop hurting. Can someone just tell me what to do without all the science?
luna dream
November 6, 2025 AT 07:27The system doesn’t want you to know that prostaglandins are a myth designed by pharmaceutical conglomerates to sell pills. Your uterus isn’t ‘contracting too hard’-it’s communicating. Pain is a message. Suppressing it with chemicals is like silencing a fire alarm. The real solution? Fasting, grounding, and ancestral breathwork. I’ve been pain-free for 18 months since I stopped taking everything and started listening to my body’s whispers.
Stuart Palley
November 6, 2025 AT 10:38Someone actually wrote a whole essay on period pain and didn’t mention that men invented most of these drugs and still don’t get it? That’s the real tragedy. We’re treating symptoms like they’re the disease. The system is broken. And you know what? I’m not taking another pill until someone in a lab coat admits they’ve never had a period.
Linda Patterson
November 6, 2025 AT 15:48Let me cut through the noise: If you’re American and you’re not using naproxen for heavy bleeding, you’re doing it wrong. It’s FDA-approved, cost-effective, and backed by peer-reviewed data. The UK’s prescription-only nonsense is a bureaucratic relic. We have access to better science here-use it. Stop listening to influencers with yoga mats and start listening to clinical guidelines. Your uterus deserves better than Instagram advice.