Bleeding Risk Calculator for Cosmetic Procedures
Your Situation
Based on guidelines from the American Society of Dermatologic Surgery and British Society of Dermatologists
Stopping blood thinners can increase clot risk by 40-50% compared to continuing therapy
Why Your Blood Thinners Matter More Than You Think Before a Cosmetic Procedure
If you're taking blood thinners-whether it's warfarin, apixaban, rivaroxaban, or even daily aspirin-and you're thinking about getting a cosmetic procedure, you're not alone. Around 25 to 40% of people undergoing facial or skin procedures in the UK and US are already on these medications because of heart conditions, atrial fibrillation, or past blood clots. The big question isn't whether you should stop them. It's whether stopping them could be more dangerous than keeping them.
For years, the default advice was simple: stop your blood thinners before any surgery. But that advice is outdated. In fact, stopping them can lead to strokes, heart attacks, or even death. A 2014 survey of 168 Mohs surgeons found 46 serious blood clot events after patients stopped their medications, including three deaths. Most of those happened after warfarin or aspirin was paused. Meanwhile, the risk of serious bleeding during a minor cosmetic procedure like a mole removal or eyelid lift is tiny-often less than 2%-even if you keep taking your meds.
Not All Blood Thinners Are the Same
When doctors talk about blood thinners, they mean three different kinds of drugs, and each behaves differently in your body.
- Warfarin is the old-school option. It needs regular blood tests (INR checks) to make sure your blood isn’t too thin. If your INR is under 3.5, most experts agree you can safely keep taking it for minor procedures. But if your INR is higher, your risk of bruising and bleeding goes up. Studies show warfarin users are nearly four times more likely to have bleeding complications during facial surgery than people on newer drugs.
- Direct Oral Anticoagulants (DOACs) like apixaban, rivaroxaban, and dabigatran don’t need blood tests. They leave your system faster-usually within 9 to 17 hours. For low-risk procedures, you can often just skip your morning dose the day of the procedure. For higher-risk ones, your doctor might ask you to stop 24 to 48 hours before. Studies show the bleeding rate with DOACs is around 1.7%, but stopping them doesn’t lower that risk much-and it raises your chance of clots.
- Antiplatelets like aspirin and clopidogrel are the safest. Multiple studies confirm they don’t increase bleeding risk in skin or minor cosmetic procedures. Even if you’ve been on daily aspirin for years, you can almost always keep taking it. No need to stop.
The key takeaway? Don’t assume all blood thinners are equal. Your doctor needs to know exactly which one you’re on, not just that you’re "on blood thinners."
What Kind of Procedure Are You Getting?
Not all cosmetic procedures carry the same bleeding risk. The procedure type decides how careful you need to be.
- Low-risk procedures include things like mole removals, chemical peels, laser treatments, and small skin excisions under 2 cm. For these, you almost always keep your blood thinners. Stopping them adds no benefit and increases your risk of a clot. The British Society of Dermatologists says it’s safe to continue warfarin (with INR <3.5), DOACs, aspirin, and clopidogrel for these.
- Moderate-risk procedures are things like eyelid lifts (blepharoplasty), minor nose reshaping, or lip fillers. These involve more blood vessels. For DOACs, you might skip the morning dose. For warfarin, keep it going if your INR is controlled. Aspirin? No need to stop.
- High-risk procedures include full facelifts, rhinoplasty, neck lifts, or body contouring like tummy tucks. These are longer, involve deeper tissue, and have more blood vessels. Here, your surgeon might ask you to stop DOACs 24-48 hours before. Warfarin might need to be stopped earlier, with possible bridging (though bridging with heparin is rarely needed and often more risky). Aspirin? Still no need to stop.
Here’s the truth: Most people who think they need to stop their meds for a filler or laser treatment don’t. But if you’re having a full facelift, you need to plan ahead. Talk to your surgeon and your cardiologist or GP at least two weeks before.
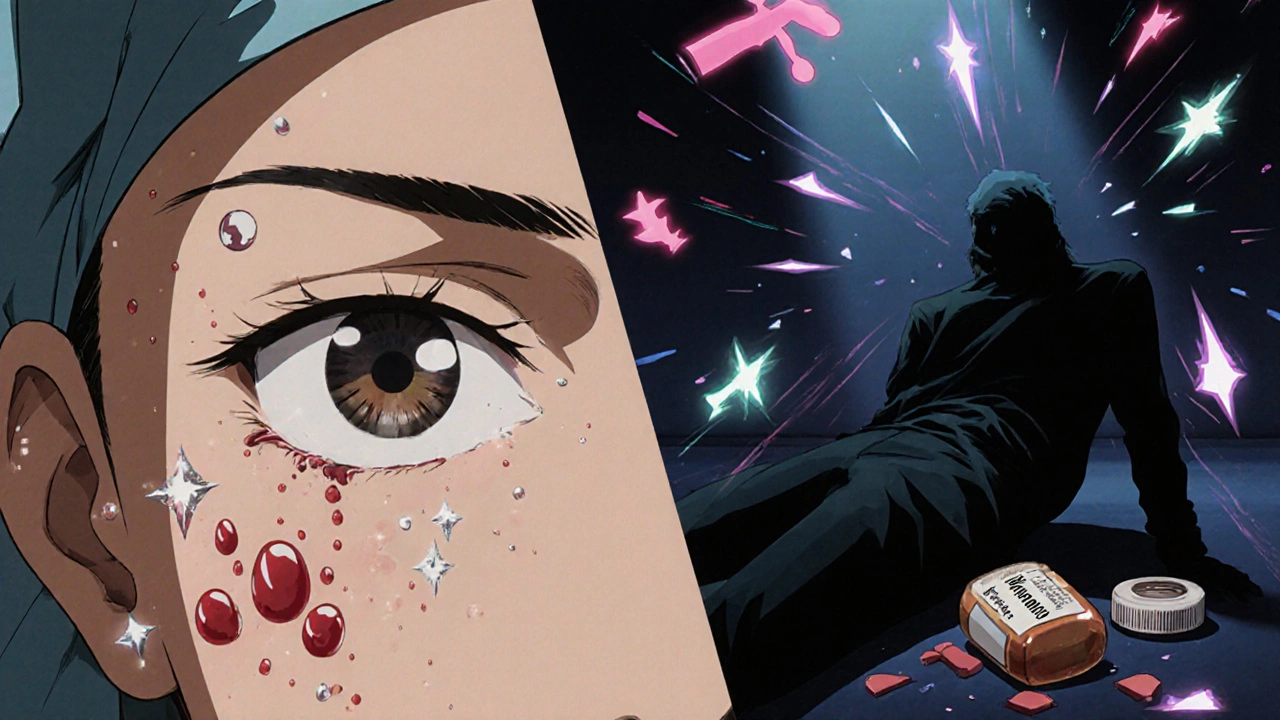
The Real Danger Isn’t Bruising-It’s the Clot
It’s natural to worry about black eyes, swollen cheeks, or big bruises after a procedure. But those are temporary. What you shouldn’t ignore is the silent risk: a blood clot.
When you stop your anticoagulant, even for a few days, your blood starts to thicken again. If you have atrial fibrillation, a mechanical heart valve, or a history of deep vein thrombosis, that’s a recipe for disaster. The average risk of a clot after stopping blood thinners is 0.15%. Sounds small? That’s only if you’re low-risk. For someone with a history of clots, that risk jumps to 1.1%-and that’s even if you’re still on your meds. Stop them? It could be higher.
One study found that 54% of strokes after stopping blood thinners happened after warfarin was paused. Another found 39% after aspirin was stopped. These aren’t rare events. They’re preventable-and too often, they happen because people followed old advice instead of current guidelines.
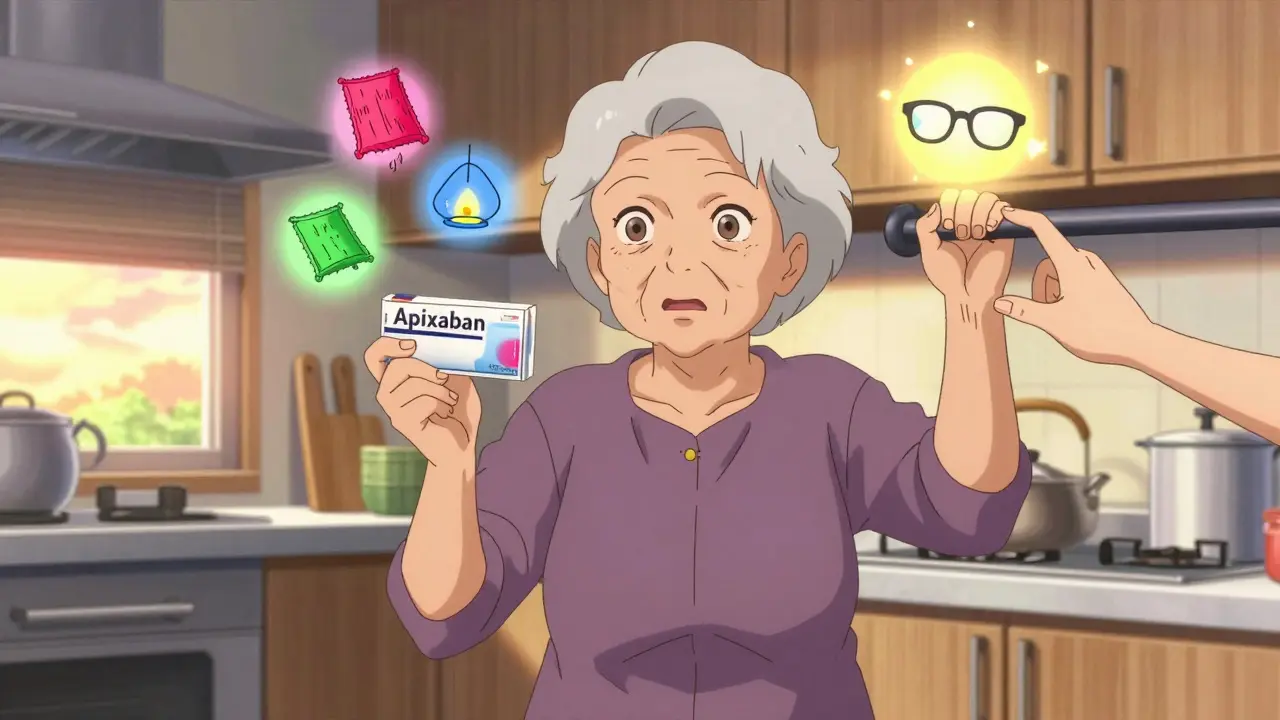
What Your Surgeon Should Be Asking You
A good surgeon won’t just ask, "Are you on blood thinners?" They’ll ask:
- What medication are you taking? (Name and dose)
- Why are you taking it? (Atrial fibrillation? Previous clot? Heart valve?)
- When was your last INR test? (If on warfarin)
- Have you had any bleeding or clotting problems in the past?
- Are you taking more than one blood thinner? (Like aspirin + apixaban?)
If you’re on two blood thinners-say, aspirin and rivaroxaban-that’s called dual therapy. It increases bleeding risk more than either drug alone. In those cases, your surgeon might delay the procedure if possible, or strongly recommend keeping both on for low-risk treatments. Stopping both? That’s a big red flag.
Don’t be afraid to bring your own records. If you have a letter from your cardiologist saying it’s safe to continue your meds, bring it. Many surgeons don’t know the latest guidelines. You might be the one who has to educate them.
What to Do Right Now
Here’s your simple action plan:
- Don’t stop anything on your own. Never stop a blood thinner without talking to both your surgeon and your GP or cardiologist.
- Know your medication. Write down the name, dose, and why you take it. If you’re on warfarin, know your last INR number.
- Ask your surgeon about the procedure’s risk level. Is it minor, moderate, or major? That determines your plan.
- Plan ahead. Schedule a pre-op consultation at least two weeks before your procedure. Give your team time to coordinate.
- Bring your meds list. Include over-the-counter stuff like fish oil, ginkgo, or garlic supplements-they can also thin your blood.
For most people, the answer is simple: keep taking your meds. For others, it’s a careful balance. But one thing is clear: the safest choice isn’t always the one that sounds most obvious.
What Happens If You Bleed Too Much?
Even with the best planning, bleeding can happen. If you notice:
- Swelling that gets worse after 24 hours
- Severe pain or pressure in the treated area
- Dark, bruised skin spreading quickly
- Difficulty breathing or swallowing (after neck or throat procedures)
Call your surgeon immediately. These could be signs of a hematoma-a collection of blood under the skin. In rare cases, it can cut off blood flow to skin grafts or flaps, cause permanent scarring, or even require another surgery to drain it.
But here’s the thing: the chance of this happening if you keep your anticoagulants is still low. In one study of over 1,500 body contouring patients, only 1.27% had drug-related bleeding that needed surgery. For those on apixaban, it was just 0.48%. The risk of a clot from stopping? Much higher.
Bottom Line: Stay on Your Meds Unless Told Otherwise
For the vast majority of people on blood thinners, the best choice is to keep taking them during cosmetic procedures. Bruising and swelling happen anyway-even without meds. But a stroke or pulmonary embolism? That changes your life.
Modern guidelines from the British Society of Dermatologists and the American Society of Plastic Surgeons agree: for minor procedures, don’t stop. For moderate ones, adjust timing. For major ones, plan carefully with your team.
The old rule-stop everything before surgery-is dangerous. The new rule? Work with your doctors. Know your meds. Understand your risk. And don’t let fear of a bruise make you ignore the real danger.




Andrew Baggley
November 20, 2025 AT 15:56Stop overthinking it. The data is clear: keep taking your meds unless you're getting a full facelift.
Reema Al-Zaheri
November 21, 2025 AT 12:58Michael Salmon
November 22, 2025 AT 19:51Doctors who tell you to keep your blood thinners are either lazy or desperate to avoid paperwork. Stop trusting algorithms over experience.
Dion Hetemi
November 23, 2025 AT 10:00One guy was on clopidogrel and thought he was fine because he 'didn't feel different.' Then he turned into a human pomegranate after a laser treatment. We had to ice him for an hour. Don't be that guy.
Chuck Coffer
November 24, 2025 AT 22:51People don't die from clots-they die from surgeons who don't know what they're doing. And now you want me to trust a blog post over a surgeon's gut?
Marjorie Antoniou
November 26, 2025 AT 04:58If you're reading this and you're scared, talk to your cardiologist. Not Reddit. Not your aesthetician. Your real doctor. This isn't a risk worth taking lightly.
Nick Lesieur
November 26, 2025 AT 23:19Angela Gutschwager
November 27, 2025 AT 11:14Ellen Calnan
November 28, 2025 AT 19:27Stopping a blood thinner isn't about bleeding risk. It's about fear. Fear of change. Fear of vulnerability. Fear that if you let yourself be vulnerable-really be vulnerable-you might not survive it.
Maybe the real procedure isn't the peel or the lift. Maybe it's the quiet decision to keep taking the pill. To say: 'I am still here. I am still worth protecting.'
So if you're reading this and you're scared? That's okay. But don't stop the pill because you're afraid. Stop it because your doctor says so. Not because Reddit told you to.