Peripheral neuropathy isn't a single disease-it's a group of conditions caused by damage to the nerves outside your brain and spinal cord. These nerves control everything from how your toes feel when you walk to how your heart beats. When they get damaged, you might feel burning, tingling, or numbness, usually starting in your feet or hands. For many, it’s not just discomfort-it’s life-changing. About 20 million Americans live with it, and diabetes is behind half of those cases. But it’s not just diabetes. Vitamin B12 deficiency, chemotherapy, alcohol use, and even unknown causes can trigger it. The good news? There are real ways to manage the pain and stop it from getting worse-if you know where to start.
What Actually Causes Nerve Damage?
Not all peripheral neuropathy is the same. The cause determines how you treat it. The most common culprit? High blood sugar. If you have diabetes and your HbA1c stays above 7%, your nerves slowly get damaged over time. The Diabetes Control and Complications Trial showed that keeping blood sugar under control cuts neuropathy progression by 60%. That’s not a small win-it’s the single most effective thing you can do.
Then there’s chemotherapy. About one in three cancer patients on drugs like vincristine or paclitaxel develop neuropathy. It’s often called "chemo brain" but it’s really chemo nerves-tingling fingers, trouble holding a cup, walking like you’re on ice. Sometimes it gets better after treatment ends. Sometimes it doesn’t. That’s why doctors now monitor nerve function during chemo, not just tumor size.
Vitamin B12 deficiency is another sneaky cause. It’s easy to miss because symptoms overlap with aging: fatigue, balance issues, numbness. But fixing it is simple: a monthly B12 shot or high-dose oral supplement can reverse symptoms in 4 to 8 weeks. The NHS estimates it’s behind about 8% of cases. If you’re over 60, vegetarian, or on metformin for diabetes, get your B12 checked.
Then there’s alcohol. Long-term heavy drinking damages nerves directly and also causes nutritional deficiencies. Cutting back or quitting can stop the damage-and sometimes even help nerves heal. Infections like Lyme disease or HIV, autoimmune disorders like Guillain-Barré, and even genetics (like Charcot-Marie-Tooth disease) can also be to blame.
And then there’s the 20% of cases where doctors can’t find a cause. These are called "idiopathic neuropathy." It’s frustrating, but not hopeless. Even without a clear trigger, pain can still be managed.
How Do You Know It’s Neuropathy?
It’s not just "my feet hurt." Neuropathy has a signature pattern. Symptoms usually start in your toes or fingertips and creep upward over months or years. You might feel like you’re walking on pebbles, or that your socks are bunched up-even when they’re not. Burning pain at night is common. Many people say they can’t stand the feel of bedsheets on their feet.
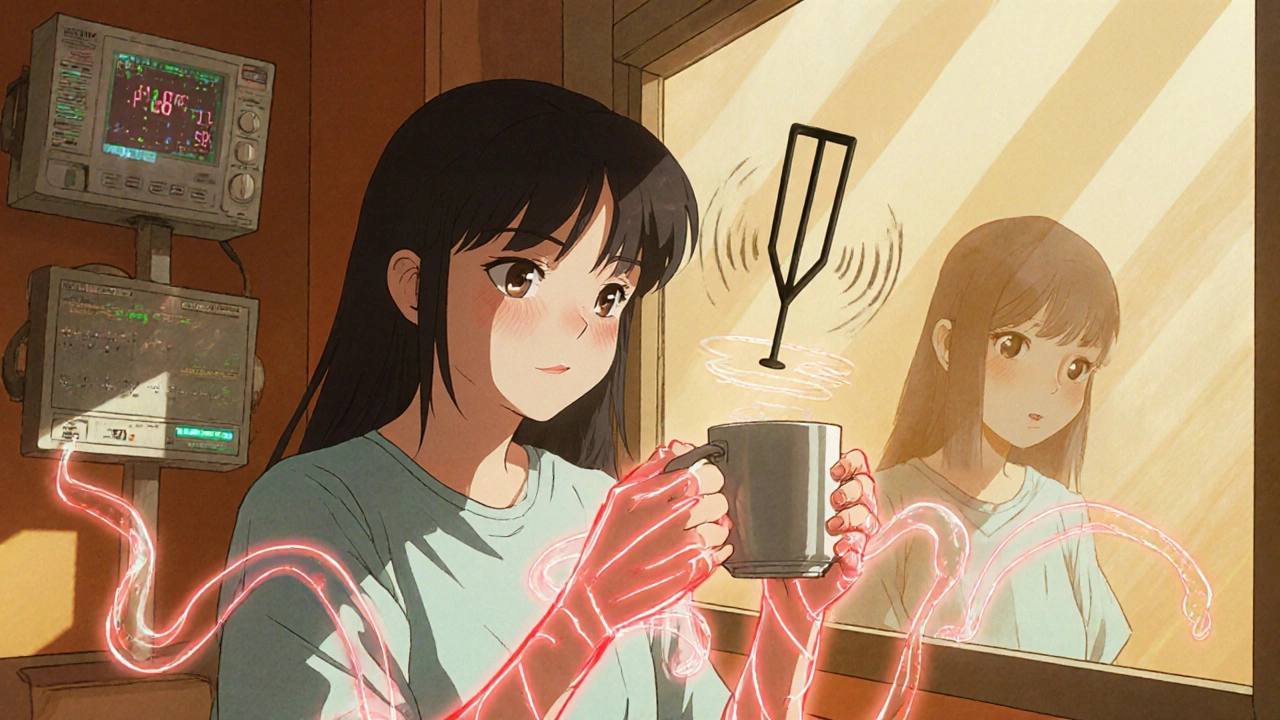
Doctors use simple tests to confirm it. A 10-gram monofilament pressed against your foot checks if you can feel light touch. A 128-Hz tuning fork on your big toe tests vibration sense. If you can’t feel either, your nerves are impaired. Nerve conduction studies measure how fast signals travel through your nerves-normal is above 50 m/s; below 40 means damage.
There are also scoring tools like the Michigan Neuropathy Screening Instrument (MNSI). A score above 8 means severe damage. These aren’t just for diagnosis-they help track if treatment is working.
What Actually Works for Pain?
Pain relief isn’t one-size-fits-all. Over-the-counter painkillers like ibuprofen or acetaminophen? They barely help. Neuropathic pain doesn’t respond to regular inflammation blockers. You need targeted meds.
Pregabalin (Lyrica) is a first-line treatment. Studies show it reduces pain by 50% in about 37% of people taking 150-600 mg daily. But it comes with side effects: dizziness, weight gain, swelling. One Reddit user said it cut her pain from 8/10 to 3/10-but made her too dizzy to drive for two weeks.
Duloxetine (Cymbalta) is another top choice. It’s an antidepressant that also blocks pain signals. About 35% of users get 50% pain relief. But nausea hits hard for some-42% quit within a month because of it.
Amitriptyline, an older tricyclic antidepressant, works for 41% of people. It’s cheap, but the side effects are rough: dry mouth (75%), drowsiness (60%), blurry vision. Many older adults can’t tolerate it.
There’s also Qutenza-a patch with high-dose capsaicin. Applied once every 3 months in a doctor’s office, it burns off pain-sensing nerves temporarily. Clinical trials show 31% pain reduction after 12 weeks. It’s not for everyone, but for those who’ve tried everything else, it’s a game-changer.
And then there’s scrambler therapy. It uses electrical signals to "trick" your brain into not feeling pain. Mayo Clinic data shows 85% of patients got 50% pain relief after just 10 sessions. It’s expensive-$1,200 to $1,500 per session-but if insurance covers it, it’s worth considering.
Non-Medication Ways to Feel Better
Medications help, but they’re not the whole story. Physical therapy is one of the most underrated tools. A 12-week program of balance training and strength exercises improves your "up and go" time by 25%. That means fewer falls, more confidence walking. The NHS reports 78% of patients say physical therapy helped them significantly.
Custom orthotics? Huge. People with neuropathy often lose sensation in their feet, so they don’t feel blisters or pressure points. Therapeutic shoes with cushioned insoles reduce foot ulcers by 50%. One patient said, "I didn’t realize how much pain I was in until I wore the right shoes. It was like a new life."
Scrambler therapy and spinal cord stimulation are high-tech options, but low-tech habits matter too. Daily foot inspections-looking for cuts, redness, swelling-are non-negotiable. The American Diabetes Association recommends checking your feet twice a day. If you can’t see your soles, use a mirror. If you have trouble bending, ask a family member to help.
Light exercise like walking, swimming, or tai chi improves circulation and nerve function. Even 20 minutes a day makes a difference. Sleep matters too. Neuropathy pain keeps 75% of patients awake. Try cooling your feet before bed, avoiding caffeine after 2 p.m., and using a pillow between your legs to reduce pressure.
What Doesn’t Work (And Why)
Opioids are a trap. Studies show they only reduce neuropathic pain by 30%-and addiction rates jump to over 15% with long-term use. The American Diabetes Association and Harvard Medical School both warn against them. They don’t fix the nerve damage. They just mask the pain, often making things worse.
Supplements like alpha-lipoic acid or acetyl-L-carnitine sound promising, but the evidence is weak. Some small studies show mild benefit, but nothing consistent enough to recommend as standard care. Don’t waste money unless your doctor says it’s safe to try.
And don’t wait. The longer you wait to treat it, the harder it is to reverse. Dr. P. James B. Dyck from Mayo Clinic says early treatment-within six months of symptoms-boosts response rates by 40%. If you’ve had numbness for two years, your nerves may be too damaged to fully recover. But you can still stop it from getting worse.

What’s Next? New Treatments on the Horizon
Research is moving fast. The FDA approved Qutenza in 2020, but newer therapies are coming. Gene therapy for inherited neuropathies like Charcot-Marie-Tooth is in early trials. One study showed a 20% improvement in nerve signal speed after six months.
The Foundation for Peripheral Neuropathy launched the Neuropathy Genomics Project in 2023. By 2026, they hope to identify genetic markers for over 50 types of neuropathy. That could lead to personalized treatments.
Wearable nerve stimulators are in development. Early models promise 40% pain reduction with daily use. They’re expected to hit the market in 2025. AI tools are also being trained to spot early nerve damage from foot scans or gait patterns-potentially cutting diagnosis time from 18 months to just 6.
For now, the best strategy is simple: treat the cause, manage the pain, protect your nerves. If you have diabetes, get your HbA1c below 7%. If you’re on chemo, ask about nerve monitoring. If your feet feel numb, don’t ignore it. See a neurologist. Get tested. Start moving. Your nerves can’t heal if they’re still under attack.
Can peripheral neuropathy be reversed?
It depends on the cause and how early you act. If it’s from vitamin B12 deficiency, correcting the deficiency can fully reverse symptoms in weeks. If it’s from uncontrolled diabetes, you can stop it from getting worse-but existing damage may not fully heal. In cases of chemotherapy or idiopathic neuropathy, nerves may partially recover over time, but full reversal is rare. The key is early intervention: within the first six months, treatment response improves by 40%.
Is neuropathy pain always in the feet?
No, but it usually starts there. Peripheral nerves in the feet are the longest in the body, so they’re the first to show damage. Many people feel tingling or burning in their toes first. But neuropathy can also affect hands, arms, legs, and even internal organs. If your digestive system is involved, you might have nausea, constipation, or trouble swallowing. Heart rate and blood pressure can also be affected. Symptoms vary by which nerves are damaged.
How long does it take for neuropathy treatments to work?
It varies. For B12 deficiency, you might feel better in 4 to 8 weeks. For diabetes, lowering your HbA1c below 7% can stabilize symptoms in 3 to 6 months. Medications like pregabalin or duloxetine often take 2 to 4 weeks to build up in your system. Physical therapy shows results after 8 to 12 weeks. Scrambler therapy requires 10 sessions over 2 to 3 weeks. Patience is key-but don’t wait too long. Delaying treatment reduces your chances of improvement.
Can I still drive with neuropathy?
It depends. If you have numbness in your feet, you might not feel the gas or brake pedal properly. Dizziness from medications like pregabalin can also make driving unsafe. Many patients report losing confidence behind the wheel. If you’re unsure, ask your doctor for a driving assessment. Some states require medical clearance for drivers with neurological conditions. Always prioritize safety over convenience.
Are there any natural remedies that help?
There’s no magic cure, but some lifestyle changes help. Regular low-impact exercise improves circulation. Avoiding alcohol protects your nerves. Eating a balanced diet rich in B vitamins supports nerve health. Some people find relief with acupuncture or massage, though evidence is limited. Topical creams with lidocaine or capsaicin can ease localized pain. But don’t rely on supplements like turmeric or omega-3s-they haven’t been proven to reverse nerve damage.
What should I do if my current treatment isn’t working?
Talk to your doctor about switching or combining therapies. If one medication causes side effects, try another. If pain persists, ask about scrambler therapy or spinal cord stimulation. Consider a referral to a neuropathy specialist or pain clinic. Also, make sure your underlying cause is fully addressed-like checking your HbA1c, B12 levels, or thyroid function. Sometimes, the problem isn’t the treatment-it’s the diagnosis.
What to Do Next
If you’re experiencing symptoms, don’t wait. Start with your primary care doctor. Ask for a nerve conduction test or a simple monofilament check. If you have diabetes, get your HbA1c tested if you haven’t in the last 3 months. If it’s above 7%, work with your doctor to bring it down.
Start daily foot checks. Buy a mirror if you can’t see your soles. Wear supportive shoes-even around the house. Cut back on alcohol. Eat more leafy greens, eggs, and fish for B vitamins. Move your body every day.
If you’re already diagnosed, don’t give up. Many people find relief with the right mix of treatments. It might take trying a few options. Keep track of what helps and what doesn’t. Bring that list to your next appointment. You’re not alone-millions are managing this, and new tools are coming every year.






Josh Gonzales
November 26, 2025 AT 02:15Been living with this for 8 years since my chemo ended. Lyrica helped at first but now I need higher doses just to feel numb. The real game-changer? Custom orthotics. I didn't think shoes could make that difference until I stopped feeling like I was walking on broken glass. Also, foot checks twice a day. Non-negotiable. If you're not doing this, you're playing Russian roulette with ulcers.
Valérie Siébert
November 27, 2025 AT 21:39OMG YES TO THE SHOES!!! I was skeptical too but got these therapeutic ones from my PT and now I can actually walk to the mailbox without crying. Also started walking 20 mins after dinner and my night pain dropped like a rock. No magic pills, just dumb consistent stuff. Also stop drinking. Like, just stop. Your nerves aren't a bar napkin.
Ellen Sales
November 29, 2025 AT 04:11I know this feels hopeless but you're not broken-you're just damaged, and damage can be managed. I was told at 52 that I’d be in a wheelchair by 60. I’m 64 and I walk every morning with a cane, not a walker. It’s not about curing it-it’s about reclaiming your life one step, one sock, one foot check at a time. You’re still you. The nerves just got loud.
katia dagenais
December 1, 2025 AT 04:08Let me just say-this whole post is sooo 2020. Everyone’s obsessed with Lyrica and Qutenza like they’re holy grails, but have you considered that maybe the real issue is systemic neglect? The medical industrial complex profits off chronic pain, not cures. Why do you think they push expensive patches and drugs over lifestyle? Because pills are billable. B12 shots? Free. Foot inspections? No CPT code. And don’t even get me started on how insurance denies scrambler therapy unless you’ve already tried 17 meds and failed. It’s not medicine-it’s capitalism with a stethoscope.
Also, ‘idiopathic’ just means ‘we don’t know and we’re too lazy to dig deeper.’ I’ve had neuropathy for 12 years and no one ever tested my heavy metal levels. Lead? Mercury? Mold toxicity? Nah. Let’s just give you more gabapentin and call it a day.
And yes, I’ve tried everything. Even the acupuncture. It felt like needles in my soul. But I still believe the answer isn’t in a pharmacy-it’s in detoxing your environment, your diet, your trauma. Your nerves aren’t just broken-they’re screaming for justice.
Jack Riley
December 2, 2025 AT 01:27So let me get this straight-we’re told to take a drug that makes you dizzy as hell, then pay $1500 for a machine that tricks your brain into pretending your feet don’t feel like they’re on fire, while the real solution-cutting sugar, quitting booze, taking B12-is free, simple, and ignored because it’s not sexy enough for Big Pharma? Of course. We live in a world where you can buy a $400 smart sock that tracks your steps but won’t tell you if your nerves are dying. We’re not treating disease. We’re performing grief rituals with insurance forms.
And the worst part? The people who actually heal? They’re the ones who stopped listening to doctors and started listening to their bodies. I stopped eating processed food. I started walking barefoot on grass. I took B12 like it was oxygen. Two years later, I can feel my toes again. Not perfectly. But enough to know I’m still alive. Not a patient. A person.
Caroline Marchetta
December 4, 2025 AT 00:38Oh, wonderful. Another article that treats peripheral neuropathy like a DIY project you can fix with orthotics and tai chi. Let me just grab my lavender-scented foot soak and my affirmations while my nerves slowly turn to ash. How thoughtful of you to suggest I ‘check my feet’ like I’m not already terrified every time I step out of bed. And yes, I know about the B12. I’ve been taking it since 2019. It didn’t fix the fact that I can’t feel my husband’s hand when he holds mine. So thank you for the pamphlet. Truly. I’ll frame it next to my divorce papers.
Josh Zubkoff
December 4, 2025 AT 07:08Look, I’ve read this whole thing and I’m just going to say it-this is the most tone-deaf, oversimplified, corporate wellness garbage I’ve seen since someone told me to ‘just meditate’ after my heart attack. You talk about ‘early intervention’ like it’s a choice. What if you’re uninsured? What if you work two jobs and your doctor won’t see you for six months? What if you’re 72 and your kid is in rehab and you’re too tired to care about monofilament tests? This isn’t a blog post. It’s a luxury. And the fact that you think ‘walk more’ and ‘eat greens’ is a solution for people who can’t afford shoes, let alone scrambler therapy, is morally obscene. Stop pretending this is about health. It’s about privilege.
Also, ‘idiopathic’ isn’t a mystery-it’s a euphemism for ‘we don’t care enough to figure it out.’ And the fact that you didn’t mention opioid addiction rates in the elderly? That’s not an oversight. That’s complicity.
Jacqueline Aslet
December 5, 2025 AT 12:52While the article presents a comprehensive overview of peripheral neuropathy and its management, one cannot help but observe the implicit epistemological bias toward biomedical reductionism. The emphasis on pharmacological interventions and technological solutions such as scrambler therapy, while clinically relevant, inadvertently marginalizes the phenomenological experience of chronic pain as a lived, embodied condition. The suggestion that ‘early intervention improves response rates by 40%’ presumes a linear model of healing that neglects the nonlinear, often regressive nature of neurological degeneration. Furthermore, the absence of any discourse on socioeconomic determinants-such as food deserts, access to physical therapy, or the psychological toll of medical gaslighting-renders the proposed strategies functionally inaccessible to the very populations most affected. One is left to question: Is this a guide to healing, or a manual for compliance?