When you pick up a prescription, you expect the generic version to work just like the brand-name drug. That’s the whole point of generics - they save money without sacrificing effectiveness. But what happens when your medication isn’t just a pill? What if it’s a generic combination product - like a drug paired with a device - and the generic versions of each part don’t work together the way the brand does? This isn’t a theoretical problem. It’s happening right now, and it’s leaving patients confused, paying more, and sometimes going without treatment.
What exactly is a generic combination product?
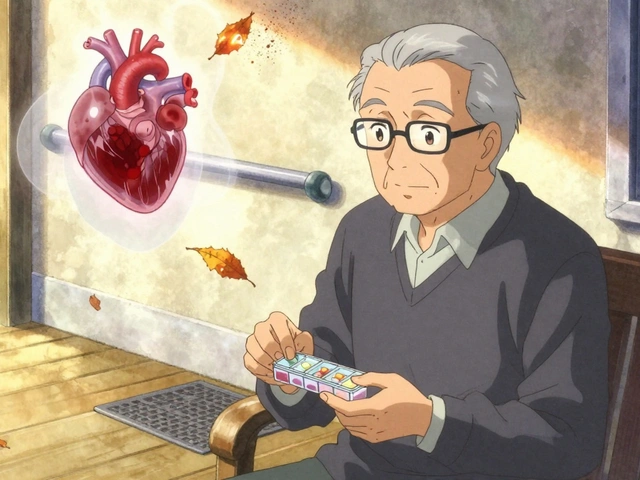
A combination product isn’t just two things in one box. It’s a medical product that blends a drug, a device, or a biological product into a single, interdependent system. Think of an EpiPen: the epinephrine is the drug, but the auto-injector device is just as critical. Without the right mechanism to deliver the dose quickly and accurately, the drug doesn’t work. The FDA calls these drug-device combination products, and they’re classified based on their Primary Mode of Action - the part that does the most important job. If the drug does the heavy lifting, the FDA’s Center for Drug Evaluation and Research (CDER) leads the review. If the device does, it’s the Center for Devices and Radiological Health (CDRH).
Now, here’s the twist: a generic version of a combination product isn’t just a copy of the drug. It’s a copy of the whole system - drug and device - working together. That means if you try to substitute just the generic drug into a branded device, or vice versa, you’re not getting a true generic. You’re getting a mismatch. And that’s dangerous.
Why can’t you just swap parts?
Traditional generic substitution laws were built for pills and capsules. They assume that if the active ingredient matches, the product is interchangeable. But with combination products, the device isn’t just packaging. It’s part of the medicine. Take inhalers, for example. Two different generic inhalers might use the same asthma drug, but if the spray mechanism, valve, or mouthpiece differs even slightly, the dose delivered can vary by 20% or more. That’s not a minor difference - it’s the difference between controlling symptoms and ending up in the ER.
The FDA requires manufacturers of generic combination products to prove their product is substitutable, not just equivalent. That means they must show the device’s user interface - how it feels, how it clicks, how it’s held - behaves exactly like the brand. This isn’t just about function. It’s about human behavior. If a patient can’t press the device the same way, they might not activate it fully. That’s why the FDA demands a six-phase human factors study, including real-world testing with patients. Most companies can’t afford this. Only 38% of complex combination products have more than one generic on the market, compared to 72% of regular generics.

The cost of complexity
Developing a generic combination product takes 18 to 24 months longer than a regular generic. It costs $2.1 million to $3.7 million more. That’s because every part of the device - the button, the spring, the seal - must be matched down to the millimeter. Even small changes in material can affect how the drug is released. One manufacturer told the FDA that their team spent over a year just testing how different plastics reacted to the drug’s chemical composition.
And the result? Patients pay more. A 2024 survey found that people using generic combination products pay 37% more out-of-pocket than those using simple generics. Why? Because there’s so little competition. Only 17 companies have successfully brought generic combination products to market. In contrast, over 120 companies make generic pills. This isn’t a market failure - it’s a regulatory bottleneck.
Real-world consequences
Pharmacists report confusion daily. In a March 2024 survey, 68% said they’ve had patients come in asking why their generic EpiPen doesn’t work with the old device. One pharmacist on Reddit wrote: “I had a mom call me in tears because her son’s new generic injector didn’t click the same way. She thought we gave her the wrong thing.”
Healthcare providers are seeing delays too. A May 2024 AMA survey found that 57% of doctors have had treatment delayed because a patient couldn’t get the right combination. The average delay? Over three business days. That’s three days without medication for someone with asthma, diabetes, or anaphylaxis risk.
And then there’s the data: in 2023, 43% of rejected generic combination product applications were turned down because the device comparison was incomplete. That’s not a technical glitch - it’s a systemic issue. The FDA’s own training materials say the submissions must include “comparative analysis between the device user interfaces.” But many manufacturers don’t know how to do it right. Only 12% of companies say they’re satisfied with the current FDA guidance.

What’s changing - and what’s still broken
The FDA is trying. In April 2024, they released updated guidance to clarify how to prove substitutability. They’ve hired 32 new reviewers specializing in combination products. And in June 2024, Commissioner Dr. Robert Califf launched the “Complex Generic Initiative 2.0,” aiming to cut approval times by 30% by 2026. Fourteen states are also working on new laws to allow substitution of combination products under strict conditions.
But here’s the reality: even if a generic drug and a generic device both get approved, they’re not automatically interchangeable. Each combination - drug + device - must be approved as a single unit. That means if you have a generic epinephrine and a generic auto-injector, they still can’t be paired unless they were tested together as a matched pair. This is why patients often can’t switch, even when generics exist.
What patients and providers need to know
- Don’t assume a generic drug works with any device - even if it’s labeled the same.
- If your prescription says “EpiPen” or “Auvi-Q,” your pharmacist must give you the exact generic version approved for that device. If they can’t, ask why.
- Check the labeling. The FDA requires combination product generics to list the exact device model they’re meant to be used with.
- Report confusion. If you’re given the wrong combination, tell your pharmacist and your doctor. These reports help regulators see where the system is failing.
The goal of generics is to make medicine affordable and accessible. But for combination products, that goal is still out of reach. Until the rules catch up with the science, patients will keep paying more, waiting longer, and risking their health because a device didn’t click the way it was supposed to.
Can I use a generic drug with a brand-name device?
No. Even if the drug is generic, the device is part of the approved product. Mixing components can lead to improper dosing, device failure, or safety risks. The FDA requires that the entire combination - drug and device - be approved together as one unit. Substituting parts is not allowed.
Why are generic combination products so expensive?
Because developing them is extremely complex. Manufacturers must prove the device and drug work together perfectly, which requires years of testing, human factors studies, and regulatory review. The average cost is $2.1-$3.7 million more than a regular generic, and approval takes 18-24 months longer. Few companies can afford this, so competition stays low and prices stay high.
Are there any generic combination products available?
Yes, but they’re rare. Only 12% of the combination product market is generic, compared to over 90% for regular drugs. Some examples include generic versions of inhalers like Advair and Combivent, but even those are limited to specific device-drug pairings. Auto-injectors like EpiPen generics are still in development, and only one has been approved so far - and only as a matched system, not as interchangeable parts.
How do I know if my medication is a combination product?
Check the prescription label. If it includes a device - like an injector, inhaler, pump, or patch - it’s likely a combination product. You can also ask your pharmacist or check the FDA’s database of approved combination products. The product name will often include terms like “auto-injector,” “inhaler,” or “delivery system.”
Is there any progress being made to fix this?
Yes. The FDA has increased staff, updated guidance, and launched initiatives to speed up approvals. Fourteen states are updating laws to allow substitution under strict conditions. But the real fix requires manufacturers to invest in the complex testing needed - and until that happens, patients will continue to face delays and higher costs.