Institutional Programs in Healthcare: What They Are and How They Shape Treatment
When you walk into a hospital or clinic, you’re not just getting care—you’re stepping into a system built on institutional programs, formalized systems that standardize how medications are prescribed, monitored, and managed across healthcare settings. These programs are the hidden backbone of safe, consistent care. They’re not just paperwork. They’re the reason your doctor checks for drug interactions before writing a prescription, why pharmacists double-check your meds before handing them over, and why hospitals have strict rules about who gets which drugs and when.
These programs rely on clinical guidelines, evidence-based rules developed by medical experts to ensure treatments work and stay safe—like the ones that tell doctors when to use naltrexone for alcohol use disorder or when to avoid combining SSRIs with certain opioids. They also tie into pharmaceutical policy, the rules that control drug availability, pricing, and access within hospitals and insurance networks. For example, a hospital might only stock febuxostat over allopurinol because it’s more effective for certain patients, or require prior authorization for newer antidepressants like zuranolone to control costs and ensure proper use.
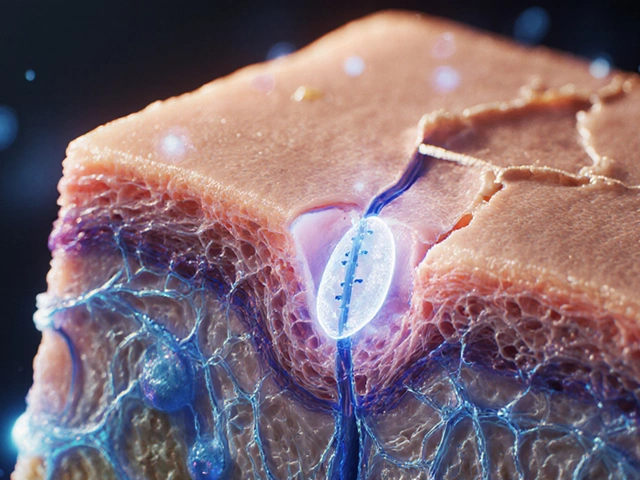
And then there’s medication safety, the core goal of every institutional program: preventing harm from drugs. That’s why you see alerts about grapefruit juice interacting with statins, why seniors get lower doses of certain pills, and why hospitals track liver enzyme changes in patients on statins. These aren’t random checks—they’re built into institutional programs to catch problems before they happen. Even something as simple as how a drug is delivered—oral, injection, or topical—gets regulated because each route carries different risks.
These programs don’t just affect what you get—they shape how you get it. If you’ve ever wondered why your doctor won’t prescribe a certain painkiller, or why you had to wait for a shunt evaluation for NPH, or why you’re being monitored for serotonin syndrome when taking both an SSRI and tramadol—it’s because of institutional programs. They’re the reason you get standardized care, not guesswork.
Below, you’ll find real-world examples of how these systems play out in practice: from how crossover trials help approve new drugs, to how FDA alerts get built into hospital protocols, to why dosing changes for aging bodies aren’t optional—they’re required. These aren’t abstract rules. They’re the reason you’re safer today than you were ten years ago. And they’re still evolving.
Healthcare Communication Training: How Institutional Education Programs Improve Patient Outcomes
By Lindsey Smith On 25 Nov, 2025 Comments (18)
Institutional healthcare communication programs are transforming patient care by teaching clinicians how to listen, explain, and collaborate effectively. Evidence shows these training initiatives reduce errors, improve satisfaction, and save lives.
View More