When your lower left abdomen suddenly feels like it’s being stabbed with a hot knife, and you can’t stand up straight, it’s not just gas. It could be diverticulitis-inflammation of small pouches in your colon that shouldn’t be there. These pouches, called diverticula, are common, especially as you get older. But when they get infected or inflamed, things turn serious fast. And the way we treat them today is nothing like it was ten years ago.
What Exactly Are Diverticula?
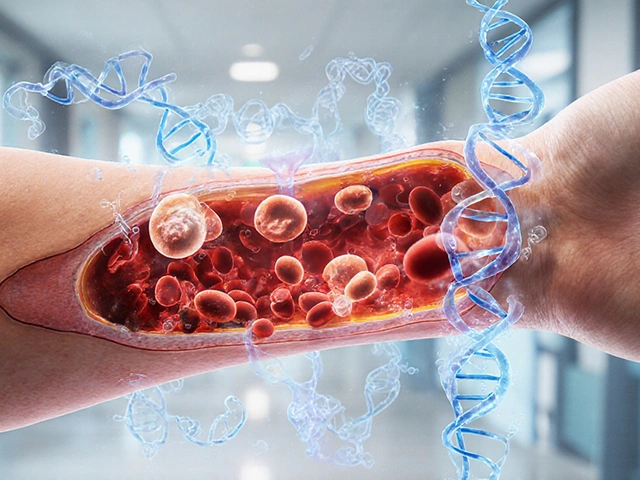
Diverticula are tiny bulges that push through weak spots in the wall of your colon. Think of them like little balloons sticking out from a stretched balloon. They’re not cancer. They’re not a disease by themselves. In fact, about 58% of people over 60 have them-this condition is called diverticulosis. Most never know they have them. They cause no symptoms. But when one of those pouches gets blocked by stool or bacteria, it can swell, get infected, and turn into diverticulitis.The sigmoid colon-your lower left colon-is where 95% of these pouches form. That’s why the pain is usually on the left side. But in people of Asian descent, it’s more common on the right side because of differences in colon structure. The pain isn’t just uncomfortable-it’s sharp, constant, and gets worse when you move. Fever above 38°C (100.4°F) often comes with it. That’s a red flag.
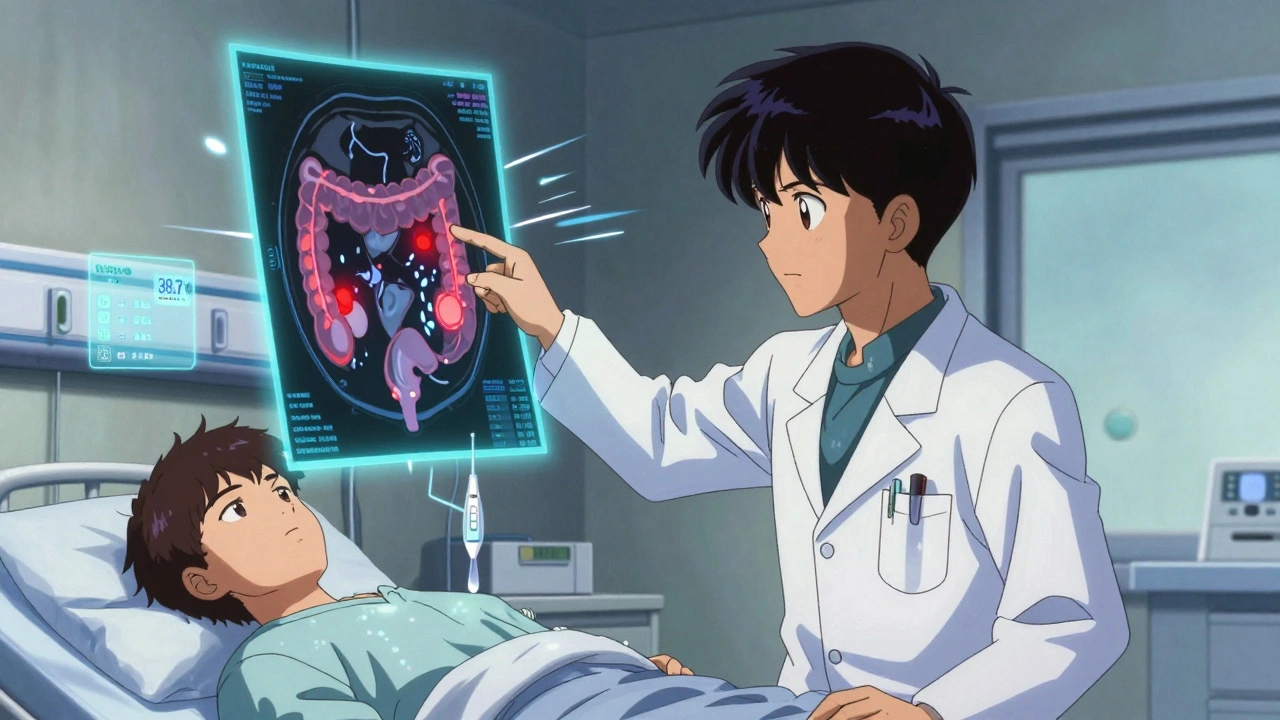
How Do Doctors Know It’s Diverticulitis?
It’s easy to mistake diverticulitis for something else. Irritable bowel syndrome (IBS) causes bloating and cramps too, but it doesn’t come with fever. Ovarian cysts in women can mimic the pain. Kidney stones can feel similar. That’s why misdiagnosis happens in about 25% of cases.Doctors look for three things: localized tenderness in the lower left abdomen, fever, and elevated white blood cell count (over 11,000 cells/µL). But the gold standard is a CT scan. It shows exactly where the inflammation is, how bad it is, and whether there’s an abscess or a hole. The Hinchey system grades it from I to IV:
- Stage Ia: Small pocket of infection around one pouch
- Stage Ib: Larger abscess, maybe over 3cm
- Stage II: Abscess in the pelvis
- Stage III: Infection spreading into the abdominal cavity
- Stage IV: A perforation-meaning the colon has burst, and poop is leaking into your belly
Stage IV is an emergency. You need surgery right away.
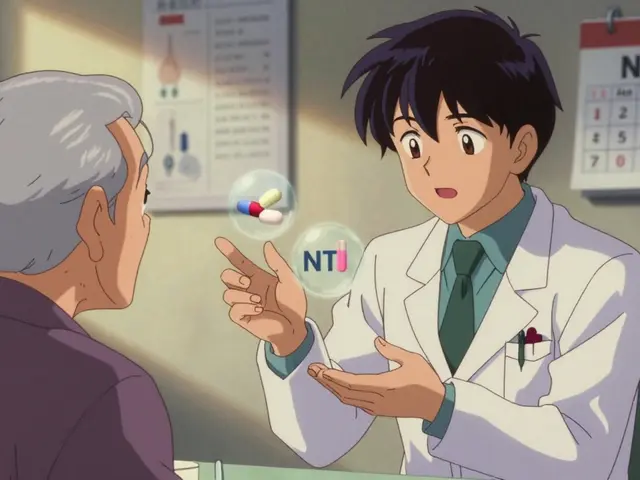
The Big Shift in Treatment: No More Antibiotics for Everyone
For decades, the rule was simple: diverticulitis = antibiotics. But that changed. In 2021, the DIVERT trial showed something shocking: for mild, uncomplicated cases, patients who didn’t take antibiotics recovered just as fast as those who did. The average recovery time? 7 days either way.Now, guidelines from the American Gastroenterological Association say: if you’re otherwise healthy, your fever is mild, and your blood tests aren’t wildly abnormal, you can skip antibiotics. Instead, focus on rest, fluids, and a clear liquid diet for 24 to 72 hours. Then slowly move to low-fiber foods like white rice, eggs, and cooked vegetables.
But here’s the catch: if you have a fever over 38.5°C, severe pain, or your white blood cell count is sky-high, antibiotics are still necessary. Common ones include amoxicillin-clavulanate (Augmentin) or ciprofloxacin with metronidazole. For hospital cases, doctors use IV antibiotics like piperacillin-tazobactam.
And avoid NSAIDs like ibuprofen or naproxen. They can increase the risk of a hole forming in your colon. Stick to acetaminophen (Tylenol) for pain.
When Surgery Becomes Necessary
Most people never need surgery. But if you’ve had multiple attacks-especially if you’ve been hospitalized for each one-your doctor might start talking about it. The old rule was three episodes. Now, it’s two, especially if your quality of life is suffering. Between attacks, you might feel fine, but you could be avoiding social events, skipping work, or living in fear of the next flare-up.For complicated cases (Stage III or IV), two main surgeries exist:
- Laparoscopic lavage: Drain the infection and clean out the belly without removing any colon. Works well in about 82% of cases when the rupture is contained.
- Resection: Remove the damaged part of the colon and reconnect the healthy ends. Sometimes you need a temporary colostomy bag while it heals.
A 2022 study (SCANDIV trial) found laparoscopic lavage had fewer complications than removal. But it’s not for everyone. If the infection is too widespread, removal is safer.
What Happens After the Attack?
Once the inflammation clears, you’ll need a colonoscopy. Not to check for cancer-but because diverticulitis can hide it. About 1.3% of people over 50 who’ve had diverticulitis turn out to have colon cancer. That’s why doctors recommend the test 6 to 8 weeks after you’ve recovered. It’s not routine for everyone, but for those over 50, it’s standard.And then comes the big question: how do you stop this from happening again?
Preventing Recurrence: Fiber, Not Fear
For years, doctors told people with diverticulitis to avoid nuts, seeds, popcorn, and corn. The idea was that these could get stuck in the pouches and cause inflammation. But that myth was busted in 2021 by an 18-year study of 47,000 women. Those who ate nuts and seeds regularly had lower rates of diverticulitis.The real enemy? Low fiber. A diet packed with white bread, processed snacks, and meat doesn’t move things through your colon. That leads to pressure, which creates more pouches-and makes existing ones more likely to inflame.
Target at least 30 grams of fiber a day. That’s:
- 1 cup cooked lentils (15g)
- 1 medium apple with skin (4g)
- 1 cup broccoli (5g)
- 1/2 cup oats (4g)
- 1 slice whole grain bread (2g)
Some people swear by fiber supplements like psyllium husk (Metamucil). One patient on a health forum said increasing fiber to 35g a day kept him attack-free for 27 months.
Other proven protectors: regular exercise (at least 2 hours a week), quitting smoking (smokers have nearly 3x the risk), and maintaining a healthy weight. Obesity increases your risk more than double.
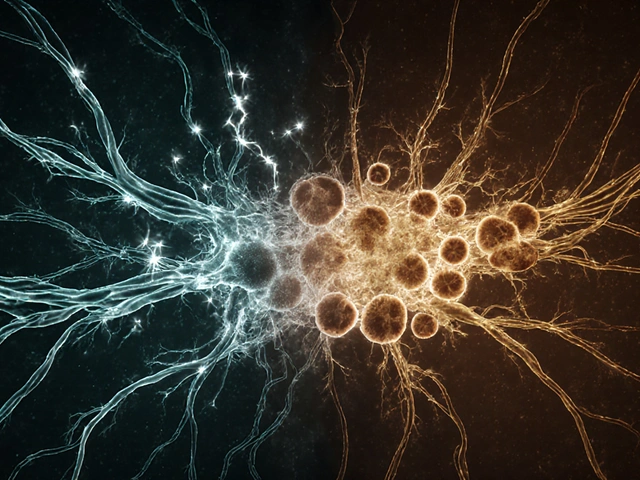
New Frontiers: Drugs and AI
In 2023, the FDA approved mesalazine (Pentasa) for long-term use after diverticulitis. In a trial, it cut recurrence rates by 31% over a year compared to placebo. It’s not a cure, but for people who’ve had multiple attacks, it’s a tool.And then there’s AI. Mayo Clinic developed a tool that looks at your CT scan, blood results, age, and BMI-and predicts your chance of another attack with 83% accuracy. That helps doctors decide who needs surgery, who needs a drug, and who just needs to eat more broccoli.
Researchers are also studying the gut microbiome. People who’ve had diverticulitis often have lower levels of Faecalibacterium prausnitzii-a good bacteria that helps calm inflammation. Future treatments might involve targeted probiotics or fecal transplants.
Why This Matters Now More Than Ever
Diverticulitis isn’t just an older person’s problem anymore. In 2023, people under 44 made up 22% of hospitalizations-up from 14% in 2000. Why? Probably because of diets low in fiber, more sedentary lifestyles, and rising obesity rates.It’s also expensive. In the U.S., diverticulitis causes 200,000 hospital stays a year and costs $2.3 billion. Misdiagnosis adds another $3,500 to $5,200 per case. That’s why knowing the signs matters-not just for you, but for the whole system.
Most people recover fully. But the key is acting fast, avoiding outdated myths, and focusing on what really works: fiber, movement, and listening to your body.
Can diverticulitis go away on its own?
Yes, in mild, uncomplicated cases, diverticulitis can resolve without antibiotics or surgery. With rest, fluids, and a clear liquid diet followed by a gradual return to low-fiber foods, many people recover within a week. However, if you have a fever above 38.5°C, severe pain, or signs of infection like vomiting or rapid heartbeat, you need medical attention immediately.
Do I need to avoid nuts and seeds if I’ve had diverticulitis?
No. That advice is outdated. A major 18-year study tracking 47,000 women found no link between eating nuts, seeds, popcorn, or corn and increased diverticulitis risk. In fact, those who ate these foods regularly had lower rates of flare-ups. These foods are high in fiber and can be part of a healthy, preventive diet.
How long should I wait before returning to a normal diet after an attack?
Start with clear liquids for 48 to 72 hours. Then slowly add low-fiber foods like eggs, white rice, and cooked chicken. Once symptoms fully disappear, gradually reintroduce high-fiber foods over the next week. Don’t rush it-jumping back to a high-fiber diet too fast can cause bloating or cramps. Listen to your body.
Is diverticulitis the same as IBS?
No. Irritable bowel syndrome (IBS) causes crampy, shifting pain, bloating, and changes in bowel habits-but no fever, no infection, and no structural damage. Diverticulitis is an infection or inflammation of pouches in the colon. It often comes with localized, constant pain (usually on the left), fever, and elevated white blood cells. The treatments are completely different.
When should I consider surgery for diverticulitis?
Surgery is no longer automatic after three attacks. Current guidelines suggest considering it after two hospitalizations for diverticulitis, especially if you’re experiencing ongoing pain, missed work, or reduced quality of life between episodes. Surgery may also be needed immediately if you develop a perforation, abscess that won’t drain, or signs of widespread infection.
Can stress cause diverticulitis?
Stress doesn’t directly cause diverticulitis, but it can worsen symptoms and slow recovery. High stress levels can affect gut motility and immune function, making it harder for your body to fight off inflammation. Managing stress through sleep, exercise, or mindfulness can support overall gut health, especially during recovery.
Are there any new medications for preventing diverticulitis recurrence?
Yes. In 2023, mesalazine (Pentasa) received FDA approval for maintenance therapy after an attack. In clinical trials, it reduced recurrence rates by 31% over 12 months compared to placebo. It’s not a cure, but for people with multiple episodes, it’s an option to consider alongside dietary changes. Always discuss it with your gastroenterologist.


Laura Saye
December 6, 2025 AT 03:58It’s fascinating how medicine keeps evolving-antibiotics for everything used to be gospel, and now we’re learning that sometimes the body just needs space to heal itself. I’ve seen friends go through diverticulitis attacks and the relief when they stopped the meds and focused on rest was almost spiritual. Like, your body isn’t your enemy-it’s trying to communicate. Listening matters more than intervening.
Krishan Patel
December 6, 2025 AT 07:39Anyone who skips antibiotics for diverticulitis is playing Russian roulette with their colon. This isn’t yoga retreat medicine-it’s a life-threatening infection. The DIVERT trial had selection bias. People who didn’t need antibiotics were already low-risk. The moment you have fever and leukocytosis, you’re in the danger zone. Don’t let trendy pseudoscience get you hospitalized.
Carole Nkosi
December 6, 2025 AT 12:11You think this is new? In South Africa, we’ve been telling people for decades that fiber is the real medicine-not pills, not surgery. The colonial mindset of ‘fix it with drugs’ is why so many Westerners are sick. Eat lentils, walk daily, stop eating processed garbage. Your colon doesn’t need a PhD to function. It needs whole food.
Jimmy Jude
December 8, 2025 AT 04:00Okay but have you ever had a diverticulitis attack at 3 a.m. while your partner is snoring and you’re curled up like a shrimp trying not to scream? I have. And let me tell you-no amount of ‘fiber is your friend’ makes that pain go away. The real villain? Modern life. Sitting. Stress. Sugar. And doctors who won’t listen. I’m not mad-I’m just… deeply disappointed in everything.
Mark Ziegenbein
December 10, 2025 AT 00:28The real tragedy here isn’t the misdiagnosis or the outdated advice-it’s that we’ve allowed the medical industrial complex to profit off fear. Antibiotics are a $12 billion industry. Colonoscopies? Billions. Laparoscopic lavage? Premium pricing. Meanwhile the cheapest, most effective intervention-eating vegetables-is treated like a fringe lifestyle choice. We’ve turned prevention into a commodity. And the people who suffer? They’re just collateral damage in the profit calculus.
Juliet Morgan
December 11, 2025 AT 16:50Just had my second flare-up last month and I’m telling you-fiber changed everything. I started with Metamucil and slowly added beans, oats, apples. No nuts at first, then tried them. No issues. I’m 41 and I’ve been attack-free for 10 months. You don’t need to be perfect. Just consistent. And if you’re scared to start? Do it slowly. One extra veggie a day. You got this.
Norene Fulwiler
December 12, 2025 AT 20:27As someone raised in a family that ate beans and greens every day, I’m not surprised the data shows fiber prevents this. But I’m angry that this info wasn’t mainstream. In my community, we didn’t call it diverticulitis-we called it ‘that thing that happens when you eat too much white bread.’ We didn’t need a CT scan to know what was wrong. We just knew food mattered.
Katie Allan
December 13, 2025 AT 09:25What’s striking is how much of this mirrors other chronic conditions-IBS, Crohn’s, even diabetes. We focus on treating symptoms rather than root causes. Diet, movement, sleep-they’re not ‘alternative.’ They’re the foundation. And yet, we treat them like optional add-ons. Maybe the real breakthrough isn’t a new drug, but a cultural shift in how we value daily habits.
Kylee Gregory
December 13, 2025 AT 10:39I think the most important thing here is that people aren’t being scared into compliance-they’re being empowered with knowledge. That’s huge. For years, we told people to avoid seeds and nuts out of fear. Now we know those were myths. That’s not just medical progress-it’s ethical progress. We’re learning to trust the body more and the fear less.
Lucy Kavanagh
December 14, 2025 AT 22:24Did you know the FDA approved mesalazine right after Big Pharma funded the trial? And AI predicting recurrence? That’s just a way to sell more scans and subscriptions. They don’t want you to heal-they want you to monitor. Fiber? Free. Colonoscopy? $3,000. Think about it.
Stephanie Fiero
December 15, 2025 AT 02:07OMG I JUST HAD A FLARE UP LAST WEEK AND I DIDNT KNOW WHAT WAS HAPPENING UNTIL I WENT TO ER AND THEY SAID DIVERTICULITIS I THOUGHT IT WAS JUST BAD GAS LIKE EVERYONE ELSE LOL THANKS FOR THE INFO I’M GONNA START EATING MORE BROCCOLI NOW
aditya dixit
December 15, 2025 AT 03:21In India, we’ve always eaten dal, roti, and vegetables daily. No one here gets diverticulitis like Americans do. It’s not genetics-it’s diet. My uncle had it once, after he started eating pizza and soda. He went back to his old food and never had another episode. Sometimes the answer is simpler than we want it to be.