One glass of grapefruit juice in the morning might seem harmless-maybe even healthy. But if you're taking certain medications, that glass could be dangerous. It doesn't matter if you drink it with breakfast, after your pill, or hours later. The interaction doesn’t wait for convenience. It happens quietly, inside your gut, and it can turn a safe dose into a toxic one.
Why Grapefruit Juice Changes How Your Medication Works
Grapefruit juice doesn’t just add flavor-it changes how your body handles drugs. The problem isn’t sugar or acidity. It’s a group of natural chemicals called furanocoumarins, mainly bergamottin and 6',7'-dihydroxybergamottin. These compounds shut down an enzyme in your intestines called CYP3A4. This enzyme normally breaks down about half of all oral medications before they enter your bloodstream. When it’s blocked, your body absorbs way more of the drug than it should.That sounds like a good thing-more drug, more effect, right? Wrong. Too much drug in your blood means side effects get worse, sometimes dangerously so. The effect isn’t temporary. Even one 200-milliliter glass (about 6.7 ounces) can block CYP3A4 for up to 72 hours. That means if you drink grapefruit juice on Monday, your body is still affected on Thursday. The FDA says patients should avoid grapefruit products the entire time they’re on these medications-not just at the same time as taking the pill.
Which Medications Are Most at Risk?
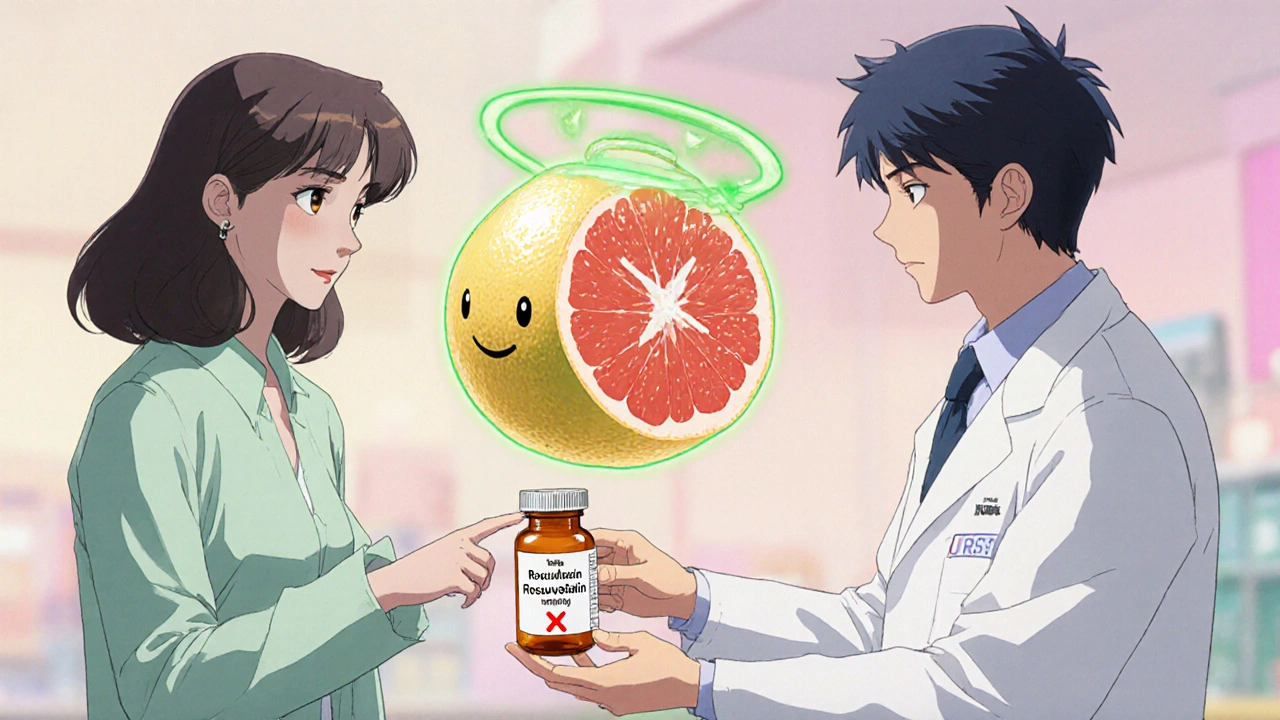
More than 85 prescription drugs have documented interactions with grapefruit juice. Of those, 43 can cause life-threatening reactions. Not all drugs react the same way. Here are the biggest red flags:- Statins (cholesterol drugs): Simvastatin (Zocor) is the most dangerous. Just one glass a day for three days can triple its levels in your blood. That raises your risk of rhabdomyolysis-a condition where muscle tissue breaks down and can lead to kidney failure. Atorvastatin (Lipitor) has a milder interaction, but it’s still risky. Pravastatin and rosuvastatin? Safe. No interaction.
- Calcium channel blockers (blood pressure meds): Felodipine (Plendil) sees a five-fold increase in blood levels. Nifedipine (Procardia) jumps by 3.3 times. Amlodipine (Norvasc)? Minimal effect. The difference matters.
- Immunosuppressants: Cyclosporine (Neoral), used after transplants, can spike 50-60% higher with grapefruit juice. That raises the risk of kidney damage.
- Antiarrhythmics: Amiodarone (Cordarone) can increase plasma levels by 30-40%, which may trigger irregular heart rhythms.
- Some psychiatric drugs: Certain benzodiazepines and sedatives like midazolam are affected. But trazodone and zolpidem? Studies show little to no interaction.
It’s not just pills. Some over-the-counter drugs and supplements also interact. Fexofenadine (Allegra), an antihistamine, becomes less effective with grapefruit juice because the juice blocks a different transporter protein (OATP). So now your allergy meds don’t work-and you don’t know why.
Not All Citrus Is the Same
You might think all citrus fruits are risky. They’re not. Only grapefruit and its close relatives cause this problem. Seville oranges (used in marmalade) and pomelos contain the same furanocoumarins. So if you’re on a high-risk medication, skip those too.Sweet oranges (like navel or Valencia), lemons, limes, and tangerines? Safe. They don’t have the chemicals that block CYP3A4. So you can still enjoy your morning orange juice without worry.
Why Some People Are More Affected Than Others
Not everyone reacts the same way. One study found that after drinking grapefruit juice, some people had zero increase in drug levels. Others saw an 8-fold spike. Why? It comes down to your gut biology.People naturally have different levels of CYP3A4 in their intestines. Those with higher baseline levels get hit harder when the enzyme is blocked. It’s like turning off a faucet that’s already flowing fast-everything backs up. But there’s no test to measure your CYP3A4 levels. So doctors can’t predict who’s at higher risk.
Age matters too. People over 65 are more likely to be on multiple medications-and more likely to drink grapefruit juice regularly. USDA data shows older adults make up 40% of grapefruit consumers. They’re also the group most likely to take 3-5 drugs that could interact. That’s a dangerous combo.
What to Do If You’re on a High-Risk Medication
If you’re taking any of the drugs listed above, here’s what to do:- Check your prescription label. Since 2014, the FDA has required manufacturers to include grapefruit warnings on affected drug labels. Look for phrases like “Avoid grapefruit juice” or “Do not consume grapefruit products.”
- Ask your pharmacist. A 2021 study found that 89% of community pharmacists screen for grapefruit interactions when dispensing medication. Don’t assume they’ll bring it up-ask.
- Make a complete medication list. Include every pill, patch, supplement, and herbal product. Bring it to every appointment. Many interactions happen because patients forget to mention their vitamins or over-the-counter meds.
- Consider alternatives. If you love grapefruit and are on simvastatin, ask your doctor about switching to pravastatin or rosuvastatin. If you’re on cyclosporine, tacrolimus might be a safer option. These switches are common and often effective.
What About Juice That’s “Fresh-Squeezed” vs. Store-Bought?
Fresh-squeezed grapefruit juice has the highest concentration of furanocoumarins. Pasteurized or bottled juice? Still risky. Studies show even processed juice retains enough of the chemicals to cause major interactions. So don’t assume “no pulp” or “100% juice” means it’s safe. It’s not.And don’t be fooled by “low-sugar” or “diet” grapefruit juices. They still contain the same furanocoumarins. The sugar content doesn’t affect the enzyme inhibition.
What’s Being Done to Fix This?
Scientists are working on solutions. In October 2023, the USDA announced that CRISPR-edited grapefruit with 90% less furanocoumarin had passed early safety trials. These aren’t on shelves yet-but they’re coming. The hope is to create a version that tastes like grapefruit but won’t interfere with meds.In the meantime, regulators are tightening rules. The European Medicines Agency now requires all new oral drugs metabolized by CYP3A4 to be tested for grapefruit interactions. The FDA’s 2020 guidance made this part of standard drug development. That means fewer new drugs will slip through without warnings.
Why So Many People Still Don’t Know
Despite decades of research and clear warnings, patient awareness is shockingly low. A 2022 survey by the National Community Pharmacists Association found only 38% of patients recalled being told about grapefruit interactions when prescribed a risky drug. That’s not because doctors are negligent-it’s because the conversation gets buried under other priorities. Patients assume “natural” means “safe.”But grapefruit isn’t harmless because it’s fruit. It’s powerful because it’s biochemical. It’s not about calories or antioxidants. It’s about a silent, irreversible chemical lock on your body’s drug-processing system.
Bottom Line: When in Doubt, Skip It
If you’re on any medication-especially for heart disease, high cholesterol, high blood pressure, or after an organ transplant-don’t risk it. Even if you’ve had grapefruit juice for years without problems, your body’s chemistry can change. So can your meds. A new prescription, a dose change, or even a different brand of the same drug can alter your risk.The safest choice? Avoid grapefruit juice entirely while taking high-risk medications. And if you’re unsure, ask. Show your pharmacist your pill bottle. Ask your doctor: “Could grapefruit juice interfere with this?” It’s a simple question that could save your life.
Can I drink grapefruit juice if I take my medication at night?
No. The interaction isn’t about timing-it’s about enzyme suppression. Grapefruit juice blocks CYP3A4 in your intestines for up to 72 hours. Whether you take your pill in the morning or at night, if you drank grapefruit juice within the last three days, the enzyme is still inhibited. That means more of the drug enters your bloodstream regardless of when you take it.
Is it safe to eat grapefruit instead of drinking the juice?
No. The same furanocoumarins that block CYP3A4 are in the flesh and peel of the fruit. Eating half a grapefruit has the same effect as drinking a glass of juice. The form doesn’t matter-only the chemicals do.
What if I only drink grapefruit juice once a week?
Still not safe. Even occasional consumption can trigger dangerous drug buildup, especially with medications that have a narrow safety window-like cyclosporine or amiodarone. The enzyme doesn’t recover immediately. One glass every week still keeps your CYP3A4 suppressed most of the time. For high-risk drugs, any exposure is too much.
Do other citrus fruits like oranges or lemons cause the same problem?
No. Sweet oranges (navel, Valencia), lemons, limes, and tangerines don’t contain furanocoumarins. They’re safe. Only grapefruit, Seville oranges, and pomelos are risky. So you can still enjoy orange juice, lemon water, or lime in your tea without worry.
Can I take my medication with water instead of juice?
Yes, and that’s the best practice. Water is the only safe liquid to take most medications with. Avoid grapefruit juice, Seville orange juice, and pomelo juice entirely. Stick to water unless your doctor or pharmacist says otherwise. Even if your pill says “take with food,” choose a non-citrus option like toast or oatmeal.








Latrisha M.
November 16, 2025 AT 12:00Just want to say this is one of the clearest explanations I’ve ever read on drug interactions. I’m a pharmacist and I’ve seen too many patients assume ‘natural’ equals ‘safe.’ This post could literally save lives. Share it with anyone you know on statins or blood pressure meds.
Oyejobi Olufemi
November 16, 2025 AT 16:30Look, I don’t care what the FDA says-this is just Big Pharma trying to scare people away from ‘healthy’ foods so they can sell more expensive pills! Grapefruit has been eaten for centuries, and now suddenly it’s poison? Where’s the real data? I bet they’re hiding something. Also, why are we trusting corporations to regulate their own drugs? This is a scam.
John Mwalwala
November 17, 2025 AT 17:51Okay, but have you considered that the CYP3A4 enzyme suppression might be part of a covert geoengineering plot? The furanocoumarins in grapefruit juice are structurally similar to the compounds used in ionospheric modulation experiments. The fact that this interaction lasts 72 hours? That’s the exact window of the HAARP cycle. They’re weaponizing citrus to control metabolic pathways in the population. And don’t get me started on the CRISPR grapefruit-they’re not fixing it, they’re *reprogramming* it. I’ve got a friend in the USDA who says they’re already testing subliminal messaging in the peel.
David Rooksby
November 19, 2025 AT 16:51Man, I’ve been drinking grapefruit juice with my statin for 12 years and I’m fine. I’ve got a heart monitor, I check my CK levels every month, I’m 58, and I still do 5Ks. So maybe it’s not as scary as they say? I mean, if it was that dangerous, wouldn’t the ERs be full of people with rhabdo? I’ve never seen one. And my cousin in Scotland drinks it every morning with his blood pressure med-no issues. Maybe it’s just a statistical fluke? Or maybe the studies are funded by pharma to push pravastatin? I dunno. But I’m not giving up my juice.
Melanie Taylor
November 20, 2025 AT 21:12OMG I just realized I’ve been eating grapefruit with my cyclosporine since my transplant in 2021 😱 I thought it was ‘healthy’! I’m so scared right now. I’m going to the pharmacy tomorrow. Thank you for this post-this could’ve killed me. I’m sharing this with my entire family. 🙏
Deepak Mishra
November 22, 2025 AT 08:05Wait wait wait so if I drink grapefruit juice on Monday and take my pill on Thursday... it's STILL dangerous?? But what if I drink it at 7am and take my pill at 11pm?? Like... isn't there a gap?? And what if I only eat half?? And what if I drink it with milk?? Does milk neutralize it?? I'm so confused now I think I'm gonna have a panic attack 😭😭😭
Teresa Smith
November 23, 2025 AT 13:59This is exactly why we need better patient education. Not just in clinics, but in schools, grocery stores, pharmacies. People aren’t being negligent-they’re being misinformed by marketing, cultural habits, and outdated advice. I teach health literacy to seniors in my community, and this is one of the top three things we cover every month. Knowledge isn’t power-it’s survival. Thank you for making this accessible.
Daniel Stewart
November 24, 2025 AT 09:27It’s fascinating how we’ve built entire rituals around food-morning juice, Sunday oranges-and then science comes along and says, ‘Actually, this ritual is a slow poison.’ We cling to comfort, even when it’s dangerous. The grapefruit isn’t the villain. We are. We want our medicine to be simple, our fruit to be guilt-free, our bodies to be predictable. But biology doesn’t care about our preferences. It just works. And it doesn’t forgive.
ZAK SCHADER
November 25, 2025 AT 23:48Why is this even a thing? I mean, seriously? The FDA says avoid grapefruit juice but they don’t ban it? They don’t put warning labels on the fruit itself? That’s lazy. And why are we still using CYP3A4 as a metric? It’s outdated. We need AI-driven metabolic profiling for every patient. My cousin got his genome sequenced and they told him he’s a slow metabolizer-so why isn’t that standard? This whole system is broken. Also, I think this is why my dad’s kidneys failed. He never knew.
Diane Tomaszewski
November 27, 2025 AT 13:18I never knew this. I love grapefruit. I take blood pressure meds. I’m stopping. Simple. Thank you.
Dan Angles
November 29, 2025 AT 11:33As a clinical pharmacist with over two decades of experience, I can confirm the data presented here is both accurate and critically important. The pharmacokinetic interactions between furanocoumarins and CYP3A4 substrates are well-documented in peer-reviewed literature dating back to the 1990s. The persistence of this interaction for up to 72 hours is not anecdotal-it is reproducible in controlled studies. I routinely counsel patients on this issue, and I encourage all clinicians to include this in their standard intake protocols. Patient safety is not negotiable.
Ankit Right-hand for this but 2 qty HK 21
December 1, 2025 AT 09:57This is why America is weak. In India, we don’t need warnings-we know our bodies. My uncle takes simvastatin and drinks grapefruit juice every day-he’s 70 and still lifts weights. You people are too scared of everything. This is just another Western overreaction. If your body can’t handle a little fruit, maybe you shouldn’t be on drugs at all. Also, why are you trusting American science? They don’t even know how to make good coffee.