Naranjo Scale Calculator
How It Works
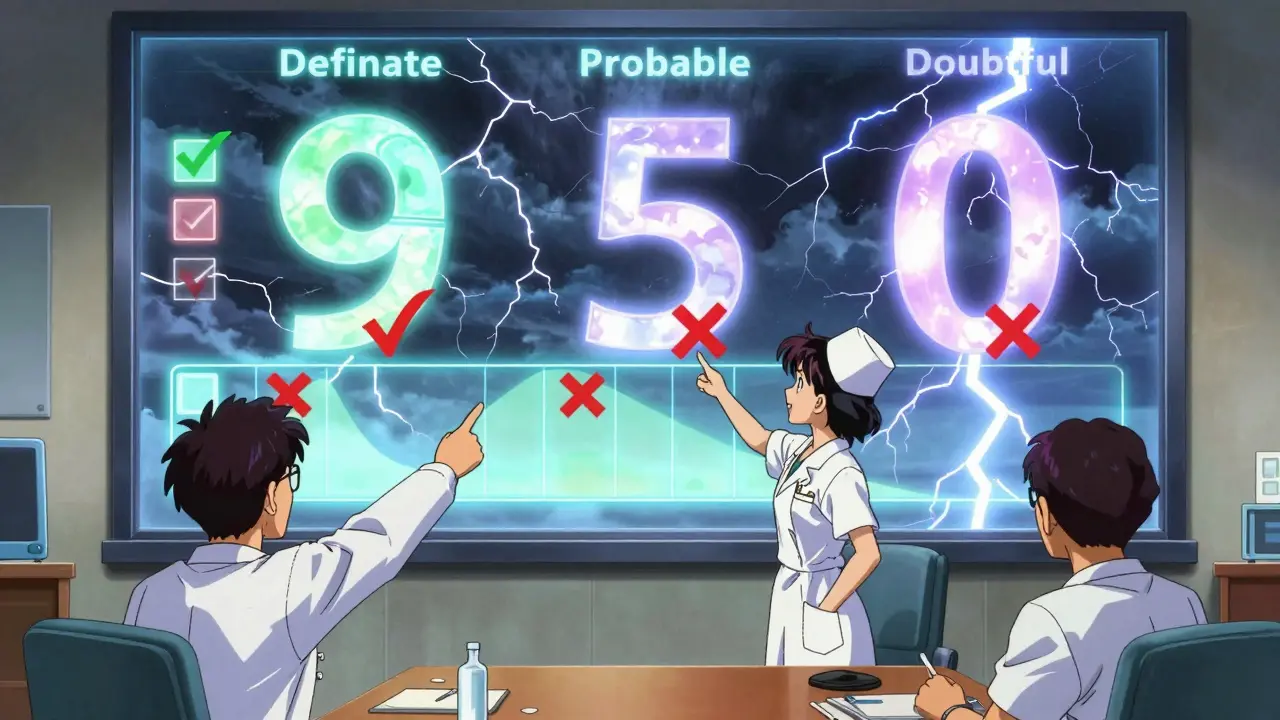
The Naranjo Scale is a standardized 10-question tool used by healthcare professionals to determine if a drug caused an adverse reaction. Each question gives points based on your answers, and your total score determines the likelihood:
- 9+ Definite reaction
- 5-8 Probable reaction
- 1-4 Possible reaction
- 0 or lower Doubtful reaction
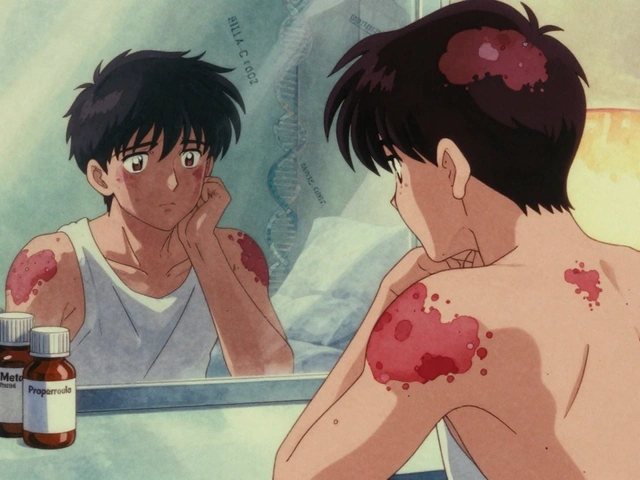
When a patient gets sick after taking a new medication, how do you know if the drug actually caused it? It’s not always obvious. Maybe the patient had a virus. Maybe their condition worsened on its own. Or maybe the drug triggered a rare reaction. Without a clear way to tell, doctors and pharmacists risk missing serious side effects-or blaming drugs for problems they didn’t cause. That’s where the Naranjo Scale comes in.
What Is the Naranjo Scale?
The Naranjo Scale is a simple, 10-question tool used by healthcare professionals to decide if a drug caused an adverse reaction. It was created in 1981 by Dr. Carlos A. Naranjo and a team of researchers in response to the thalidomide disaster, when thousands of babies were born with severe birth defects after their mothers took the drug during pregnancy. Back then, there was no standard way to link drugs to side effects. The Naranjo Scale fixed that.It’s not fancy. No machines. No blood tests. Just a checklist you fill out based on what you know about the patient, the drug, and what happened after they took it. Each question gives you points-positive, negative, or zero. Add them up, and you get a score that tells you how likely the drug caused the reaction.
How the Scoring Works
The scale has 10 questions. Here’s what they look like, simplified:- Have other reports linked this drug to this reaction before? (+1 if yes)
- Did the reaction happen after the drug was given? (+2 if timing fits, -1 if it happened before)
- Did symptoms get better after stopping the drug? (+1 if yes)
- Did the reaction come back when the drug was given again? (+2 if yes, -1 if it got worse)
- Could something else have caused it? (-1 if yes, +2 if no)
- Did giving a placebo cause the same reaction? (-1 if yes, +1 if no)
- Was the drug at toxic levels in the blood? (+1 if yes)
- Did the reaction get worse when the dose went up? (+1 if yes)
- Has the patient had this reaction to the same drug before? (+1 if yes)
- Is there objective proof, like lab results or imaging, confirming the reaction? (+1 if yes)
You don’t answer ‘maybe.’ You pick Yes, No, or Don’t Know. Each choice adds or subtracts points. The total score tells you the likelihood:
- 9 or higher = Definite reaction
- 5 to 8 = Probable reaction
- 1 to 4 = Possible reaction
- 0 or lower = Doubtful reaction
That’s it. No guesswork. No gut feeling. Just numbers.
Why It’s Still Used Today
You might think a 40-year-old tool would be outdated. But it’s not. In 2023, a study in Cureus found that the Naranjo Scale was still used in 78% of published drug safety case reports-more than any other tool. Why?Because it works. Hospitals, pharmacies, and regulatory agencies use it to decide whether to report a side effect to the FDA or EMA. It’s built into electronic health records like Epic. Pharmacists in Massachusetts General Hospital use it daily to document reactions. It forces you to ask the right questions instead of jumping to conclusions.
One pharmacist told a Reddit thread: “We use it every day. It stops us from blaming drugs for everything. And it stops us from ignoring real reactions.”

Where It Falls Short
The Naranjo Scale isn’t perfect. It was designed for single drugs and simple reactions. Today, patients often take five, six, even ten medications at once. That’s a problem.Imagine an 80-year-old with heart disease, diabetes, and arthritis. They start a new blood pressure pill and get dizzy. Was it the new drug? Or the statin they’ve been on for 10 years? Or the interaction between all of them? The Naranjo Scale can’t handle that. It only looks at one drug at a time.
Another issue: Question 6 asks about placebo rechallenge. That means giving the patient a sugar pill to see if they still react. But in modern medicine, that’s unethical. You don’t give someone a placebo if they had a dangerous reaction before. So most clinicians answer “Don’t Know,” which lowers their score-even if the reaction is real.
And what about new drugs? Immunotherapies, gene therapies, biologics-these can cause side effects months after stopping. The Naranjo Scale doesn’t account for delayed reactions like that. A 2024 analysis in Nature Reviews Drug Discovery pointed out that the scale’s framework just doesn’t fit these modern treatments.
What’s Replacing It?
There are newer tools. The Liverpool ADR Probability Scale can handle multiple drugs. The PADRAT is designed for kids. The WHO-UMC system is simpler but less precise. The ALDEN scale is better for antibiotics.But here’s the thing: none of them have the same global reach. The Naranjo Scale is in 78 of the 152 countries in the WHO’s drug safety program. It’s the default in North America and Europe. Regulatory agencies like the FDA and EMA still reference it in their guidelines.
Instead of replacing it, people are upgrading it. A 2023 study built a Python app that auto-fills the scale using electronic health data. It cuts assessment time from 11 minutes to 4.2 minutes and cuts errors from 28% to 9%. Hospitals are starting to use it.
How to Use It Right
If you’re a nurse, pharmacist, or doctor trying to use the Naranjo Scale, here’s what you need to know:- Don’t skip the “Don’t Know” answers. They’re not a cop-out. They’re honest.
- Question 5 (“Could something else cause this?”) is the trickiest. Talk to a clinical pharmacist if you’re unsure.
- Don’t force a “definite” score just because you think the drug is guilty. Stick to the facts.
- Use digital tools if you can. They reduce mistakes and save time.
- Training takes 2-4 hours. Practice with 5-10 real cases before using it alone.
There’s a free worksheet from Nebraska ASAP and a 27-page training manual from the International Society of Pharmacovigilance. Use them.
What Happens After You Score It?
If you score a reaction as “probable” or “definite,” you report it. In the U.S., that means filing a report to the FDA’s FAERS system. In Europe, it goes to EudraVigilance. These reports help regulators spot dangerous drugs before they hurt more people.But reporting isn’t just about compliance. It’s about safety. One case report using the Naranjo Scale helped identify a new interaction between a common antibiotic and a blood thinner. That led to updated prescribing guidelines-and saved lives.
Final Thoughts
The Naranjo Scale isn’t magic. It doesn’t replace clinical judgment. But it gives you structure. It turns guesswork into evidence. In a world full of complex drugs and confusing symptoms, that’s powerful.It’s not going away anytime soon. Even as AI and new tools emerge, the Naranjo Scale will stick around-not because it’s perfect, but because it’s simple, transparent, and proven. For now, it’s still the best starting point for figuring out if a drug really caused a reaction.
Is the Naranjo Scale still used today?
Yes. As of 2023, it’s used in 78% of published adverse drug reaction case reports and is referenced by the FDA and European Medicines Agency. Many hospitals and pharmacovigilance teams rely on it daily, especially in structured reporting systems.
Can the Naranjo Scale be used for multiple drugs at once?
No. The Naranjo Scale is designed for single-drug reactions. In patients taking multiple medications-common in older adults-it can’t determine which drug caused the reaction. Tools like the Liverpool ADR Probability Scale are better suited for these complex cases.
Why is the placebo challenge question problematic?
Re-administering a drug to test if a reaction returns (placebo challenge) is considered unethical in modern medicine. If a patient had a severe reaction, giving them a placebo to see if symptoms return could be dangerous or misleading. Most clinicians now mark this as “Don’t Know,” which affects the final score.
How accurate is the Naranjo Scale?
Studies show moderate inter-rater reliability (kappa 0.4-0.6), meaning different clinicians usually agree on the score. But accuracy depends on clinical knowledge. Misinterpreting “alternative causes” or missing key timelines can lead to errors. Digital tools have reduced error rates from 28% to 9%.
Can I use the Naranjo Scale for pediatric patients?
The original scale wasn’t designed for children. A modified version called PADRAT (Paediatric Adverse Drug Reaction Assessment Tool), developed in 2015, is better suited for kids because it considers age-specific reactions, growth effects, and developmental factors.
Where can I find a free Naranjo Scale calculator?
Yes. An open-source Python-based Naranjo Calculator is available on GitHub and has over 2,100 stars. Some electronic health record systems, like Epic’s Safety Module, also auto-fill parts of the scale. Free worksheets and training modules are available from Nebraska ASAP and the International Society of Pharmacovigilance.
How long does it take to learn the Naranjo Scale?
Most people can learn the basics in 2-4 hours of training. But becoming confident takes practice. Health professionals typically need 20-30 real cases to use it reliably. Nurses and pharmacists report mastering it after 3-5 practice sessions.
Does the Naranjo Scale work for new drugs like biologics or immunotherapies?
It’s limited. The scale was built for traditional small-molecule drugs. New therapies like immunotherapies can cause delayed reactions months after stopping, which the scale doesn’t account for. Experts say it struggles with these modern treatments and should be used alongside newer assessment methods.






Bridget Molokomme
February 3, 2026 AT 06:52Bob Hynes
February 5, 2026 AT 06:23larry keenan
February 5, 2026 AT 08:04Akhona Myeki
February 5, 2026 AT 21:28Chinmoy Kumar
February 7, 2026 AT 06:30Ansley Mayson
February 8, 2026 AT 09:35phara don
February 10, 2026 AT 04:05Hannah Gliane
February 11, 2026 AT 00:27Murarikar Satishwar
February 11, 2026 AT 23:31Dan Pearson
February 13, 2026 AT 05:25