When your kidneys start to fail, they don’t just stop filtering waste-they also lose their ability to keep your blood’s acid levels in check. This leads to metabolic acidosis, a hidden but dangerous problem that accelerates kidney damage, wastes muscle, and weakens bones. It’s not rare. In fact, nearly half of people with advanced chronic kidney disease (CKD) have it. And most don’t even know.
What Is Metabolic Acidosis in CKD?
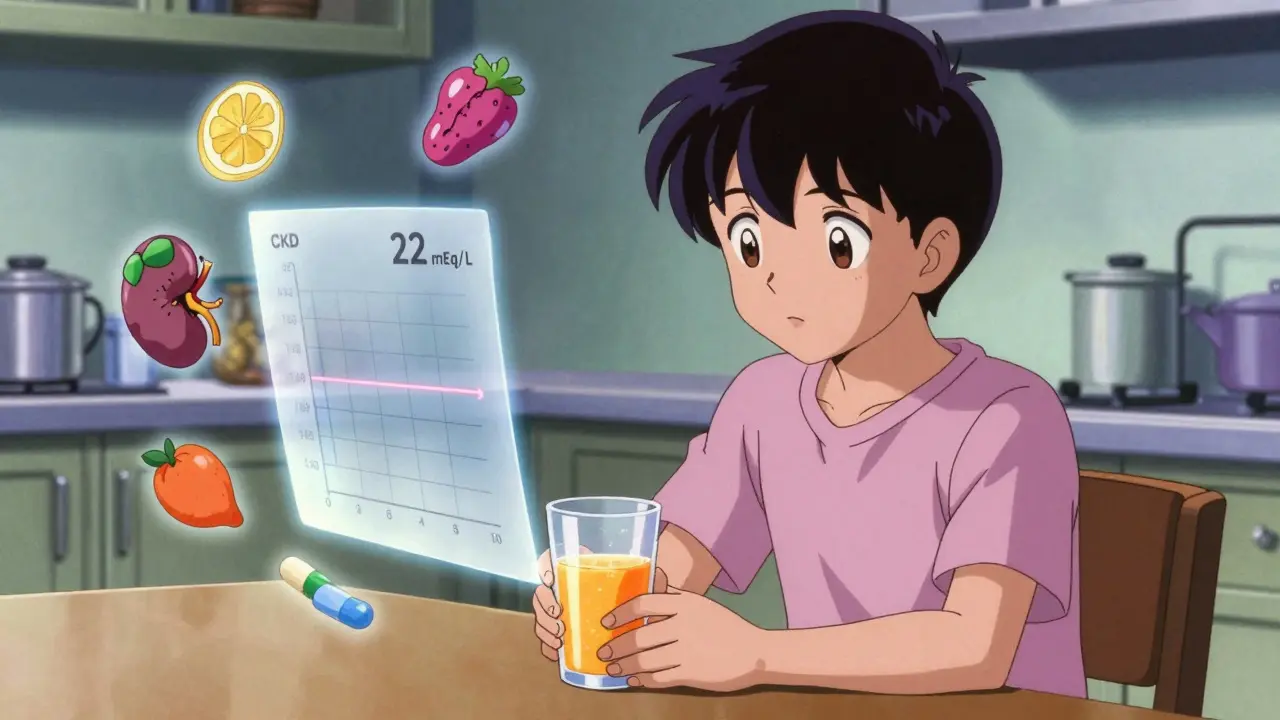
Metabolic acidosis happens when your blood becomes too acidic because your kidneys can’t get rid of acid or make enough bicarbonate to balance it. Normal blood bicarbonate is 22-29 mEq/L. When it drops below 22, you’re in acidosis. In stage 3 CKD, about 15% of people have it. By stage 5, that number jumps to 42%. It’s not just a lab value-it’s a signal your kidneys are struggling to do their most basic job: maintaining chemical balance.
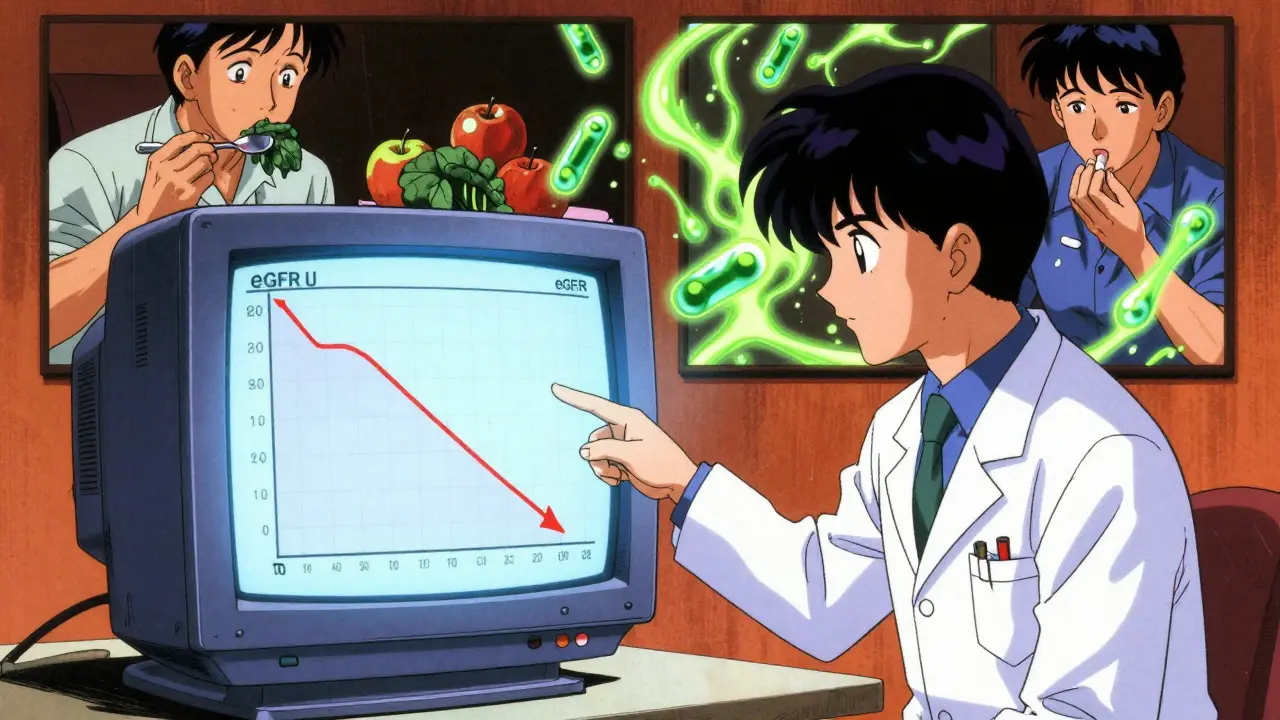
Why does this matter? Acid buildup doesn’t just sit there. It triggers a chain reaction. Your body pulls calcium from your bones to neutralize the acid, leading to osteoporosis. It breaks down muscle tissue for energy, causing weakness and fatigue. It strains your heart and raises blood pressure. And worst of all, it speeds up the decline of your kidney function. Studies show that keeping bicarbonate above 22 mEq/L cuts the risk of kidney failure by 23%.
Why Bicarbonate Therapy Is the Standard
The most common treatment is sodium bicarbonate. It’s cheap, available over the counter as baking soda, and sold in tablet form (650 mg = 7.6 mEq of bicarbonate). A major 3-year trial with 740 CKD patients found that those taking sodium bicarbonate (0.5-1.0 mEq/kg/day) slowed their kidney decline by nearly 6 mL/min/1.73m² compared to those who didn’t. That’s the difference between reaching dialysis in 5 years versus 10.
But it’s not simple. Each 500 mg tablet of sodium bicarbonate contains 610 mg of sodium. For someone with high blood pressure or heart failure, that’s risky. One study found patients on sodium bicarbonate had a 32% higher chance of being hospitalized for heart failure than those on calcium citrate. So while it works, it’s not safe for everyone.
Alternatives to Sodium Bicarbonate
If you can’t take sodium bicarbonate, there are other options-but each has trade-offs.
- Sodium citrate (Shohl’s solution): Similar to bicarbonate but less likely to cause gas or bloating. One teaspoon provides about 50 mEq of alkali. Taste is bitter, so many mix it with orange juice-which adds sugar you may need to avoid.
- Potassium citrate: Good for people with low potassium, but dangerous if your potassium is already high. Nearly 1 in 5 CKD patients on potassium supplements develop dangerous hyperkalemia (potassium >5.0 mEq/L). Guidelines now warn against using it in stages 3b-5 unless potassium is confirmed low.
- Calcium citrate: Helps with acid and gives you calcium. But too much can raise blood calcium levels, increasing kidney stone risk by 27%. Most doctors cap it at 1,000 mg of elemental calcium per day.
- Veverimer: A non-absorbed pill that traps acid in your gut. It was promising-raised bicarbonate by 4.3 mEq/L in early trials. But its final phase 3 trial in 2021 missed its goal. No FDA approval yet, though the manufacturer is re-analyzing data for a 2024 resubmission.
Dietary Changes: The Forgotten Treatment
Many people don’t realize that what you eat can be as powerful as any pill. Acid-producing foods-meat, cheese, processed grains-add 40-60 mEq of acid to your daily load. Base-producing foods-fruits and vegetables-remove acid. One study showed patients who switched to 5-9 daily servings of fruits and vegetables increased their bicarbonate by 3.5 mEq/L in six months, without any pills.
But it’s hard. A renal dietitian will help you map out your meals. For example:
- 100g of chicken = +9.5 mEq acid load
- 100g of cheddar cheese = +8.0 mEq acid load
- 100g of spinach = -2.8 mEq acid load
- 100g of apples = -2.2 mEq acid load
Getting your daily acid load below zero (PRAL score < 0) is ideal. But only 35% of patients on dietary counseling reach that goal. It takes time, coaching, and real effort.
Who Should Be Treated-and When?
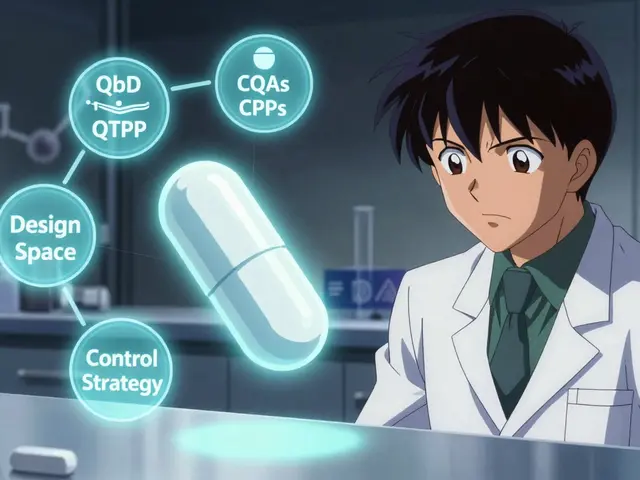
KDIGO guidelines say: Start alkali therapy when bicarbonate drops below 22 mEq/L. That’s a Grade 1B recommendation-strong, based on solid evidence. But what’s the target? That’s where things get messy.
Some experts say aim for 24-26 mEq/L. Others warn that going above 26 may raise death risk in older patients. A 2020 study found the lowest mortality happened when bicarbonate stayed between 24 and 26. For someone with heart failure, 22-24 might be safer. For someone with muscle wasting, 25-27 might help more.
Here’s what most nephrologists do:
- Check bicarbonate every 3-6 months in stable CKD.
- If it’s under 22, start with diet: add 5 servings of fruits/vegetables daily.
- If no improvement after 3 months, add oral alkali.
- Start low: 650 mg sodium bicarbonate once or twice daily.
- Monitor blood pressure, weight, and potassium every 4 weeks.
- Adjust dose to hit 23-29 mEq/L, avoiding side effects.

Why So Many Patients Go Untreated
Despite clear guidelines, only 43% of CKD patients with low bicarbonate get treatment. Why?
- Pill burden: Patients average 4.2 pills a day. That’s hard to stick to.
- Taste: Liquid forms taste awful. One patient said she had to mix baking soda with orange juice-adding sugar she shouldn’t have.
- Side effects: 29% report bloating, nausea, or cramps.
- Access: Rural patients are 30% less likely to get treatment than urban ones. Black patients are 9% less likely than White patients.
- Awareness: Many doctors still don’t check bicarbonate regularly. It’s not part of routine labs like creatinine or eGFR.
The result? Thousands of preventable kidney failures each year. The National Institute of Diabetes and Digestive and Kidney Diseases estimates correcting metabolic acidosis could prevent 28,000 cases of ESRD annually in the U.S.-and save $1.4 billion.
What’s Next?
Research is moving fast. The COMET-CKD trial, enrolling 1,200 patients, is testing high-dose versus low-dose bicarbonate. Results come in late 2025. A new citrate-free alkali supplement (TRC001) showed a 4.1 mEq/L bicarbonate boost with half the stomach upset of older forms.
KDIGO’s 2024 draft guidelines are already shifting. They’re expanding the target range to 22-29 mEq/L, acknowledging that even 22 can protect your kidneys. The future is personalization: a 75-year-old with heart failure gets a lower target than a 50-year-old with muscle loss.
But right now, the best tools we have are simple: check your bicarbonate. Eat more plants. Take your pills. Monitor your blood pressure. Don’t let a treatable condition quietly steal your kidney function.
What is the normal bicarbonate level for someone with CKD?
For people with chronic kidney disease, the target serum bicarbonate level is 23-29 mEq/L, according to KDIGO guidelines. Some experts now say 22-29 mEq/L is acceptable, especially if you have heart failure or are elderly. Levels below 22 mEq/L indicate metabolic acidosis and should be treated.
Can I just use baking soda instead of prescription bicarbonate?
Yes, one teaspoon of baking soda contains about 50 mEq of bicarbonate, which is equivalent to several prescription tablets. But it’s not recommended without medical supervision. Baking soda is pure sodium bicarbonate, so it can spike your sodium and worsen high blood pressure or heart failure. Always talk to your nephrologist before using it.
Does potassium citrate help with acidosis in CKD?
Potassium citrate can help neutralize acid, but it’s risky in CKD. About 18% of patients develop dangerous high potassium levels (hyperkalemia) on this treatment. It’s only recommended if you have low potassium (below 3.5 mEq/L) and your doctor closely monitors your levels. Most guidelines now advise against it in stages 3b-5.
How long does it take for bicarbonate therapy to slow kidney decline?
In clinical trials, patients on bicarbonate therapy showed slower kidney decline within 6-12 months. The landmark 2018 study showed a clear benefit after 3 years, with eGFR decline slowed by nearly 6 mL/min/1.73m². The key is consistency-treatment must be maintained long-term to protect kidney function.
Can diet alone fix metabolic acidosis in CKD?
Diet can help, but it’s rarely enough on its own. Eating 5-9 servings of fruits and vegetables daily can raise bicarbonate by 1-3 mEq/L. For patients with severe acidosis (bicarbonate <18 mEq/L), that’s not enough. Diet works best as a first step or combined with low-dose alkali therapy. Many patients need both.
Is there a new drug coming for metabolic acidosis in CKD?
Veverimer was the most promising new drug, but its phase 3 trial failed in 2021. The company plans to resubmit to the FDA in 2024 with new data. A new citrate-free alkali supplement (TRC001) is in early trials and shows better tolerance than current options. But as of 2026, no new FDA-approved drug is available. Sodium bicarbonate and dietary changes remain the standard.




Meghan Hammack
January 9, 2026 AT 05:28Just found out my bicarb was 20.5 after my last blood test. I started eating more spinach and apples and switched to potassium citrate after my nephrologist said it was safe. It’s been 4 months and I’m at 24. No more muscle cramps at night. I know it’s not magic, but it’s something.
Also, I mix baking soda with unsweetened cranberry juice. Tastes like a science experiment, but it works.
Lindsey Wellmann
January 11, 2026 AT 01:52OMG I’m literally crying rn 🥹 I’ve been on sodium bicarbonate for 2 years and my nephrologist told me I’m ‘lucky’ to not be on dialysis yet. I thought I was just ‘getting older.’ Turns out I was being poisoned by my own kidneys and no one told me. This post is a GAME CHANGER. I’m sharing this with my entire family. THANK YOU.
Ian Long
January 12, 2026 AT 21:34Look, I get the hype around bicarbonate. But let’s not pretend this is a cure-all. I’ve seen patients on high-dose alkali develop edema, hypertension, and then get hospitalized. The real issue isn’t the acid-it’s the system. We’re treating lab values instead of people. If you’re eating processed food, smoking, and sitting all day, no pill is gonna save you.
Also, why is no one talking about the cost? A month of veverimer would cost more than my rent.
Pooja Kumari
January 14, 2026 AT 16:40I’m from India and I’ve been watching this whole thing unfold with so much emotion. In my village, people think CKD is just ‘weak kidneys’ and drink sugary chai all day. No one checks bicarbonate. My aunt died at 58 from ESRD and they never even ran the test. I cried for days.
And now I see here in the US, people are debating doses and sodium content like it’s a math problem. But in my country, they don’t even have the labs. This isn’t just medicine-it’s justice. We need global access to cheap alkali therapy. Not just for the privileged with insurance. My heart is breaking.
Also, I’ve started eating 10 servings of papaya and banana daily. My cousin says I look ‘less yellow.’ I don’t know what that means but I’m taking it as a win.
Angela Stanton
January 14, 2026 AT 23:42Let’s cut through the noise. The 2018 bicarbonate trial had a 6 mL/min/1.73m² difference? That’s statistically significant but clinically marginal. The number needed to treat to prevent one dialysis event is 18. Meanwhile, the sodium load increases heart failure risk by 32%.
And don’t get me started on dietary PRAL scores. You’re telling me a 72-year-old with dementia and no teeth is gonna hit a PRAL < 0 by eating 9 servings of kale? That’s not medicine, that’s performative nutritionism.
Also, veverimer failed phase 3. Why are we still talking about it like it’s coming next year? Marketing.
Johanna Baxter
January 15, 2026 AT 16:32Why is everyone so obsessed with pills? I used baking soda in my coffee for 3 months. My BP went through the roof. My doctor said I was ‘a walking emergency.’ Now I eat 3 oranges a day and I feel like a new person. No pills. No drama. Just fruit. Stop overcomplicating your health.
Also, if you’re not eating plants, you’re just feeding your kidneys to the wolves. End of story.
Jerian Lewis
January 15, 2026 AT 21:10My father died of CKD at 67. He never knew his bicarb was low. The doctor said his creatinine was ‘fine.’ That’s the problem. We treat numbers, not people. If we had checked bicarbonate early, he might have had 5 more years. I’m not angry. Just… tired. This system is broken.
Kiruthiga Udayakumar
January 17, 2026 AT 19:25Hey everyone, I’m a nurse in Kerala and I’ve seen this over and over. People come in with swollen legs and say, ‘I’m just tired.’ We check bicarb-20. They’re shocked. We give them potassium citrate and tell them to eat bananas. Two weeks later, they’re walking again. It’s not rocket science. It’s basic care.
Why does the US make it so complicated? Just give them the pills. And the fruit. And the education. Not all of us have fancy trials and $300 supplements.
Patty Walters
January 17, 2026 AT 23:13Hi, I’m a renal dietitian. I’ve helped over 200 CKD patients with acidosis. Here’s what actually works: start with diet. Add one extra serving of veggies per day. Wait 6 weeks. Recheck bicarb. If it’s still under 22, add 650mg sodium bicarbonate once daily. Don’t go over 1300mg/day. Monitor BP and weight weekly.
Most people don’t need potassium citrate. Most people don’t need veverimer. They need someone to sit with them and say, ‘Let’s make this simple.’
Also, if you’re using baking soda, use a measuring spoon. One teaspoon = 6 grams of sodium. That’s more than your daily limit.
Maggie Noe
January 18, 2026 AT 07:26Isn’t it strange that we treat acidosis like a disease to be fixed, when it’s really a symptom of a broken relationship between our bodies and our environment? We’ve engineered food to be acidic, sedentary, and processed. We’ve made medicine about dosing pills instead of restoring balance.
Maybe the real question isn’t ‘how do we raise bicarbonate?’ but ‘how do we stop poisoning ourselves in the first place?’
Also, I’ve been eating a lemon wedge with salt every morning. It’s not science. It’s ritual. And it feels like healing.
Gregory Clayton
January 19, 2026 AT 01:12Look, I don’t care what the ‘guidelines’ say. If you’re American and you’re on dialysis, it’s because you gave up. I’ve seen guys on this forum say they ‘can’t afford’ the pills. Bro, you bought a new phone and 3 energy drinks today. Pick your poison.
Also, if you’re eating fruit instead of taking your meds, you’re not ‘natural’-you’re just irresponsible. This isn’t yoga class. This is medicine.
Alicia Hasö
January 19, 2026 AT 11:06To anyone reading this and feeling overwhelmed: you’re not alone. I was diagnosed with stage 4 CKD last year. I didn’t know what bicarbonate was. Now I track my meals, I eat my greens, I take my 650mg tablets, and I check my numbers every month.
I’m not cured. But I’m alive. And I’m not giving up. You don’t need to be perfect. Just show up. One apple. One pill. One day at a time.
You’ve got this. I believe in you.
Drew Pearlman
January 21, 2026 AT 09:04I’ve been on sodium bicarbonate for 5 years now. Started at 19.8, now I’m at 25.5. I’ve lost 40 pounds, stopped needing my cane, and I walk my dog every morning. I didn’t do it because of a study. I did it because my daughter said, ‘Mom, I don’t want to lose you.’
The pills taste like chalk. The diet is boring. But I do it anyway. Not for the numbers. For the mornings. For the walks. For the quiet.
And if you’re thinking ‘I can’t do this’-you already are. You’re reading this. That’s the first step.
Chris Kauwe
January 23, 2026 AT 00:48The entire paradigm of CKD management is rooted in reductionist biomedicine. We treat bicarbonate as a variable, not a systemic biomarker of metabolic dysregulation. The real intervention isn’t alkali-it’s epigenetic reprogramming through circadian-aligned, phytonutrient-dense, low-glycemic, whole-food, plant-predominant diets.
Also, the sodium bicarbonate trials are confounded by industry funding. The real solution is ancestral nutrition. Eat like your grandparents. No pills. No science. Just food.
RAJAT KD
January 23, 2026 AT 21:25My dad had CKD. He took sodium bicarbonate. His BP went up. He got hospitalized. We switched to potassium citrate. His K+ spiked. He died.
Don’t treat numbers. Treat people. And listen to them.
That’s all.