Hypoglycemia Risk Calculator
Assess Your Hypoglycemia Risk
This tool estimates your personal risk of hypoglycemia based on factors discussed in the article. Results show your risk level and tailored prevention tips.
Insulin therapy saves lives. For people with type 1 diabetes, it’s not optional-it’s survival. For many with advanced type 2 diabetes, it’s the only way to keep blood sugar from spiraling out of control. But for every person who gains control over their diabetes with insulin, another battles two stubborn side effects: hypoglycemia and weight gain. These aren’t rare or minor issues. They’re the biggest reasons people skip doses, avoid tight control, or even stop insulin altogether.
What Hypoglycemia Really Feels Like
Hypoglycemia means your blood sugar drops below 70 mg/dL. It’s not just feeling a little shaky. It’s your body screaming for help. You might get dizzy, break out in a cold sweat, or feel your heart race. Your hands might tremble. Your vision blurs. You can’t think straight. In severe cases, you pass out. If no one helps you, it can lead to seizures or even brain damage. This isn’t theoretical. In the landmark DCCT study, people with type 1 diabetes on intensive insulin therapy had three times more severe low blood sugar episodes than those on standard treatment. About 6% of them had at least one life-threatening low per year. That’s one in every 17 people. And it’s not just type 1. People with type 2 on insulin face the same risk-especially if they’re older, have kidney problems, or don’t eat regularly. The worst part? Some people lose their warning signs. This is called hypoglycemia unawareness. After 15 to 20 years of diabetes, about one in four people on insulin no longer feel the early symptoms. They go from fine to unconscious without noticing anything’s wrong. That’s why wearing a medical ID bracelet isn’t just a good idea-it’s essential.Why Insulin Makes You Gain Weight
Insulin doesn’t just move sugar into your cells. It tells your body to store fat. When you start insulin, your body finally gets the signal it’s been missing: “You can use glucose now.” Before insulin, your body was burning muscle and fat for energy because it couldn’t use sugar. That’s why many people with undiagnosed diabetes lose weight-despite eating a lot. Once insulin kicks in, glucose stops being flushed out in urine. Instead, it’s absorbed. And excess glucose? It gets turned into fat. On average, people gain 4 to 6 kilograms (9 to 13 pounds) in the first year of insulin therapy. Some gain more. Some less. It depends on how much you eat, how active you are, and how much insulin you need. But here’s the catch: many people fear weight gain so much they underdose their insulin. They keep their blood sugar high to avoid gaining pounds. That’s dangerous. High blood sugar damages nerves, kidneys, eyes, and blood vessels. It increases heart attack and stroke risk. So you’re trading one problem for a worse one.How to Prevent Low Blood Sugar
You don’t have to live in fear of hypoglycemia. There are proven ways to reduce the risk.- Check your blood sugar often. At least four to six times a day if you’re on multiple daily injections or an insulin pump. Don’t skip meals or snacks just because you’re busy.
- Use continuous glucose monitoring (CGM). CGM devices track your sugar levels 24/7 and alert you when you’re dropping too fast. Studies show they cut hypoglycemia events by 40 to 50%.
- Know your correction factors. How much does one unit of insulin lower your blood sugar? That number varies. Work with your doctor to find yours. Don’t guess.
- Carry fast-acting sugar. Glucose tablets, juice, or candy. Keep them everywhere-your car, purse, desk, bedside. If you feel a low coming on, treat it immediately. Don’t wait.
- Teach someone how to give glucagon. Glucagon is a hormone that raises blood sugar fast. It comes in an injection or nasal spray. If you pass out, someone needs to be able to use it. Make sure your family, coworkers, or friends know where it is and how to use it.
How to Avoid Weight Gain on Insulin
Weight gain isn’t inevitable. It’s manageable.- Start with nutrition counseling. A dietitian who specializes in diabetes can help you adjust your meals to match your insulin. Portion control matters more than ever now that your body is using sugar efficiently.
- Don’t overcorrect lows. If your blood sugar is 60 mg/dL, you don’t need 4 glucose tablets. One or two are enough. Too much sugar leads to rebound highs-and then more insulin, which leads to more fat storage.
- Move more. Exercise makes your body use insulin better. You need less of it. That means less fat storage. Aim for 150 minutes a week of walking, swimming, or cycling.
- Ask about combination therapy. GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) or liraglutide (Victoza) are now often used with insulin. These drugs slow digestion, reduce appetite, and help you lose weight. In clinical trials, people on insulin plus semaglutide lost 5 to 10 kilograms over 30 weeks-while improving blood sugar control.
- Use newer insulins. Long-acting insulins like insulin degludec (Tresiba) and insulin glargine (Lantus) cause fewer lows than older types like NPH. Tresiba reduces nighttime lows by 40% compared to older insulins.
When to Talk to Your Doctor
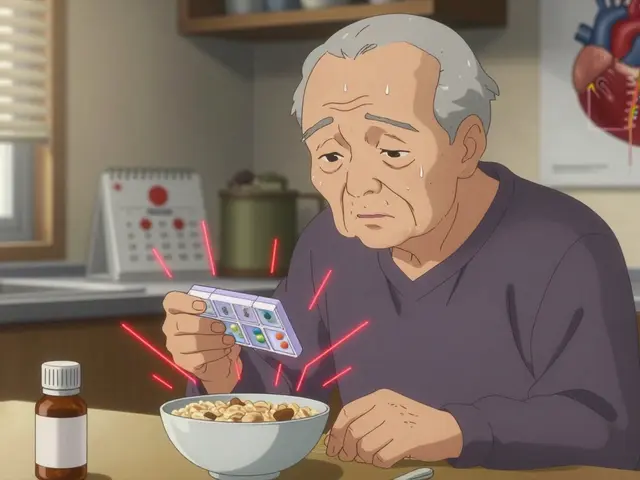
If you’re having frequent lows-even mild ones-or gaining weight faster than you expected, don’t wait. Your insulin plan can be adjusted. Your dose can be lowered. Your timing can be changed. You might need a different type of insulin. Or you might benefit from adding a non-insulin medication that helps with weight and lowers blood sugar. The goal isn’t perfection. It’s safety. It’s balance. You don’t need to hit an A1c of 6.5% if it means you’re passing out once a month. The American Diabetes Association now recommends individualized goals. For someone at high risk of lows, an A1c of 7.5% to 8% might be the right target. That’s not failure. That’s smart management.
The Bigger Picture
Insulin is powerful. It’s life-saving. But it’s not simple. It requires constant attention. It demands you learn your body’s signals. It asks you to eat when you’re not hungry, check your sugar when you’re tired, and carry emergency supplies even when you feel fine. But here’s the truth: the risks of not using insulin are far worse. Uncontrolled diabetes leads to amputations, kidney failure, blindness, and early death. Hypoglycemia and weight gain are challenges-but they’re manageable challenges. Technology is helping. New insulins, CGMs, and closed-loop systems (artificial pancreas) are cutting hypoglycemia rates in half. Combination therapies are turning weight gain into weight loss. Education programs that teach carb counting and insulin dosing reduce severe lows by up to 50%. You’re not alone. Millions of people manage insulin every day. They live full lives. They travel. They work. They raise families. They don’t let fear stop them. They learn. They adapt. They get help. Your job isn’t to be perfect. It’s to stay safe. To stay informed. To speak up when something doesn’t feel right.Frequently Asked Questions
Can insulin cause seizures?
Yes. Severe hypoglycemia from insulin can lead to seizures if blood sugar drops too low and isn’t treated quickly. This happens when the brain doesn’t get enough glucose to function. Seizures are a medical emergency. If someone has a seizure from low blood sugar, call 999 immediately and give glucagon if available.
Why do I gain weight even if I eat the same as before?
Before insulin, your body couldn’t use glucose properly, so excess sugar was lost in urine. Once you start insulin, your body begins absorbing and storing that glucose instead. Any extra calories-whether from carbs, fat, or protein-are more likely to be stored as fat. That’s why weight gain happens even without eating more.
Is it safe to skip insulin doses to avoid weight gain?
No. Skipping insulin leads to high blood sugar, which damages organs over time. It increases your risk of heart disease, kidney failure, nerve damage, and blindness. Weight gain is a side effect-but uncontrolled diabetes is life-threatening. Talk to your doctor about safer ways to manage weight, like adjusting your diet or adding GLP-1 medications.
Do all types of insulin cause the same amount of weight gain?
No. Older insulins like NPH cause more weight gain and more lows than newer analogs. Long-acting insulins like insulin glargine (Lantus) and insulin degludec (Tresiba) are designed to work more steadily, reducing both hypoglycemia and weight gain. Tresiba, in particular, has been shown to reduce nighttime lows by 40% compared to older insulins.
Can continuous glucose monitors (CGMs) help with both hypoglycemia and weight gain?
Yes. CGMs show you how your body reacts to food, activity, and insulin in real time. You can see which meals spike your sugar and which ones cause lows. This helps you adjust portions and timing to avoid overtreating lows-which reduces unnecessary calorie intake. Many people using CGMs lose weight because they eat more intentionally.
How long does insulin-related weight gain last?
Most weight gain happens in the first 6 to 12 months after starting insulin. After that, it usually slows down. But if you keep eating more than your body needs, you’ll keep gaining. The key is matching your food intake to your insulin dose and activity level. With the right diet and exercise, weight can stabilize or even go down.
Are there any new medications that help with insulin side effects?
Yes. GLP-1 receptor agonists like semaglutide and liraglutide are now commonly added to insulin regimens. They reduce appetite, slow digestion, and help you lose weight-while also improving blood sugar control. In trials, patients on insulin plus semaglutide lost 5 to 10 kg over 6 to 8 months. These drugs are changing how insulin is used today.




Colin Pierce
January 28, 2026 AT 16:25Been on insulin for 12 years. The weight gain was brutal at first - I picked up 18 lbs in 6 months. But once I started working with a diabetes dietitian and switched to Tresiba, it got way more manageable. Also, CGM was a game-changer. I stopped overtreating lows because I could see the trend before it crashed. No more 4 glucose tabs for a 65 reading - just one. Life’s easier now.
And yeah, hypoglycemia unawareness? Scary as hell. I passed out once in the grocery store. Now I wear a medical ID and my wife knows where the glucagon is. Don’t wait till it’s too late.
Phil Davis
January 29, 2026 AT 18:02So insulin makes you fat. Who knew? Next you’ll tell me breathing oxygen causes weight gain. Jeez.
Just kidding. But seriously, if you’re shocked that a hormone that stores glucose = stores fat, maybe don’t start with the ‘I didn’t know’ face. We’ve known this since the 1920s.
Irebami Soyinka
January 30, 2026 AT 22:48USA always making everything about insulin like it’s some magical cure-all. In Nigeria, we don’t even have access to CGMs or Tresiba. We use NPH and pray. And yes, we gain weight. And yes, we get lows. But we still live. We still feed our kids. You guys complain about 6 lbs - we fight for a vial of insulin that doesn’t expire in the heat.
Stop acting like this is a first-world problem. It’s a global crisis. 🙏😭
doug b
February 1, 2026 AT 11:35Look. Insulin isn’t the enemy. Fear is. If you skip doses to avoid weight gain, you’re trading a slow death for a fast one. I’ve seen it. Kidneys failing. Nerves dead. Toes gone. All because someone didn’t want to gain 10 pounds.
Start walking. Eat clean. Use your CGM. Talk to your doc about Ozempic. You can do this. You’re not broken. You’re just learning.
Mel MJPS
February 2, 2026 AT 00:58I love how you included the FAOs - they’re so helpful. I had no idea CGMs could help with weight too. I thought they were just for lows. Now I’m looking at my trends and realizing I was eating way too many carbs after every ‘low’ that wasn’t even a real low. Mind blown. Thank you for this.
Katie Mccreary
February 2, 2026 AT 07:42You say ‘don’t skip insulin’ like it’s that simple. Have you ever tried to explain to your partner why you can’t eat dessert because your insulin dose is already maxed out? Or why you cry when you gain 2 lbs? Or why your mom thinks you’re lazy because you ‘just need to stop eating’? This isn’t just medical. It’s emotional. And you’re not addressing that.
Also, who even uses glucagon anymore? It’s a nightmare to inject. And nasal spray? Still feels like a science experiment.
SRI GUNTORO
February 3, 2026 AT 00:09Why do people still use insulin at all? In India, we’ve been using Ayurveda and fasting for centuries. No chemicals. No weight gain. No hypoglycemia. You Americans are so dependent on pills and machines. It’s pathetic. You think science fixes everything. But nature knows better.
Go drink bitter gourd juice. Go walk barefoot on grass. Stop poisoning your body with insulin.
Jess Bevis
February 4, 2026 AT 03:07Just moved from the US to Japan. Here, they use insulin differently - smaller doses, more frequent checks, way less carb-heavy meals. No one gains 10 lbs on insulin here. Why? Culture. Food. Mindset. Not magic.
It’s not the insulin. It’s the plate.
Rose Palmer
February 4, 2026 AT 16:44Thank you for this comprehensive and clinically accurate overview. The integration of evidence-based strategies - including the use of newer insulin analogs and GLP-1 receptor agonists - represents a significant advancement in personalized diabetes management. It is imperative that healthcare providers communicate these options with clarity and compassion, ensuring patients understand that therapeutic goals are individualized and that safety supersedes arbitrary glycemic targets. This post exemplifies best-practice patient education.
Kathy Scaman
February 6, 2026 AT 13:12My dad started insulin last year. He gained 15 lbs, got scared, stopped taking it for two weeks. Ended up in the ER. Now he uses Tresiba, checks his sugar with his phone, and walks after dinner. He’s down 8 lbs. Still has lows sometimes. But he’s alive. And he’s not afraid anymore.
Just saying - it gets better.