Every year, one in three adults over 65 falls. Many of these falls aren’t bad luck-they’re caused by medications they’re taking every day. It’s not just about being unsteady on your feet. It’s about what’s in your medicine cabinet. Some common prescriptions, even ones prescribed for years, can quietly rob you of your balance, your confidence, and your independence.
Why Medications Are a Silent Threat
Falls aren’t just bruises or bumps. For older adults, a fall can mean a broken hip, a long hospital stay, or even death. In the U.S., over 36,000 older adults died from falls in 2023. And research shows that in 65% to 93% of those cases, the person was taking at least one medication known to increase fall risk. These aren’t rare or experimental drugs. They’re the ones doctors prescribe regularly-for sleep, anxiety, blood pressure, pain, and depression. The problem isn’t always the drug itself. It’s how the body changes with age. Older adults process medications differently. Their kidneys and liver don’t clear drugs as fast. Their nervous system becomes more sensitive. A dose that was fine at 50 can become dangerous at 75.The Top 9 Medication Classes That Raise Fall Risk
Not all medications are created equal when it comes to falls. Some are far more dangerous than others. Here are the nine main classes linked to higher fall risk, ranked by how strongly they’re tied to injuries:- Antidepressants - These have the strongest link to falls. Both tricyclics (like amitriptyline) and SSRIs (like sertraline or fluoxetine) can cause dizziness, low blood pressure, and slowed reactions. A 2023 Mayo Clinic review found that older adults on antidepressants were up to 50% more likely to fall than those not taking them.
- Benzodiazepines - Drugs like diazepam (Valium), lorazepam (Ativan), and alprazolam (Xanax) are prescribed for anxiety and sleep. But they cause drowsiness, confusion, and poor coordination. Long-term use (more than two weeks) is especially risky. The American Geriatrics Society says these drugs should be avoided in older adults whenever possible.
- Sedative-Hypnotics - Sleep aids like zolpidem (Ambien), eszopiclone (Lunesta), and zaleplon (Sonata) don’t just help you sleep-they can make you sleepwalk, act confused, or fall the next morning. The CDC calls them “high-risk” because their effects linger into daylight hours.
- Antipsychotics - Used for dementia-related agitation, drugs like haloperidol and risperidone increase fall risk by 40%. First-generation antipsychotics are worse than newer ones, but none are safe for long-term use in older adults.
- Muscle Relaxants - Baclofen, cyclobenzaprine, and methocarbamol can make you feel drugged. Baclofen, in particular, has been linked to a 70% higher fall risk. These are often prescribed for back pain, but the trade-off isn’t worth it.
- Opioids - Painkillers like oxycodone, hydrocodone, and tramadol cause dizziness, slow reflexes, and impaired thinking. The higher the dose, the higher the risk. High-potency opioids can increase fall risk by 80% compared to low-dose options.
- NSAIDs - Common pain relievers like ibuprofen and naproxen can lower blood pressure, especially when standing up. This sudden drop-called orthostatic hypotension-is a major cause of falls. NSAIDs also interact badly with blood pressure meds.
- Diuretics - Water pills like furosemide (Lasix) help with fluid retention but can cause dehydration and low blood pressure. A sudden trip to the bathroom at night can become a fall risk if you’re dizzy or weak.
- Anticholinergics - Found in many over-the-counter sleep aids, allergy meds, and bladder pills (like diphenhydramine or oxybutynin), these drugs block a key brain chemical. The result? Blurry vision, confusion, dry mouth, and poor balance. Many older adults don’t realize their nighttime allergy pill is putting them at risk.
It’s Not Just Prescription Drugs
Many people think only prescriptions matter. But over-the-counter meds can be just as dangerous. Antihistamines like Benadryl, sleep aids like Unisom, and even some herbal supplements like valerian root can cause drowsiness and disorientation. A 2023 study found that 65% of older adults didn’t know their allergy or sleep meds could make them fall. One woman in Bristol, 76, fell twice in one month after starting a new OTC sleep aid. She didn’t tell her doctor because she thought it was “just a pill.” Her pharmacist later flagged it as a high-risk anticholinergic. She switched to a non-sedating option and hasn’t fallen since.How Doctors Miss the Signs
Doctors aren’t ignoring the risk. But they’re often overwhelmed. A typical visit lasts 15 minutes. Medication lists are long. Patients don’t always mention what they’re taking-especially if they think it’s harmless. Only 15% of older adults who’ve fallen talk to their doctor about it. Many patients take meds for years without review. A 2023 study showed 63% of older adults on multiple fall-risk drugs didn’t know they were at risk. That’s not their fault. It’s a system failure.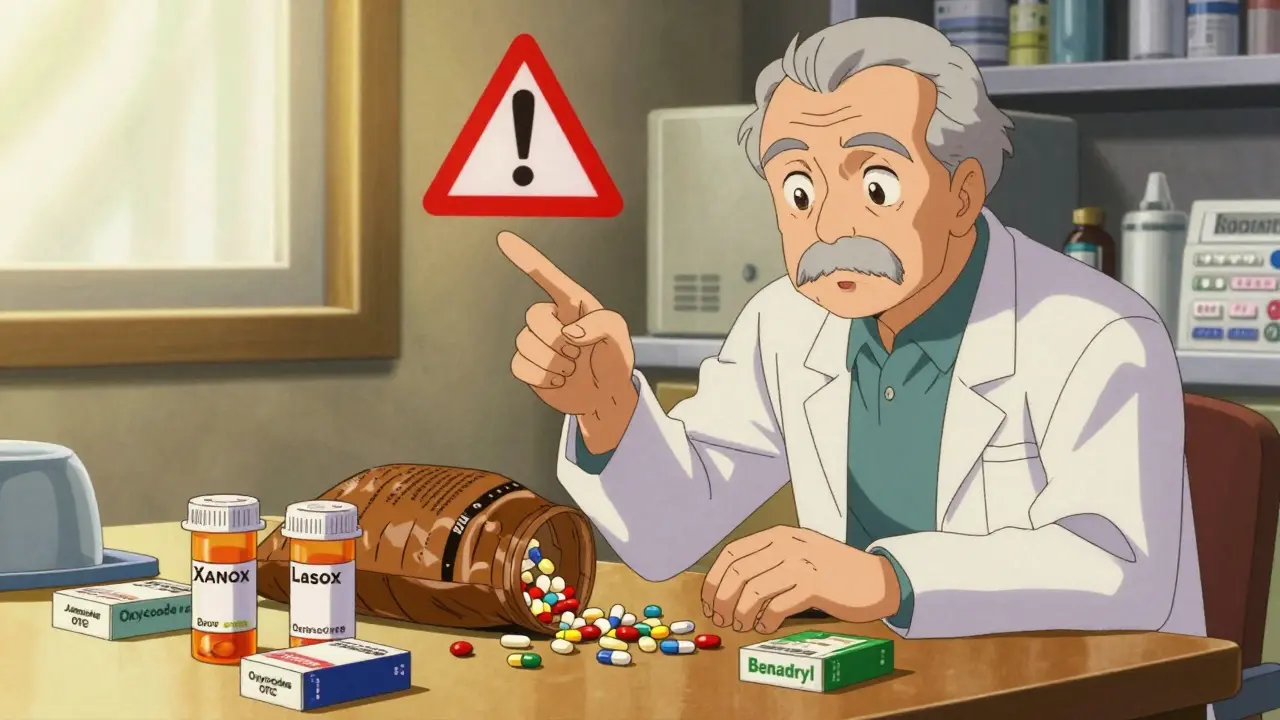
What You Can Do: The STOP, SWITCH, REDUCE Plan
The CDC’s STEADI program gives a clear, simple plan:- STOP - Ask your doctor if any meds can be stopped entirely. Many sleep aids, anxiety meds, and painkillers are taken long after they’re needed.
- SWITCH - Can a safer alternative work? For insomnia, cognitive behavioral therapy (CBT-I) works better than Ambien and has no fall risk. For anxiety, non-benzodiazepine options like buspirone are safer. For pain, physical therapy and acetaminophen may be enough.
- REDUCE - Lower the dose. Even cutting a benzodiazepine in half can reduce fall risk significantly. Always do this slowly under medical supervision.
How to Have This Conversation
Don’t wait for your doctor to bring it up. Be ready. Bring your entire medication list to every appointment-including vitamins, supplements, and OTC drugs. Use the “brown bag method”: dump everything out on the table. It’s easier to see what you’re really taking. Ask these questions:- “Is this medication still necessary?”
- “Could it be making me dizzy or unsteady?”
- “Is there a safer option?”
- “Can we try stopping or lowering this one?”
What’s Changing in 2025
The landscape is shifting. The American Geriatrics Society’s 2024 Beers Criteria update will include new warnings for recently approved drugs. Medicare now penalizes doctors who overprescribe fall-risk meds. AI tools are being tested to flag dangerous combinations before they’re even written. The National Institute on Aging just funded $15 million in research to develop better deprescribing protocols-ways to safely stop harmful meds without causing withdrawal or rebound symptoms. And while safer alternatives exist, they’re not always affordable. New non-benzodiazepine anxiety drugs can cost $450 a month-15 times more than generic Xanax. But for many, the cost of a fall-hospital bills, rehab, lost independence-is far higher.






Sidra Khan
December 25, 2025 AT 00:57I get that meds can cause falls, but let’s be real-half these people are just lazy. If you’re on 12 pills and still can’t walk to the bathroom without holding the wall, maybe the problem isn’t the drugs, it’s that you haven’t moved in years. My grandma took everything and still hiked the Grand Canyon at 82. She didn’t need a pharmacist to babysit her medicine cabinet.
Stop blaming the pills and start blaming the couch.
Ademola Madehin
December 25, 2025 AT 16:08OMG I JUST HAD THIS SAME THING WITH MY DAD 😭
He was on Xanax for 7 years, then one morning he fell in the shower and cracked his skull. We didn’t even know it was the med until the ER doc said, ‘Sir, you’re basically drunk right now.’
Now he’s on CBD oil and walks like a teenager again. I’m telling everyone. This post saved his life. 🙏
Andy Grace
December 27, 2025 AT 00:01There’s real value here. I’ve seen elderly patients on 8+ meds with zero review. The system is broken-not because doctors are negligent, but because time and reimbursement structures don’t allow for proper deprescribing. It’s not about blame, it’s about design.
Pharmacists doing medication reviews should be standard, not optional. And insurance needs to cover non-pharmaceutical alternatives like CBT-I or PT. We’re spending millions on ER visits after falls-why not prevent them?
Delilah Rose
December 28, 2025 AT 22:12I’ve been researching this for my mom since she started falling last year-she’s 81, takes 6 prescriptions, 3 OTC sleep aids, and a ‘natural’ blend of herbs that says ‘calming’ on the bottle but has diphenhydramine in the ingredients list. I didn’t know that was an anticholinergic until I read this. I cried. Not because she’s old, but because I thought I was helping her by giving her something to sleep. Turns out, I was putting her at risk every night.
So I made a spreadsheet. Every med, every supplement, every dose, every reason it was prescribed. Took it to her PCP and her pharmacist together. We cut two meds cold turkey (she was fine), tapered two others over six weeks, and switched her sleep aid to a non-sedating melatonin formula. She hasn’t fallen in four months. It’s not magic. It’s just… attention. And it’s terrifying how few people do it.
If you’re over 65 and on more than three meds, please, please, please do this. Even if you think you’re fine. You’re not. We’re not. The body changes. The meds don’t. And that’s the problem.
Spencer Garcia
December 30, 2025 AT 12:50Bring your brown bag to your next appointment. That’s it. That’s the whole checklist.
Don’t overthink it. Just do it.
Abby Polhill
December 30, 2025 AT 14:26Interesting how the Beers Criteria keeps evolving but primary care still operates on 15-minute visit economics. The pharmacoeconomic burden of fall-related injuries in elderly populations is estimated at $50B annually in the US alone, yet deprescribing interventions remain underfunded and underutilized. We’re treating symptoms, not systems.
Also, the OTC anticholinergic burden is grossly underestimated. A 2023 JAMA study showed 42% of community-dwelling seniors consume ≥1 anticholinergic daily-many unaware it’s in their allergy med. This isn’t a clinical issue. It’s a public health blind spot.
Jillian Angus
January 1, 2026 AT 02:57My uncle took Ambien for years. Never fell. Then one night he got up, walked to the kitchen, and broke his wrist trying to make toast. He didn’t remember any of it.
He stopped the med. No more falls. No more confusion.
Just saying.
Gray Dedoiko
January 2, 2026 AT 22:41I work in geriatrics. I see this every week. The saddest part? Most patients don’t even connect the dots. They say, ‘I’m just getting older,’ or ‘I’m clumsy now.’ But it’s not aging. It’s the meds.
One woman told me she took her blood pressure med at night because she didn’t want to pee during the day. I had to explain that’s why she was falling at 3 a.m. She cried. Then she switched to morning dosing. No more falls.
Small changes. Big impact.
Steven Mayer
January 3, 2026 AT 07:59Let’s not pretend this is about safety. This is about pharmaceutical profit margins. The FDA approves these drugs because they’re profitable. The CDC warns about them because they’re politically convenient. But no one’s holding the manufacturers accountable for designing drugs that degrade mobility in the elderly.
Who profits when a 78-year-old breaks a hip? Hospitals. Rehab centers. Insurance companies. Not the patient.
And now they’re pushing AI to ‘flag’ dangerous combos instead of banning the damn drugs. That’s not innovation. That’s damage control with a tech veneer.
Charles Barry
January 4, 2026 AT 20:46THIS IS A GOVERNMENT PLOY TO CONTROL THE ELDERLY.
They don’t want you mobile. They don’t want you independent. That’s why they push these ‘fall risk’ narratives-so you’ll take fewer meds, get weaker, and rely on them for everything. Look at the stats-they’re cooked. The CDC is funded by Big Pharma. The ‘Beers Criteria’? Written by doctors who get paid by drug reps.
My grandfather took 12 pills a day. Lived to 94. Walked 5 miles a day. Never fell. Why? Because he didn’t listen to the fear-mongering. He trusted his body.
Don’t let them take your autonomy. Keep your pills. Stay strong.
Joe Jeter
January 5, 2026 AT 08:14So what? You’re telling me we should stop giving people meds because they might fall? What about their anxiety? Their insomnia? Their pain? You want them to suffer so they don’t trip over a rug?
And who’s gonna pay for ‘CBT-I’? It’s $200 a session. My aunt’s on Social Security. She can’t afford therapy. She can afford $5 for Ambien.
Stop pretending this is about safety. It’s about privilege. If you’re rich, you get non-drug options. If you’re poor, you get the pill and hope you don’t fall.
Real solution? Fix the housing. Fix the lighting. Fix the stairs. Not the meds.