Gout Medication Selection Tool
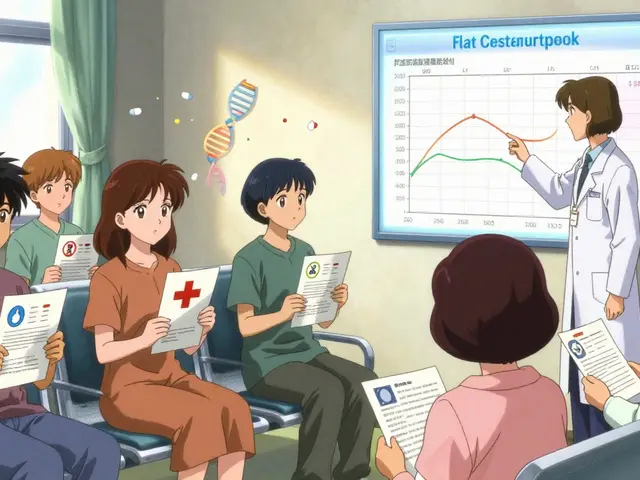
This tool helps you determine which gout medication might be most appropriate based on your kidney function, cardiovascular risk, and current medications.
Quick Takeaways
- Allopurinol is a xanthine oxidase inhibitor that lowers uric acid production, making it a first‑line drug for chronic gout.
- Febuxostat offers similar efficacy with a lower dose‑adjustment burden in mild‑to‑moderate renal impairment.
- Probenecid works by increasing uric acid excretion; it’s useful when uric acid production is already low.
- Lesinurad and topiroxostat are newer options that target uric acid transporters or enzyme activity, respectively, but have limited long‑term safety data.
- Choosing the right drug depends on kidney function, cardiovascular risk, drug‑interaction profile, and cost considerations.
When treating gout, Allopurinol is a xanthine oxidase inhibitor that reduces uric acid synthesis. It has been the backbone of chronic gout management for decades, yet a growing list of alternatives now competes for the same therapeutic niche. This guide walks you through the science, the safety profiles, and the practical trade‑offs so you can decide which option fits your situation best.
What Is Allopurinol and How Does It Work?
Allopurinol blocks the enzyme xanthine oxidase, which converts hypoxanthine and xanthine into uric acid. By curbing this final step, plasma urate levels fall, preventing crystal formation in joints and soft tissues. The typical starting dose is 100mg once daily, titrated up to 300mg (or 400mg in some cases) based on serum urate targets (<6mg/dL). For patients with severe renal impairment, the dose is reduced to 50‑100mg daily.
Common side effects include rash, elevated liver enzymes, and, rarely, allopurinol hypersensitivity syndrome-a severe reaction that demands immediate cessation of the drug. Monitoring liver function and renal labs every 2‑4weeks during dose escalation is standard practice.
Key Alternatives to Allopurinol
Below are the most frequently considered alternatives, each with a distinct mechanism.
Febuxostat is a non‑purine selective xanthine oxidase inhibitor. It achieves comparable urate lowering at doses of 40‑80mg daily and requires minimal dose adjustment for mild‑to‑moderate renal dysfunction.
Probenecid is a uricosuric agent that blocks renal tubular reabsorption of uric acid, increasing its excretion. It is best used in patients with good kidney function (eGFR>50mL/min) and in those who have not responded to uric‑acid‑production inhibitors.
Lesinurad is a selective uric acid transporter (URAT1) inhibitor used in combination with a xanthine oxidase inhibitor. The usual dose is 200mg daily, added to an existing Allopurinol or Febuxostat regimen.
Topiroxostat is another xanthine oxidase inhibitor approved in Japan, showing similar potency to Allopurinol. It is still gaining regulatory approval worldwide, so data are limited.

Side‑Effect Profiles at a Glance
| Drug | Mechanism | Typical Dose | Renal Adjustment | Key Side Effects | UK Cost (approx.) |
|---|---|---|---|---|---|
| Allopurinol | Xanthine oxidase inhibitor | 100‑300mg/d | Yes, reduce if eGFR<30 | Rash, hepatic ↑, hypersensitivity | £2‑£5 per month |
| Febuxostat | Selective xanthine oxidase inhibitor | 40‑80mg/d | Minimal | Cardiovascular events, liver ↑ | £30‑£45 per month |
| Probenecid | Uricosuric (URAT1 blocker) | 250‑500mg 2‑3×/d | Not recommended | Kidney stones, GI upset |
£5‑£8 per month |
|
| Lesinurad | URAT1 inhibitor (add‑on) | 200mg/d (with XO‑inhibitor) | Reduce to 200mg if eGFR30‑50 | Renal toxicity, rash | £25‑£35 per month |
| Topiroxostat | Xanthine oxidase inhibitor | 30‑60mg/d | Limited data | Elevated liver enzymes | £20‑£30 per month (est.) |
When to Choose Allopurinol vs. an Alternative
Allopurinol remains the first‑line choice for most patients because of its long‑track record, low price, and broad safety data. However, specific clinical scenarios tip the balance toward an alternative:
- Renal impairment: If eGFR is 30‑60mL/min, febuxostat often achieves target urate without aggressive dose reduction.
- Cardiovascular risk: Some studies link febuxostat to higher cardiovascular events, making allopurinol or probenecid safer for high‑risk patients.
- Allopurinol hypersensitivity: In patients with a history of rash or severe reaction, switching to febuxostat or a uricosuric agent is prudent.
- Uricosuric advantage: When underexcretion of uric acid is the primary problem (identified via 24‑hour urine collection), probenecid or lesinurad can be more effective.
- Cost constraints: Allopurinol is the cheapest; patients on limited budgets often stay on it unless side‑effects force a switch.
Step‑by‑Step Checklist for Switching from Allopurinol
- Confirm target serum urate (<6mg/dL) and document current dose.
- Assess renal function (eGFR) and liver enzymes.
- Identify the reason for switching (e.g., hypersensitivity, inadequate control, renal dose‑limit).
- Select the new agent based on the decision matrix above.
- Overlap therapy: start the new drug at a low dose while tapering Allopurinol over 1‑2weeks to avoid flare‑ups.
- Schedule follow‑up labs at 2‑4weeks to verify urate reduction and monitor for adverse events.
- Educate the patient on signs of severe rash, hepatic symptoms, or kidney stones, and provide an emergency contact.
Practical Tips for Clinicians and Patients
- Always start prophylactic colchicine or NSAIDs when initiating or changing urate‑lowering therapy to prevent acute gout attacks.
- Use the 24‑hour urine uric acid test to differentiate over‑production vs. under‑excretion patterns.
- Check for drug‑drug interactions: probenecid can increase plasma levels of penicillins and ceftriaxone; febuxostat may interact with azathioprine.
- Consider genetic testing for HLA‑B*58:01 in patients of Asian descent before starting Allopurinol, as they have a higher risk of hypersensitivity.
- For patients on dialysis, low‑dose Allopurinol (50mg) is often sufficient; alternatives generally require intact renal clearance.
Frequently Asked Questions
Can I take Allopurinol and Febuxostat together?
No. Both drugs inhibit xanthine oxidase, so combining them offers no added benefit and raises the risk of liver toxicity.
What is the fastest way to lower uric acid?
Starting a low dose of colchicine or a short course of NSAIDs while initiating a urate‑lowering drug provides rapid symptom control. The drug itself takes 2‑4weeks to reach steady‑state urate reduction.
Is Probenecid safe for people with kidney stones?
Probenecid can increase urine uric acid concentration, potentially triggering stone formation. It should be avoided in patients with a history of uric acid stones unless adequate hydration is ensured.
How often should serum urate be checked after switching medication?
Check at 2‑4weeks, then every 3‑6months once the target is stable.
Are there any dietary changes that complement medication?
Limit high‑purine foods (red meat, seafood), avoid excessive alcohol, stay hydrated, and consider a low‑fructose diet to reduce urate production.
Bottom Line
The choice between Allopurinol and its alternatives hinges on kidney function, cardiovascular health, cost, and personal tolerance. Allopurinol stays the go‑to drug for most, but febuxostat shines when renal dose‑adjustments become cumbersome, and probenecid offers a useful uricosuric route for select patients. Lesinurad and topiroxostat expand the toolbox but require careful monitoring. By matching drug properties to patient specifics, clinicians can achieve sustained urate control with minimal side effects.




Sara Werb
October 17, 2025 AT 14:18Listen up-this WHOLE MEDICNE saga isn’t just about chemistry; it’s a battle of loyalties and hidden agendas!!! They don’t want you to know that the pharma giants are secretly swapping Allopurinol with experimental concoctions under the guise of “new alternatives”!!! The FDA? A puppet. The data? Fabricated. Wake up!!!
Russell Abelido
October 18, 2025 AT 17:06We’re all walking that painful road of gout, and every pill we swallow is a story of hope and struggle. I feel the weight of each dose, the anxiety of side‑effects, and the yearning for a life without that burning flare‑up. Allopurinol has been a steadfast companion for many, yet it’s okay to explore the newer options when they align better with our bodies. Let’s remember that medicine is as personal as a diary entry, and the best choice respects both science and our individual rhythm 😊. Stay curious, stay kind to yourself.
Steve Holmes
October 19, 2025 AT 20:53Hey folks, I’m trying to piece together the renal‑adjustment guidelines-does anyone have a clear chart that lines up eGFR thresholds with the recommended Allopurinol dose??? Also, how do the newer agents like Lesinurad fit into that algorithm when kidney function is borderline??? I’ve seen mixed advice on whether to combine, and I’d love a consolidated view!!!
Tom Green
October 19, 2025 AT 22:16Great questions, Steve! The key is to start low and go slow-if eGFR is below 30 mL/min, many clinicians cap Allopurinol at 100 mg and titrate cautiously. Lesinurad, on the other hand, is usually added only after a stable xanthine oxidase inhibitor is in place, and you’ll want to watch for nephrolithiasis. Think of it like building a house: solid foundation first, then add the decorative layers.
Emily Rankin
October 21, 2025 AT 00:40When we look at the landscape of gout therapy, it feels like a sunrise after a long night-every new drug is a ray of light breaking through the clouds of chronic pain. Allopurinol gave us stability, but Febuxostat and even experimental agents like Topiroxostat show us that progress never stops. Embrace the options, weigh the risks, and let your body guide you toward that brighter, pain‑free horizon.
Rebecca Mitchell
October 22, 2025 AT 04:26Just switch to febuxostat if you hate allergies.
Roberta Makaravage
October 22, 2025 AT 05:50Honestly, Emily, the “sunrise” metaphor is cute, but let’s get real: the evidence shows that Febuxostat carries a higher cardiovascular risk in certain populations, a fact the marketing glosses over 😊. If you’re aiming for optimal safety, stick with Allopurinol unless your urate levels are stubbornly high despite max dosing. Remember, not every “new” is better, and the FDA’s warnings are there for a reason.
genevieve gaudet
October 23, 2025 AT 08:13I gotta say, reading through this whole compare‑and‑contrast feels like flipping through a messy kitchen recipe book where the chef forgot to write down the measurements. First off, Allopurinol has been the grandpa of gout meds, sitting on the porch and watching the younger drugs try to steal his thunder. But the thing is, the kidney thingy-eGFR-makes everything more complicated than a soap opera plot twist. When your kidneys are low, you cant just crank the dose like a volume knob; you have to turn it down and hope the uric acid still goes down. Febuxostat comes in looking all shiny, promising fewer dose adjustments, yet the studies whisper about heart issues that most brochures ignore. Probenecid is a neat trick, making the body throw out more acid, but it only works if you’re not already making too much. Lesinurad tries to hijack the urate transporter, kinda like a traffic cop redirecting cars, but the long‑term safety data is still a mystery. Topiroxostat is like the secret menu item you only hear about in Japan, and we’re still waiting for the rest of the world to taste it. Cost wise, the UK numbers show Allopurinol is cheap, while the newer guys can feel like a splurge at a fancy coffee shop. From a patient perspective, the choice often boils down to side‑effects, how your doctor monitors you, and whether you can afford the meds. If you’ve had a rash with Allopurinol, switching to Febuxostat might save you from a skin nightmare. On the other hand, if you have a history of heart disease, you might want to stick with the old reliable or at least discuss the risks with your cardiologist. The combination therapies, like Allopurinol plus Lesinurad, are tempting but you have to watch for kidney stones, which are a painful surprise. In practice, many rheumatologists start low, go slow, and keep checking serum urate every few months. Ultimately, there’s no one‑size‑fits‑all, and the best plan is a conversation between you, your doctor, and maybe even a pharmacist. So keep reading, keep questioning, and don’t let the pharma hype drown out the real data that matters to your health.
Patricia Echegaray
October 24, 2025 AT 12:00Ever notice how every “new” gout drug pops up just when the big pharma lobby is lobbying for fresh patents? It’s like they’re playing a chess game with our kidneys-moving pieces, hiding attacks, and calling it “innovation.” The “research” behind Lesinurad’s safety feels more like a smoke‑filled room where the fire alarm is turned off. If you ask me, the only real freedom is sticking with what’s been battle‑tested, unless you want to be a pawn in their profit‑driven scheme.
Samantha Oldrid
October 24, 2025 AT 13:23Oh sure, because sticking to old drugs is the ultimate act of rebellion.