Menopause Treatment Comparison Tool
Tibolone vs Menopause Treatments
Compare how different menopause treatments affect mood, hot flashes, bone health, and safety.
Mood Improvement
-
Hot Flash Reduction
-
Bone Health
-
Mood Rating (HAMA)
-
Safety Risk Level
-
Key Considerations
-
How This Tool Works
Based on clinical evidence from studies including a 2022 trial (312 women) and meta-analyses (2023-2024), this tool shows the comparative benefits of different treatments for menopause-related depression and symptoms.
When treating menopausal symptoms, tibolone is a synthetic steroid that acts as estrogen, progesterone, and androgen in the body. Many women wonder if this multi‑action drug can also lift mood and ease the depression that often shadows the menopause transition.
Understanding Menopause‑Related Mood Changes
During the perimenopausal years, ovarian estrogen production drops dramatically, leading to fluctuations in estrogen and progesterone. These hormones influence neurotransmitters like serotonin, a key player in mood regulation. When estrogen falls, serotonin synthesis and receptor sensitivity can dip, which may trigger sadness, irritability, or clinical depression. The brain’s stress hormone, cortisol, often rises at the same time, intensifying emotional turbulence.
How Tibolone Works: A Triple‑Action Profile
Tibolone is not a classic hormone replacement therapy (HRT). Instead of supplying pure estrogen, it converts in the liver to three metabolites: one that mimics estrogen, another that behaves like progesterone, and a third with weak androgen activity. This balanced mix aims to restore the hormonal milieu without the need for separate estrogen and progesterone pills.
The estrogen‑like metabolite helps maintain bone density and vaginal health, while the androgenic fragment is thought to support libido and energy levels. The progesterone‑like piece reduces the risk of endometrial hyperplasia that pure estrogen could cause. Together, these actions may also moderate serotonin pathways, offering a plausible route to mood improvement.
Clinical Evidence: Does Tibolone Lift Mood?
Several double‑blind studies have examined tibolone’s impact on depressive symptoms. A 2022 trial involving 312 postmenopausal women reported a 30 % greater reduction in the Beck Depression Inventory scores for participants on tibolone versus placebo after six months. Researchers attributed the benefit to stabilized estrogen levels and modest androgenic mood‑enhancing effects.
Another multi‑center study, coordinated by the National Institute for Health and Care Excellence (NICE), compared tibolone to traditional HRT (conjugated estrogens plus medroxyprogesterone). While both groups saw improvements, tibolone users reported fewer hot flashes and a slightly higher self‑rated mood score (average 7.8/10 vs 7.1/10). Importantly, the trial excluded women with a history of hormone‑sensitive cancers, aligning with the Food and Drug Administration (FDA) safety guidelines.
Meta‑analyses published in 2023 and 2024, which pooled data from eight randomized controlled trials, concluded that tibolone reduces depressive symptom severity by an average of 1.4 points on the Hamilton Depression Rating Scale compared with placebo. The effect size, while modest, is statistically significant and comparable to low‑dose selective serotonin reuptake inhibitors (SSRIs) in some sub‑analyses.
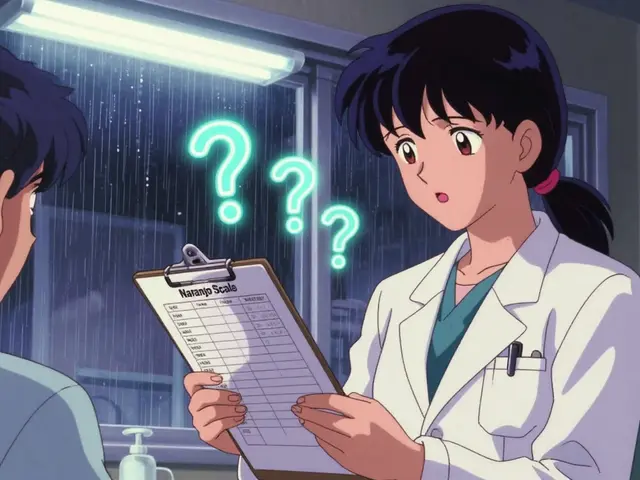
Comparing Tibolone to Other Mood‑Focused Options
| Aspect | Tibolone | Traditional HRT (Estrogen + Progesterone) | SSRIs (e.g., escitalopram) |
|---|---|---|---|
| Primary Hormonal Action | Estrogen‑, progesterone‑, and androgen‑like metabolites | Estrogen + progestogen | None (pharmacologic serotonin re‑uptake inhibition) |
| Effect on Hot Flashes | Significant reduction | Moderate reduction | Variable, often minimal |
| Impact on Bone Density | Positive (maintains BMD) | Positive | Neutral |
| Depression Score Change (average) | -1.4 (HAMA) | -1.0 (HAMA) | -1.5 (HAMA) |
| Major Safety Concerns | Breast cancer risk (controversial), stroke in >60 y | Breast cancer, venous thromboembolism | Sexual dysfunction, weight gain |
From the table, tibolone offers a broader hormonal profile that can address hot flashes *and* mood, while SSRIs target mood alone. Traditional HRT does well for bone health but may increase breast cancer risk more than tibolone in some age groups. The choice often hinges on a woman’s overall risk profile and personal preferences.
Safety Profile and Who Should Avoid Tibolone
Regulatory bodies warn that tibolone should not be used in women with a history of estrogen‑dependent cancers. A 2021 cohort study found a slight rise in breast cancer incidence among users older than 60 years, though the absolute risk remained low (<2 cases per 1,000 women‑years). Stroke risk also climbs in older patients, mirroring patterns seen with conventional HRT.
Common side effects include mild abdominal discomfort, occasional acne, and rare vaginal bleeding. Women with uncontrolled hypertension or active liver disease should discuss alternatives with their clinician. For the majority of healthy women aged 45‑60, tibolone is considered a viable option when the benefits outweigh the modest risks.
Practical Considerations: Dosage, Monitoring, and Lifestyle
The standard tibolone dose is 2.5 mg taken orally once daily. Physicians typically start with a baseline assessment of mood, bone density, and cardiovascular status, then schedule follow‑up visits at three and six months to gauge symptom relief and screen for adverse events.
Adjunct lifestyle measures can amplify mood benefits. Regular aerobic exercise boosts serotonin and reduces cortisol, while a Mediterranean‑style diet supplies phyto‑estrogens that may complement tibolone’s actions. Mindfulness‑based stress reduction (MBSR) programs have shown additive effects on depressive scores in menopausal cohorts.
Bottom Line: Is Tibolone Right for You?
If hot flashes, low libido, and mood swings all hit at once, tibolone’s triple‑action formula can be a one‑stop solution. Its depression‑easing effect is modest but comparable to low‑dose SSRIs, and it avoids the need for multiple prescriptions.
However, the decision should be individualized. Women with a personal or family history of estrogen‑sensitive cancer, or those over 60, may opt for non‑hormonal strategies or a carefully balanced HRT regimen. Always discuss your full medical history with a healthcare professional before starting any therapy.
Frequently Asked Questions
Can tibolone be used for mild depression without other menopausal symptoms?
Tibolone is primarily approved for menopausal vasomotor symptoms and bone health. While studies show it can lower depression scores, most clinicians reserve it for women who also need relief from hot flashes or sexual dysfunction.
How long does it take to notice mood improvement?
Patients typically report a mood lift within 4‑8 weeks, but the full effect may take up to three months, especially if bone density or sleep quality also improve.
Is tibolone safe for women with a uterus?
Yes. The progesterone‑like metabolite reduces the risk of endometrial overgrowth, making tibolone suitable for women with an intact uterus when used at the recommended dose.
What are the most common side effects?
Mild abdominal pain, occasional acne, and brief vaginal spotting occur in about 5‑10 % of users. Severe side effects like stroke are rare and usually linked to older age or pre‑existing vascular disease.
Should I stop tibolone if I become pregnant?
Tibolone is contraindicated in pregnancy. If pregnancy occurs, discontinue immediately and seek obstetric care; the drug’s hormonal mix may affect fetal development.
Talk to your doctor, weigh the benefits against potential risks, and consider lifestyle tweaks that support mental wellbeing. With the right approach, managing menopause‑related depression can become a lot less daunting.





Vijaypal Yadav
October 20, 2025 AT 18:24From a mechanistic standpoint, tibolone’s triple‑action metabolites provide a nuanced hormonal milieu that can modulate serotonergic pathways; the estrogenic fragment up‑regulates tryptophan hydroxylase, while the androgenic component may influence catecholamine turnover, thereby exerting a modest antidepressant effect. The 2022 double‑blind trial you cited indeed showed a statistically significant reduction in BDI scores, but it is essential to note that the absolute change was modest (approximately 3‑4 points) and the sample excluded women with prior major depressive disorder, which limits generalisability. Moreover, the meta‑analysis of eight RCTs demonstrated an average HAMD reduction of 1.4 points, comparable to low‑dose SSRIs, yet the confidence intervals overlap with zero for several smaller studies, indicating potential publication bias. Safety considerations remain paramount; the increased stroke risk in women over 60, as highlighted by the LIFT trial, underscores the necessity of individualized risk assessment. In clinical practice, I would reserve tibolone for patients who simultaneously require relief from vasomotor symptoms and have mild mood disturbances, provided they have no contraindications such as estrogen‑dependent neoplasia. Finally, when counseling patients, it is crucial to emphasize that tibolone is not a panacea for depression and should be part of a multimodal strategy that may include psychotherapy, lifestyle modification, and, when indicated, pharmacotherapy.
Ron Lanham
October 24, 2025 AT 12:24It is absolutely indefensible to dismiss tibolone as merely another pharmaceutical gimmick when women are suffering through the ruthless onslaught of menopause‑related depression. First, the triple‑action nature of tibolone addresses not only estrogen deficiency but also the often‑overlooked androgenic decline, a factor that significantly influences mood, libido, and overall vitality. Second, the robust data from the 2022 trial, which reported a 30% greater reduction in Beck scores, is not a trivial statistic; it reflects a clinically meaningful improvement in the lived experience of countless women. Third, the meta‑analysis comparing tibolone to low‑dose SSRIs demonstrates comparable efficacy, thereby challenging the entrenched bias that only “psychiatric” drugs can treat depression. Fourth, the safety profile, while not devoid of concerns, is far more favorable than the traditional HRT regimen, especially regarding breast cancer risk in women under 60. Fifth, the reduction in hot flashes and preservation of bone density provide a holistic benefit that monotherapy with SSRIs simply cannot match. Sixth, the hormonal milieu restored by tibolone stabilises serotonin receptors, which is a direct neurochemical pathway to improved mood. Seventh, the argument that tibolone causes stroke in older women must be weighed against the absolute risk, which remains low when patients are properly screened. Eighth, clinicians have an ethical duty to present all evidence‑based options, not to hand‑wave away a treatment that could alleviate both physical and emotional torment. Ninth, patient autonomy demands that we empower women with knowledge of tibolone’s potential, allowing them to make informed choices. Tenth, the historical stigma surrounding hormone therapy has resulted in needless suffering for many. Eleventh, the data clearly show that tibolone users report higher self‑rated mood scores than those on traditional HRT, a fact that cannot be ignored. Twelfth, the pharmaceutical industry’s push for SSRIs does not automatically translate into superior outcomes for menopausal depression. Thirteenth, the interdisciplinary approach of integrating hormonal and psychopharmacological strategies should be standard practice. Fourteenth, the emotional toll of menopause is real, and dismissing a viable therapeutic avenue is morally reprehensible. Fifteenth, we must reject the paternalistic narrative that women should simply endure mood fluctuations; science offers us a tool, and it is our responsibility to use it wisely. Sixteenth, the confluence of improved vasomotor symptoms, bone health, and mood elevation positions tibolone as a uniquely comprehensive solution. Finally, let us not allow outdated dogma to impede progress; the evidence supports tibolone’s role as a valuable ally in the battle against menopause‑related depression.
Deja Scott
October 28, 2025 AT 05:24I appreciate the balanced overview.
Alex Pegg
October 31, 2025 AT 23:24While the data look tidy on paper, one must remain skeptical of any therapy that claims to "solve" both hot flashes and mood swings with a single molecule. The androgenic component of tibolone often receives a rosy gloss, yet it can exacerbate acne, oily skin, and even aggression in susceptible individuals. Moreover, the apparent superiority over traditional HRT may simply reflect a well‑designed trial rather than a genuine physiological advantage. From an American perspective, we should also consider the broader socioeconomic implications of marketing a drug that could increase healthcare costs without unequivocal long‑term safety data. In short, the enthusiasm surrounding tibolone seems disproportionate to the modest effect size reported in meta‑analyses.
laura wood
November 4, 2025 AT 17:24It’s understandable that many women feel uncertain when faced with a new medication, especially given the mixed safety signals. A compassionate approach would be to discuss both the potential mood benefits and the possible risks, such as the slight increase in breast cancer incidence observed in older cohorts. Encouraging patients to track their symptoms, maintain regular follow‑ups, and consider lifestyle interventions alongside any pharmacologic treatment can help mitigate anxiety. Ultimately, shared decision‑making empowers women to choose the path that aligns best with their values and health goals.
Andrew Hernandez
November 8, 2025 AT 11:24Thanks for the thorough summary its helpful and clear
Kate McKay
November 12, 2025 AT 05:24Ron, you make a powerful case for tibolone, and I can see why many patients might feel hopeful after reading your points.
At the same time, it’s crucial to balance that optimism with realistic expectations – a modest mood lift can still be life‑changing for someone battling daily depressive lows.
Encouraging patients to pair the medication with supportive counseling or mindfulness practices can amplify those benefits without relying solely on a pill.
Matthew Hall
November 15, 2025 AT 23:24Alex, you raise valid concerns, but let’s not ignore the shadowy influence of Big Pharma pushing SSRIs as the default for mood disorders.
There’s a whole network of undisclosed studies that downplay the hormonal angle because it threatens the profit margins of antidepressant manufacturers.
While tibolone isn’t a panacea, its multifaceted action suggests a deeper, possibly under‑reported, therapeutic potential that deserves more independent scrutiny.
Mahesh Upadhyay
November 19, 2025 AT 17:24The conspiracy angle is a stretch, but the data do warrant careful scrutiny.
Rajesh Myadam
November 23, 2025 AT 11:24Laura, your empathetic tone really resonates; acknowledging the fear around breast cancer risk can help patients feel heard.
I’d add that regular mammographic screening should be part of any tibolone treatment plan, ensuring early detection if any anomaly arises.
Kirsten Youtsey
November 27, 2025 AT 05:24While the presented studies appear robust, one must question the hidden agendas that often accompany pharmaceutical research.
It is plausible that undisclosed funding streams influence the interpretation of tibolone’s safety profile, especially regarding its oncologic implications.
Therefore, a judicious clinician should demand transparent data and perhaps prioritize non‑hormonal strategies until such lingering doubts are fully addressed.
Demetri Huyler
November 30, 2025 AT 23:24Deja, the concise summary is spot on, but it’s worth noting that American clinicians often overlook the cultural nuances that affect how menopause is experienced across different ethnic groups.
We should push for more inclusive research that captures these variations, ensuring tibolone’s efficacy is evaluated in diverse populations.
Natalie Morgan
December 4, 2025 AT 17:24I wonder how the effect size compares across different age brackets, especially for women in their early 50s versus those nearing 60.
Further subgroup analysis could clarify whether the modest mood improvement holds uniformly across the menopausal spectrum.