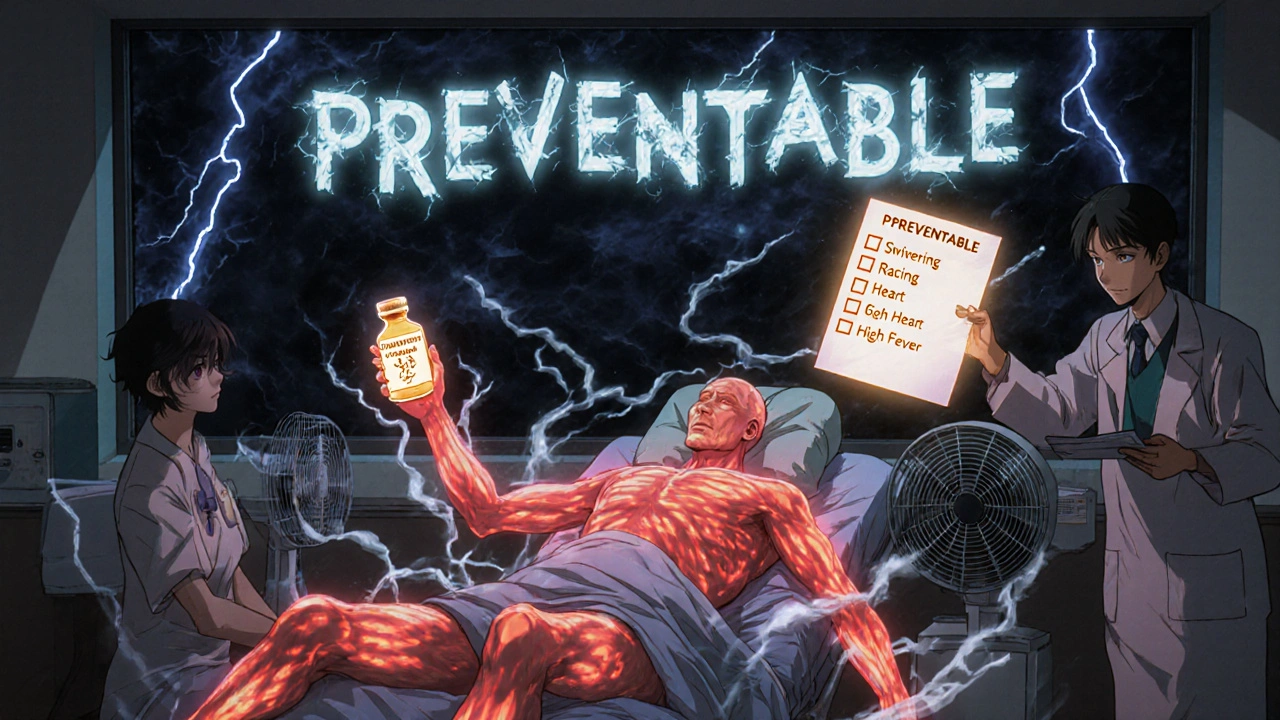
Combining SSRIs and opioids might seem harmless if you're managing both depression and pain. But for thousands of people, this common mix can trigger something dangerous: serotonin syndrome. It doesn't happen often, but when it does, it can turn deadly in hours. You won't always know it's coming-symptoms start mild, like shivering or a racing heart, then spiral into muscle rigidity, high fever, and seizures. And here's the scary part: many doctors miss it at first. It’s often mistaken for infection, anxiety, or even a drug overdose. The truth? This isn’t rare. In the U.S. alone, over 800 cases were reported between 2018 and 2022 just from opioid-SSRI combinations. And tramadol? It’s behind nearly 4 out of 10 of those cases.
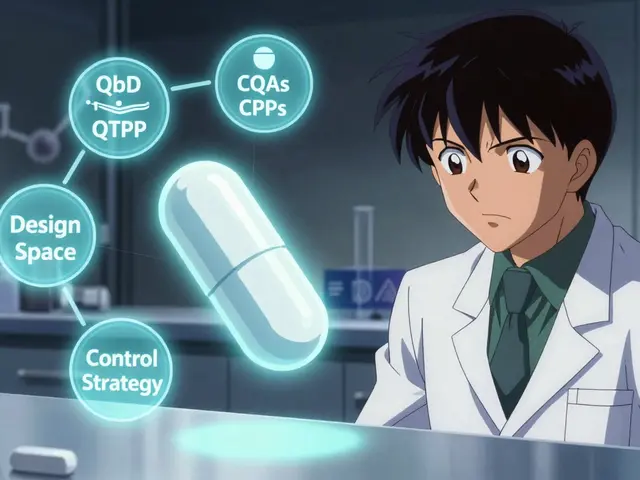
What Exactly Is Serotonin Syndrome?
Serotonin syndrome isn’t an allergy. It’s a chemical overload. Your brain uses serotonin to control mood, sleep, and pain. SSRIs like sertraline, fluoxetine, and escitalopram stop your body from reabsorbing serotonin, so more stays active in your brain. Opioids like tramadol, methadone, and pethidine do something similar-they block the serotonin transporter (SERT), which is the system that normally clears serotonin from between nerve cells. When both types of drugs are taken together, serotonin piles up faster than your body can handle. Too much serotonin overstimulates receptors, especially 5-HT1A and 5-HT2A, and your nervous system goes into overdrive.
The symptoms come on fast-often within hours of taking a new dose or increasing one. Mild cases include sweating, tremors, diarrhea, and a heart rate over 100 beats per minute. Severe cases? Core body temperature can spike above 41°C (106°F), muscles lock up, you may have seizures, or fall into a coma. About 1 in 10 people with severe serotonin syndrome die if it’s not treated immediately. And because symptoms mimic other conditions, many patients wait too long to get help.
Not All Opioids Are Equal
Here’s the critical thing: not every opioid carries the same risk. Some are quiet. Others are loud. If you’re on an SSRI and need pain relief, your choice of opioid matters more than you think.
- High-risk opioids: Tramadol, methadone, and pethidine (meperidine) directly block serotonin reuptake. Tramadol is especially dangerous-it’s 30 times stronger at inhibiting serotonin than morphine. In fact, studies show tramadol combined with an SSRI is over four times more likely to cause serotonin syndrome than morphine with an SSRI.
- Lower-risk opioids: Morphine, oxycodone, hydromorphone, and buprenorphine don’t significantly interfere with serotonin transporters. They’re still opioids, so they carry addiction risks, but they’re far safer when paired with SSRIs.
- Confusing cases: Fentanyl doesn’t block serotonin in lab tests, yet over 120 real-world cases of serotonin syndrome have been linked to it. Why? It may directly stimulate serotonin receptors. Codeine was once thought to be safe-but there are documented cases where even codeine triggered serotonin syndrome in people already on SSRIs.
And it’s not just about the opioid. The SSRI you’re on matters too. Fluoxetine sticks around in your body for weeks-even after you stop taking it. Norfluoxetine, its active metabolite, can linger for over two weeks. That means if you switch from fluoxetine to an opioid, you’re still at risk for days or even weeks after stopping. Sertraline? It clears out in about a day. Big difference.
Who’s Most at Risk?
It’s not just about the drugs you take-it’s about your body’s ability to handle them. Certain people are far more vulnerable.
- Older adults: People over 65 take, on average, 31% more medications than younger adults. That means more chances for interactions. The American Geriatrics Society specifically warns against prescribing tramadol to seniors already on SSRIs.
- People with liver or kidney problems: If your liver can’t break down drugs or your kidneys can’t flush them out, serotonin builds up faster. A standard dose of tramadol can become toxic in someone with cirrhosis or chronic kidney disease.
- Genetic factors: About 7% of people are poor metabolizers of CYP2D6, the enzyme that breaks down tramadol and some SSRIs. These individuals can’t process the drugs normally, so serotonin levels climb dangerously even at low doses. Studies show they’re over three times more likely to develop serotonin syndrome.
- People recently starting or increasing doses: Over 80% of serotonin syndrome cases happen within hours of a new dose or a dose increase. That’s why it’s so easy to miss-the connection feels coincidental.
How to Prevent It
Prevention isn’t complicated-it’s about awareness, communication, and smart choices.
- Avoid high-risk combinations altogether. If you’re on an SSRI or SNRI, don’t take tramadol, methadone, or pethidine. Period. There are safer alternatives like morphine or oxycodone for pain.
- Check your meds with your pharmacist. Don’t assume your doctor knows every drug you’re taking. Pharmacists see the full picture. Ask: “Is this opioid safe with my antidepressant?”
- Know your SSRI’s half-life. If you’re on fluoxetine, wait at least five weeks before starting a new opioid. For sertraline or escitalopram, a week is usually enough. Never switch cold turkey.
- Use electronic alerts. Hospitals and clinics using modern EHR systems like Epic have started building hard stops for dangerous combinations. If your doctor prescribes tramadol while you’re on an SSRI, the system should flag it. If it doesn’t, speak up.
- Start low, go slow. If you absolutely must combine a lower-risk opioid with an SSRI, start at half the normal dose. Monitor for symptoms for at least 72 hours.
Patients should also carry a simple symptom checklist: Shivering I can’t stop? Muscle twitching? Fast heartbeat? Feeling overheated? Agitated or confused? If any of these show up after starting a new pain med, stop taking it and get help immediately.
What to Do If It Happens
If you suspect serotonin syndrome, don’t wait. Go to the ER. Time is everything.
- Stop all serotonergic drugs. That includes your SSRI, the opioid, and any supplements like St. John’s Wort or tryptophan.
- Get benzodiazepines. Medications like lorazepam calm the nervous system, reduce muscle rigidity, and lower the risk of seizures.
- Use cyproheptadine. This antihistamine blocks serotonin receptors. Doctors give 12 mg initially, then 2 mg every two hours until symptoms improve. It’s not available over the counter, but ERs keep it on hand.
- Cool the body. If your temperature is above 39°C (102°F), external cooling with ice packs and fans is critical. Internal cooling may be needed in severe cases.
There’s no blood test for serotonin syndrome. Diagnosis is based on symptoms and drug history using the Hunter Criteria-specific combinations like spontaneous clonus, or inducible clonus with agitation and sweating. If your doctor doesn’t know these criteria, ask for a pharmacist or toxicologist to consult.
The Bigger Picture
This isn’t just about one bad combo. It’s about how we treat pain and depression together. Over 21% of opioid prescriptions in 2022 went to people already on antidepressants. That’s millions of people at risk. Regulatory agencies are catching up-the FDA now requires opioid medication guides to include serotonin syndrome warnings, and the EMA updated tramadol labels in 2021. But real change needs to happen at the point of care.
Hospitals like Kaiser Permanente cut dangerous tramadol-SSRI prescriptions by 87% after adding clinical decision alerts. That’s proof it works. And research is moving forward: the NIH is funding $2.4 million to find early biomarkers for serotonin syndrome, and Epic Systems is building tools to analyze 17 genetic interactions by 2024.
For now, the message is simple: if you’re on an SSRI and your doctor suggests tramadol for pain, say no. Ask for morphine or oxycodone instead. If you’ve been on fluoxetine for years and just got a new pain script, pause. Talk to your pharmacist. Don’t assume it’s safe just because both drugs are legal and prescribed.
Serotonin syndrome is preventable. But only if you know what to look for-and who to ask.
Can you get serotonin syndrome from taking tramadol and sertraline together?
Yes. Tramadol blocks serotonin reuptake, and sertraline prevents it from being cleared from the brain. Together, they cause serotonin to build up rapidly. This combination is one of the most common causes of serotonin syndrome in real-world settings. Cases have been documented within hours of starting the combo, even at normal doses.
Is morphine safe to take with SSRIs?
Yes, morphine is considered a low-risk opioid when combined with SSRIs. It doesn’t significantly inhibit the serotonin transporter (SERT) or stimulate serotonin receptors. It’s often recommended as a safer alternative to tramadol or methadone for patients on antidepressants. But always start with a lower dose and monitor for symptoms.
How long after stopping fluoxetine is it safe to start an opioid?
Because fluoxetine and its active metabolite, norfluoxetine, stay in your system for up to 16 days after your last dose, you should wait at least five weeks before starting any opioid that affects serotonin-like tramadol or methadone. For other SSRIs like sertraline or escitalopram, a one-week washout is usually sufficient.
Can codeine cause serotonin syndrome?
Yes. Although codeine doesn’t strongly inhibit serotonin in lab tests, real-world case reports show it has triggered serotonin syndrome in people already taking SSRIs like paroxetine. This suggests other mechanisms may be involved, such as active metabolites or individual sensitivity. Never assume a drug is safe just because it’s "mild."
What should I do if I think I have serotonin syndrome?
Stop taking all serotonergic drugs immediately. Go to the nearest emergency room. Do not wait. Symptoms like uncontrollable shivering, muscle rigidity, fast heartbeat, or high fever need urgent treatment. Bring a list of all your medications. Treatment includes benzodiazepines, cyproheptadine, and cooling measures. Early action saves lives.
Are there any over-the-counter supplements that increase serotonin syndrome risk?
Yes. St. John’s Wort, tryptophan, and 5-HTP are all supplements that increase serotonin levels. Taking them with SSRIs or certain opioids can trigger serotonin syndrome-even if you’re not on prescription medication. Always tell your doctor or pharmacist about any supplements you take.
Can serotonin syndrome happen with just one drug?
Yes, but it’s rare. It usually happens with overdose, or in people with impaired metabolism (like CYP2D6 poor metabolizers). Tramadol alone has caused serotonin syndrome in patients with kidney failure or genetic variations that slow its breakdown. It’s not common, but it’s possible.
Bottom line: if you’re on an SSRI, treat every new pain medication like a potential trigger. Ask questions. Don’t accept "it’s fine" without proof. Your life might depend on it.






Georgia Green
November 17, 2025 AT 00:29Just had my doc switch me from tramadol to oxycodone last month after I mentioned I was on sertraline. She didn’t even know the risk. Scary how common this is. Thanks for the clarity.
Ashley Unknown
November 18, 2025 AT 08:13OMG I KNEW IT. I’ve been saying this for YEARS. Big Pharma doesn’t want you to know this because they make billions off these deadly combos. Tramadol? It’s literally a chemical weapon disguised as pain relief. And don’t get me started on how the FDA is bought off by pharma lobbyists. I’ve seen people go into seizures from this-my cousin almost died. They buried the data. I’ve got screenshots. You think this is an accident? No. It’s systemic. They profit off your suffering. Wake up. This isn’t medicine-it’s a slaughterhouse with a white coat. And they’ll tell you it’s ‘rare’ until your organs shut down. I’m not paranoid. I’m informed. And I’m not the only one. Check the VA records. 800 cases? That’s the tip of the iceberg. They’re silencing the whistleblowers. I’ve got emails. I’ll post them. Someone needs to sue. Someone needs to burn it all down.
Christina Abellar
November 19, 2025 AT 09:10Thank you for this. I’m on escitalopram and was prescribed oxycodone after surgery-my pharmacist flagged it immediately. So glad I asked.
Margo Utomo
November 20, 2025 AT 17:23Yessssss 🙌 This is the kind of post that should be mandatory reading before any pain script is written. Seriously, if your doctor doesn’t know this, find a new one. Also, St. John’s Wort? That stuff’s basically a serotonin bomb. I used to take it ‘naturally’-now I know better. 🙏
Matt Wells
November 22, 2025 AT 03:25The scientific accuracy of this post is commendable, though I must note that the term 'chemical overload' is imprecise. Serotonin syndrome is a pharmacodynamic receptor-mediated phenomenon, not a mere accumulation. Furthermore, the assertion that tramadol is '30 times stronger' than morphine in SERT inhibition is misleading without contextualizing IC50 values. Still, the clinical guidance is sound.
Eva Vega
November 22, 2025 AT 15:18As a clinical pharmacist, I see this every day. The CYP2D6 poor metabolizer issue is grossly underdiagnosed-especially in older adults on polypharmacy. We run pharmacogenetic panels now for anyone on tramadol + SSRI. If your hospital doesn’t, demand it. Also, fluoxetine’s half-life is the silent killer here. I’ve had patients come in with serotonin syndrome two weeks after stopping it. No one connects the dots.
George Gaitara
November 23, 2025 AT 05:54Wow. Another fear-mongering article. You say tramadol is dangerous, but what about the millions who take it safely? You’re ignoring the fact that most cases occur with overdose or polypharmacy. This is just scare tactics to push people toward more expensive opioids. Morphine isn’t ‘safe’-it’s just less flashy. And why aren’t you talking about the opioid crisis? This feels like a distraction.
Sylvia Clarke
November 24, 2025 AT 02:46Let’s be real-this isn’t about ‘risk,’ it’s about systemic negligence. We’ve got AI-driven EHRs that could flag every dangerous combo in real time… but hospitals still rely on paper charts and ‘trust your doctor.’ Meanwhile, patients are being turned into lab rats. And don’t even get me started on how pharmacies don’t get paid for counseling, so they skip the conversation entirely. We’ve got the tools. We just lack the will. Someone needs to sue the AMA for malpractice by omission. This is preventable. And it’s not just ‘rare.’ It’s routine.
Deepali Singh
November 25, 2025 AT 12:36Statistical noise. 800 cases in 5 years across 330M people? That’s 0.00024%. You’re equating correlation with causation. Most of these cases involved polypharmacy, illicit substances, or non-compliance. The real issue is patient non-adherence and poor clinical judgment-not the drugs themselves. This post is emotionally manipulative, not evidence-based.
Jennifer Howard
November 25, 2025 AT 23:56How can anyone be so irresponsible? I am a mother of three. I take sertraline. I was prescribed tramadol for a back injury. I did not question it. I am now terrified. This is not just medical negligence-it is moral failure. Doctors are not gods. They are fallible. And patients are not idiots. We deserve better. I will be writing to my state medical board. This is unacceptable. I will not be silent. I will not let this happen to another person. I will not.
Joyce Genon
November 26, 2025 AT 19:48Oh please. This is just another ‘dangerous combo’ panic. You say morphine is ‘safe’? What about respiratory depression? What about addiction? You’re swapping one risk for another. And why are you ignoring the fact that serotonin syndrome is often misdiagnosed as neuroleptic malignant syndrome or heat stroke? This entire narrative is built on cherry-picked data. Also, why no mention of MAOIs? Oh right-because those are even deadlier, and nobody wants to talk about them. This isn’t education. It’s fear porn.
John Wayne
November 27, 2025 AT 09:47Tramadol is a weak opioid with a serotonin effect. So? Many drugs have multiple mechanisms. This isn’t a revelation. It’s pharmacology 101. The real problem is that people think they’re experts after reading one article. You don’t get to play doctor because you read a PubMed abstract. Trust your physician. They’ve spent 12 years training. You’ve spent 10 minutes scrolling.
Abdul Mubeen
November 28, 2025 AT 17:42Interesting how this post conveniently omits the fact that the CDC and WHO both state that the risk is negligible when used as directed. Also, why is there no mention of the 2019 Lancet study that found no significant increase in serotonin syndrome with tramadol/SSRI in controlled populations? This feels like an anti-pharma campaign disguised as patient safety. The truth? You’re being manipulated by alarmist content creators. Look at the funding sources. Who paid for this?