When a sprain, strain, or post‑surgical wound leaves you on the couch, the path back to full movement often feels foggy. That’s where physiotherapy steps in - a hands‑on, science‑based approach that turns a painful setback into a structured recovery.
What Injury Rehabilitation Really Means
Injury rehabilitation is the process of restoring strength, range of motion, and function after tissue damage. It isn’t just “waiting for it to heal”; it’s an active collaboration between the patient, the physiotherapist, and any other health professionals involved.
Rehabilitation goals differ by injury type - a torn rotator cuff needs gradual loading, while a fractured wrist needs protection followed by gentle mobilization. Yet every plan shares three core pillars: assessing the current state, prescribing targeted interventions, and monitoring progress.
Physiotherapy’s Core Contributions
Physiotherapists bring a blend of assessment skills, therapeutic techniques, and patient education that sets them apart from generic “rest and ice” advice.
- Assessment expertise: Using tools like goniometers, manual muscle testing, and functional movement screens, they pinpoint deficits that aren’t obvious to the layperson.
- Tailored interventions: Whether it’s hands‑on mobilization or a home‑based exercise program, each action is selected to match the tissue healing stage.
- Education & empowerment: Patients learn how to move safely, modify activities, and prevent re‑injury, which dramatically lowers recurrence rates.
These contributions translate into faster recovery times, reduced pain, and fewer future injuries.
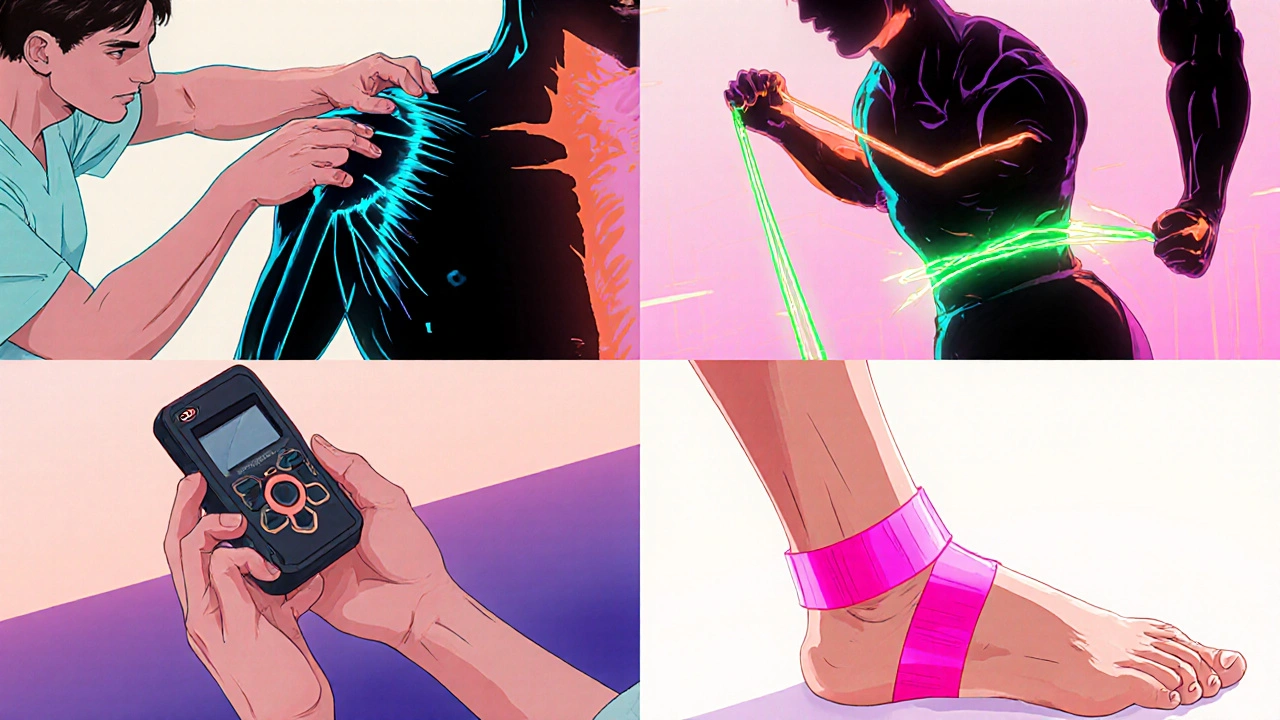
Key Techniques Physiotherapists Use
Below are the most common modalities you’ll encounter during a rehab journey.
- Manual therapy: Joint mobilisations, soft‑tissue massage, and myofascial release restore tissue elasticity and improve circulation.
- Exercise therapy: Progressive resistance training, functional drills, and proprioceptive exercises rebuild strength and coordination.
- Electrotherapy: TENS, ultrasound, and electrical muscle stimulation help manage pain and stimulate tissue repair.
- Therapeutic taping: Kinesiology tape provides support while allowing movement, useful for swelling control.
- Patient education: Instruction on posture, ergonomics, and activity pacing empowers self‑management.
Each technique is chosen based on the injury’s phase - acute, sub‑acute, or chronic - and the patient’s individual needs.
Matching Injuries with Physiotherapy Approaches
| Injury Type | Typical Healing Phase | Key Physiotherapy Techniques |
|---|---|---|
| Acute ankle sprain | 0‑7 days | Manual therapy (soft‑tissue mobilization), cryotherapy, low‑intensity exercise, taping |
| Rotator cuff tear (post‑surgery) | Weeks 3‑12 | Passive range‑of‑motion, scapular stabilisation exercises, gradual resistance training |
| Hamstring strain | 2‑6 weeks | Gentle stretching, eccentric strengthening, neuromuscular drills |
| Chronic low back pain | Ongoing | Core stabilisation, manual therapy, education on posture, electrotherapy for pain modulation |
| Post‑knee replacement | Weeks 1‑12 | Early mobilisation, progressive resistance, gait training, edema management |
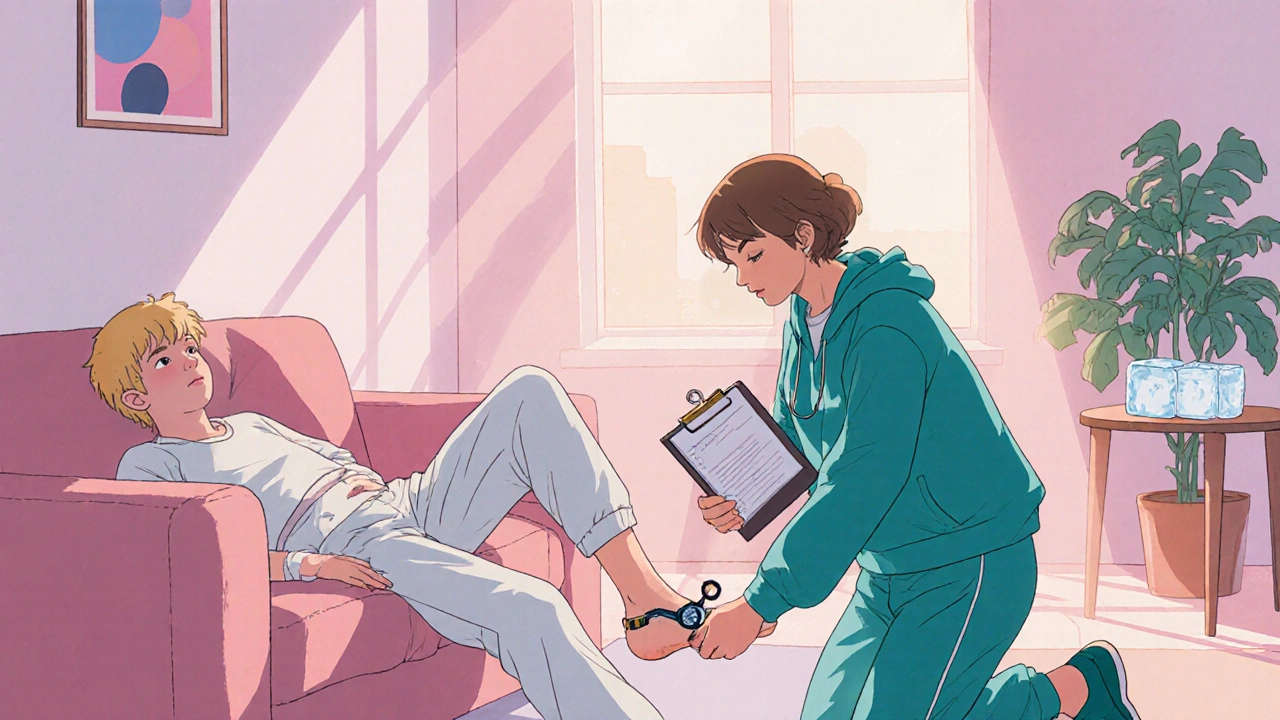
Designing a Personalized Rehab Plan
Every recovery program follows a simple three‑step framework.
- Initial assessment: The physiotherapist records baseline measurements - range of motion, strength grades, pain scores, and functional limits.
- Goal setting: Short‑term goals (e.g., “walk pain‑free 20 m”) and long‑term goals (e.g., “return to sport at pre‑injury level”) are written down and revisited weekly.
- Intervention schedule: A weekly calendar outlines clinic sessions, home‑exercise frequency, and progress checkpoints.
Consistency matters. Research from the British Journal of Sports Medicine (2022) shows patients who adhered to a physiotherapist‑prescribed exercise program recovered 30 % faster than those who followed generic advice.

Common Pitfalls and How to Avoid Them
Even with a solid plan, certain habits can stall progress.
- Skipping pain‑free movement checks: If an exercise triggers sharp pain, it’s a sign to modify the load or technique.
- Over‑reliance on passive modalities: Machines like ultrasound help, but they don’t replace active movement. Use them as adjuncts.
- Neglecting cardio fitness: Low‑impact cardio (e.g., stationary bike) maintains endurance while protecting the injured area.
- Ignoring ergonomics at home or work: Adjusting workstation height or footwear can prevent compensation patterns that cause new injuries.
Addressing these issues early keeps the rehab trajectory smooth.
Measuring Progress and Knowing When to Advance
Objective metrics keep both patient and therapist on the same page.
- Pain scales (0‑10 numeric rating) recorded after each session.
- Range of motion measured in degrees with a goniometer.
- Strength testing using manual muscle testing or handheld dynamometers.
- Functional tests such as single‑leg hop distance or timed up‑and‑go.
When a metric reaches 80‑90 % of the unaffected side or the patient reports minimal pain during the targeted activity, it’s usually safe to increase load or introduce sport‑specific drills.
Frequently Asked Questions
How soon after an injury should I see a physiotherapist?
Ideally within 48‑72 hours. Early assessment helps reduce swelling, prevent maladaptive movement patterns, and set a clear recovery roadmap.
Do I need equipment for home exercises?
Most programs start with body‑weight moves. As you progress, a resistance band, dumbbell, or medicine ball can add load, but your therapist will guide you on what’s needed.
Can physiotherapy help chronic conditions like low‑back pain?
Absolutely. For chronic pain, physiotherapists focus on core stability, posture correction, and pain‑modulating techniques to break the pain‑cycle.
Is it safe to exercise while still in pain?
A mild, tolerable ache during controlled movement is normal, but sharp or increasing pain signals you should stop and check with your therapist.
How long does a typical physiotherapy program last?
Program length varies by injury severity - from 2‑3 weeks for minor sprains to 12‑16 weeks for post‑surgical rehab. The therapist will outline milestones and expected timelines.


Drew Waggoner
October 18, 2025 AT 14:52Reading through this guide felt like walking out of a foggy room into bright daylight, and the gratitude that surged through me was almost overwhelming. The way physiotherapy is presented here captures the intricate dance between science and human touch, reminding me why I turned to rehab after that brutal ankle sprain. Every sentence echoed the echoing pulse of a heart that refuses to stay still, craving movement and progress. I could almost hear the therapist’s voice encouraging each tiny range‑of‑motion stretch, a whisper that said, "You’re not broken, just healing." The description of manual therapy made me recall the subtle release of tension, like a sigh escaping after a long hold. When the article mentioned electrotherapy, I imagined tiny currents of hope pulsing through fatigued fibers, nudging them back to life. The emphasis on education struck a chord; knowledge is the lantern we carry through the darkest nights of pain. I was moved by the statistics showing a 30 % faster recovery, a number that felt like a promise rather than just a data point. The practical guide on goal‑setting resonated deeply, as I have always believed that clear milestones are the scaffolding of success. The caution against over‑reliance on passive modalities reminded me of the dangerous lull of complacency, a trap I once fell into. I appreciated the reminder to blend cardio fitness with rehab, as the rhythm of a stationary bike can become a metronome for recovery. The table of injuries and techniques read like a map for a traveler lost in a forest, offering direction and safety. The section on measuring progress felt like a compass, pointing the way home with numbers and tests. I cannot stress enough how the blend of empathy and rigor in physiotherapy can transform a setback into a comeback. In short, this guide is not just information; it is an invitation to reclaim our bodies with courage and science.
Liberty Moneybomb
October 20, 2025 AT 00:12The whole "science‑based" narrative is just the latest PR spin from the corporate physiotherapy lobby, secretly funded by equipment manufacturers eager to sell more ultrasound machines. They conveniently gloss over how many of these modalities were invented in secret labs hidden from public scrutiny. While you praise manual therapy, you ignore the fact that many practitioners are paid per session, incentivizing longer treatment plans. The guide’s soothing tone masks a deeper agenda: to keep us dependent on a costly, profit‑driven industry. Remember, the same clinics that promote early mobilization also sell expensive braces that they claim are essential for recovery.
Alex Lineses
October 21, 2025 AT 09:32Great rundown! I'd like to add that when we talk about progressive overload, it's crucial to monitor the load‑velocity relationship to avoid overload injury. Incorporating proprioceptive neuromuscular facilitation (PNF) stretching can augment the tissue remodeling phase, especially after acute inflammation subsides. Don't forget to periodize the exercise therapy, alternating between hypertrophy, strength, and power blocks to optimize musculoskeletal adaptation. For patients with chronic low back pain, integrating core stabilization drills using the McGill Big‑3 can dramatically improve segmental control. Lastly, always reassess with the goniometer every two weeks to track joint angle gains and adjust the prescription accordingly.
Brian Van Horne
October 22, 2025 AT 18:52The protocol delineated aligns precisely with evidence‑based standards.
James Mali
October 24, 2025 AT 04:12Physiotherapy, in its essence, mirrors the philosophical journey of self‑discovery: we confront pain, we question limits, and we emerge transformed. Yet the modern clinical setting often reduces this odyssey to checklists and metrics, stripping away the poetry of movement. One might argue that the true art lies in balancing the empirical with the experiential. Still, it's fascinating how a simple band of elastic can become a symbol of resilience. In the end, perhaps the greatest therapy is the belief that we can heal.
Janet Morales
October 25, 2025 AT 13:32Let's cut the fluff and get real: if you skip the prescribed regimen, you’re basically sabotaging your own recovery. The guide sounds nice, but people need to hear that dedication beats excuses every single time. Don't be fooled by the gentle language; this is a battle against stagnation, and the physiotherapist is your commander. You either follow the plan or you stay stuck in pain. So gear up, commit, and watch the results speak for themselves.
Albert Fernàndez Chacón
October 26, 2025 AT 21:52I totally agree with the emphasis on patient education – it empowers folks to take charge of their own healing. When you break down the exercises into simple steps, adherence skyrockets. Also, using clear language helps bridge the gap between therapist and client, making the rehab journey less intimidating. Remember to check in on pain levels regularly; it's the compass that guides progression. Keep the communication open, and the outcomes will follow.
Poornima Ganesan
October 28, 2025 AT 07:12While Alex provides a solid technical overview, the guide neglects to address the biomechanical chain reactions that underlie many of these injuries. For instance, a rotator cuff tear is often a symptom of scapular dyskinesis, yet no mention is made of correcting that upstream flaw. Moreover, the recommendation to use TENS overlooks its limited evidence base for long‑term functional gains. A more holistic approach would integrate movement pattern analysis early on, preventing compensations before they manifest. Finally, consider incorporating functional movement screening to tailor interventions more precisely.
Emma Williams
October 29, 2025 AT 16:32Totally on board with Janet’s point – commitment is key.
Stephanie Zaragoza
October 31, 2025 AT 01:52While the emotive language employed by Drew is undoubtedly engaging, one must critique the occasional lack of precise quantification; for instance, stating “almost overwhelming” could be replaced with a metric such as a 30‑percent improvement in functional scores, thereby enhancing the scientific rigor of the narrative. Additionally, the juxtaposition of anecdotal descriptions with statistical claims could benefit from clearer source attribution to avoid conflating subjective experience with empirical evidence.
Rajesh Singh
November 1, 2025 AT 11:12In the grand tapestry of healthcare, physiotherapy stands out as a beacon of ethical responsibility, reminding us that healing is not a commodity but a moral duty. The guide rightly underscores the synergy between manual techniques and patient empowerment, yet we must also acknowledge the societal structures that often limit access to such services. It is incumbent upon us, as informed citizens, to advocate for broader insurance coverage and community‑based programs that democratize rehabilitation. When we champion equitable access, we honor the very essence of compassionate care. Let us, therefore, transform knowledge into action, ensuring that no individual is left languishing in pain due to systemic neglect.