When you’re on Medicare and taking daily medications, knowing how your plan covers generics can save you hundreds - even thousands - of dollars a year. Medicare Part D formularies are the lists of drugs your plan agrees to pay for, and generic drugs make up 92% of all prescriptions filled under Part D. That’s not an accident. The system is designed to steer you toward cheaper, equally effective options. But understanding how that works - and how to use it to your advantage - isn’t always obvious.
How Generic Drugs Fit Into Part D Tiers
Medicare Part D plans organize drugs into five tiers, and generics live mostly on the bottom two. Tier 1 is for preferred generics, which usually cost $0 to $15 for a 30-day supply. Tier 2 is for non-preferred generics, which might cost a bit more - anywhere from $15 to $40, or sometimes a percentage of the drug’s price (25% to 35%). The higher the tier, the more you pay. Brand-name drugs? They’re typically on Tier 3 or higher. That’s why your plan pushes generics: they’re cheaper for everyone - you, the plan, and the system as a whole. Here’s the real kicker: even though generics make up 92% of prescriptions, they only account for about 18% of total drug spending under Part D. That’s because they’re so much cheaper. A blood pressure generic might cost $5, while the brand version could be $120. The math adds up fast when you’re taking multiple meds daily.What Changed in 2025 - The $2,000 Cap
Before 2025, Medicare Part D had a notorious gap called the “donut hole.” Once you and your plan spent a certain amount, you paid full price until you hit a higher threshold. That was brutal for people on multiple generics. The Inflation Reduction Act of 2022 changed that. Starting January 1, 2025, there’s a hard cap: you pay no more than $2,000 out of pocket for all your drugs in a calendar year. That includes both brand-name and generic drugs. After you hit that $2,000 mark, you enter catastrophic coverage - and for the rest of the year, you pay $0 for your generics. This is huge. For someone taking three or four generic medications, that cap can mean saving $400 to $800 a year. And it’s not just a one-time thing. That cap resets every January. So even if you hit it early, you’re covered for the rest of the year.How Your Costs Work - Before and After the Cap
Let’s say you’re on a standard Part D plan in 2025. Here’s how your money flows:- Deductible: You pay the first $615 of your drug costs. Not all plans have this - 52% of stand-alone plans have a $0 deductible in 2025.
- Initial coverage phase: After the deductible, you pay 25% coinsurance for generics. Your plan pays the other 75%. This continues until your total out-of-pocket spending hits $2,000.
- Catastrophic coverage: Once you hit $2,000, you pay $0 for every generic prescription for the rest of the year.

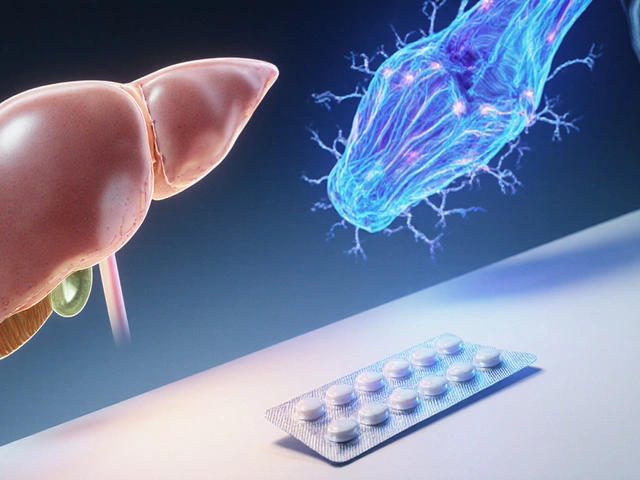
Why Your Plan Might Not Cover the Generic You Want
Just because a generic exists doesn’t mean your plan covers it. Plans pick which generics to include - and they often pick only one or two from each drug class. For example, if you take lisinopril for high blood pressure, your plan might cover the version made by Teva but not the one made by Mylan - even though they’re chemically identical. This is called “therapeutic interchange.” It’s legal, but it’s confusing. You might go to the pharmacy and get a different generic than you’re used to - and if your plan doesn’t cover that one, you’ll be stuck paying full price. That’s why 23% of all Part D complaints in 2024 were about generic substitution issues. The rules say plans must cover at least two different generics in every therapeutic class. But that doesn’t mean they cover all of them. And for six protected drug classes - like antidepressants, antiretrovirals, and anticonvulsants - plans must cover every available generic. If you’re on one of those, you’re better protected.How to Check Your Generic Coverage Before You Enroll
You can’t just pick a plan based on price. You have to check your meds. Use the Medicare Plan Finder. Type in every drug you take - including the generic name and dosage. The tool will show you exactly how much you’ll pay under each plan. Don’t guess. Don’t assume. Enter your exact prescriptions. Also, look at the Annual Notice of Change (ANOC). Every fall, your plan sends you this letter. It tells you if your drugs are moving tiers, getting removed, or if your copay is changing. Thirty-seven percent of plans change at least one generic’s tier placement each year. If your $5 generic jumps to $40, you need to know before January. If your drug isn’t on the formulary, you can request a coverage determination. You’re asking the plan to make an exception. In 2023, 83% of these requests were approved - especially if your doctor says the specific generic is medically necessary.What Experts Say - And What You Should Watch For
Dr. Richard Frank from Harvard says the tiered system saves the program $15 billion a year by pushing people toward generics. That’s good for the system. But Juliette Cubanski from KFF warns that 25% coinsurance can still be unpredictable for people on fixed incomes. If you take five generics, even at $10 each, that’s $50 a month - $600 a year. That’s not nothing. And here’s something most people don’t know: the government is starting to negotiate prices on some generics. Starting in 2029, Part D plans will be required to cover negotiated prices for certain drugs. Insulin glargine (the generic version of Lantus) is already on the list. That could bring prices down even further. In 2026, plans will have to include a “generic price comparison tool” in their member portals. That means you’ll be able to see which version of your drug costs the least - right in your online account.What You Can Do Right Now
1. Write down every medication you take - including dosages. Don’t forget over-the-counter drugs your doctor recommended. 2. Use the Medicare Plan Finder to compare plans based on your exact list. 3. Look for plans with $0 deductible if you take multiple generics. You’ll skip the first $615. 4. Check your plan’s formulary every fall when you get the ANOC. 5. Ask your pharmacist if a cheaper generic is available - even if it’s not on your plan’s list. Sometimes, switching to a different brand of the same drug saves money. 6. Request a coverage determination if your drug gets dropped or moved to a higher tier. You have the right to appeal.Real Stories - What People Are Saying
One beneficiary in Ohio wrote on Reddit: “My three generics - metformin, lisinopril, and atorvastatin - cost me $0 this year. I saved over $300 a month compared to before Medicare.” Another in Florida said: “I got a different generic for my thyroid med. My plan didn’t cover it. I had to pay $85 out of pocket. I filed an appeal - they approved it in two weeks.” The data backs this up: beneficiaries who use mostly generics report 87% satisfaction with their drug coverage. Those on brand-name drugs? Only 76%.What’s Coming Next
By 2027, nearly all Part D plans will offer $0 copays for at least half of the most common generics. More insurers are competing on price - and they’re using low-cost generics as a draw. The Senate is also looking at a rule that would force plans to cover all generics in a class if they cover any. That would end the “one generic only” problem. The bottom line? Generic coverage under Medicare Part D isn’t perfect. But it’s working better than ever. The $2,000 cap is a game-changer. The tools to find the best plan are right there. And with more price transparency coming, you’re in a better position than ever to control your drug costs.Are all generic drugs covered by Medicare Part D?
No. Medicare Part D plans choose which generics to include on their formularies. While they must cover at least two generics in each therapeutic class, they don’t have to cover every available generic. Always check your plan’s formulary before enrolling.
Why is my generic drug not covered even though it’s the same as the brand?
Plans often cover only one or two generic versions of a drug, even if others are chemically identical. This is called therapeutic interchange. If your pharmacy tries to substitute a generic your plan doesn’t cover, you’ll pay full price. You can ask your doctor to write a prescription for the specific generic your plan covers, or file a coverage determination request.
Does the $2,000 out-of-pocket cap apply to all my drugs?
Yes. The $2,000 cap (increasing to $2,100 in 2026) applies to all covered drugs - brand-name and generic - that you pay for out of pocket. Once you hit that amount, you pay nothing for the rest of the year. Only your actual payments count toward the cap for generics.
How do I find the lowest-cost generic for my medication?
Use the Medicare Plan Finder tool and enter your exact drug names and dosages. Compare multiple plans side by side. Also, ask your pharmacist if there’s a cheaper generic version available - sometimes the same drug is sold under different brand names at different prices.
What should I do if my plan drops a generic I rely on?
First, contact your plan and request a coverage determination - ask them to make an exception. If denied, you can appeal. Meanwhile, check if another plan in your area covers your drug. You can switch plans during the Annual Enrollment Period (October 15 to December 7) or during a Special Enrollment Period if you qualify.
Can I switch plans mid-year if a generic I need gets removed?
Generally, no - you can only switch during the Annual Enrollment Period. But if your plan removes a drug you’re taking, you qualify for a Special Enrollment Period. You’ll have two months to enroll in a new plan that covers your medication. Contact Medicare or your State Health Insurance Assistance Program (SHIP) for help.





josue robert figueroa salazar
December 28, 2025 AT 02:10Lori Anne Franklin
December 28, 2025 AT 04:57wendy parrales fong
December 28, 2025 AT 14:20Alex Ragen
December 28, 2025 AT 16:41carissa projo
December 29, 2025 AT 14:32Ellie Stretshberry
December 31, 2025 AT 14:10Jody Kennedy
January 1, 2026 AT 03:40christian ebongue
January 2, 2026 AT 11:26Ryan Cheng
January 2, 2026 AT 15:30Bryan Woods
January 3, 2026 AT 18:09Jeanette Jeffrey
January 4, 2026 AT 08:24Sarah Holmes
January 5, 2026 AT 18:41Matthew Ingersoll
January 6, 2026 AT 08:54david jackson
January 8, 2026 AT 08:09