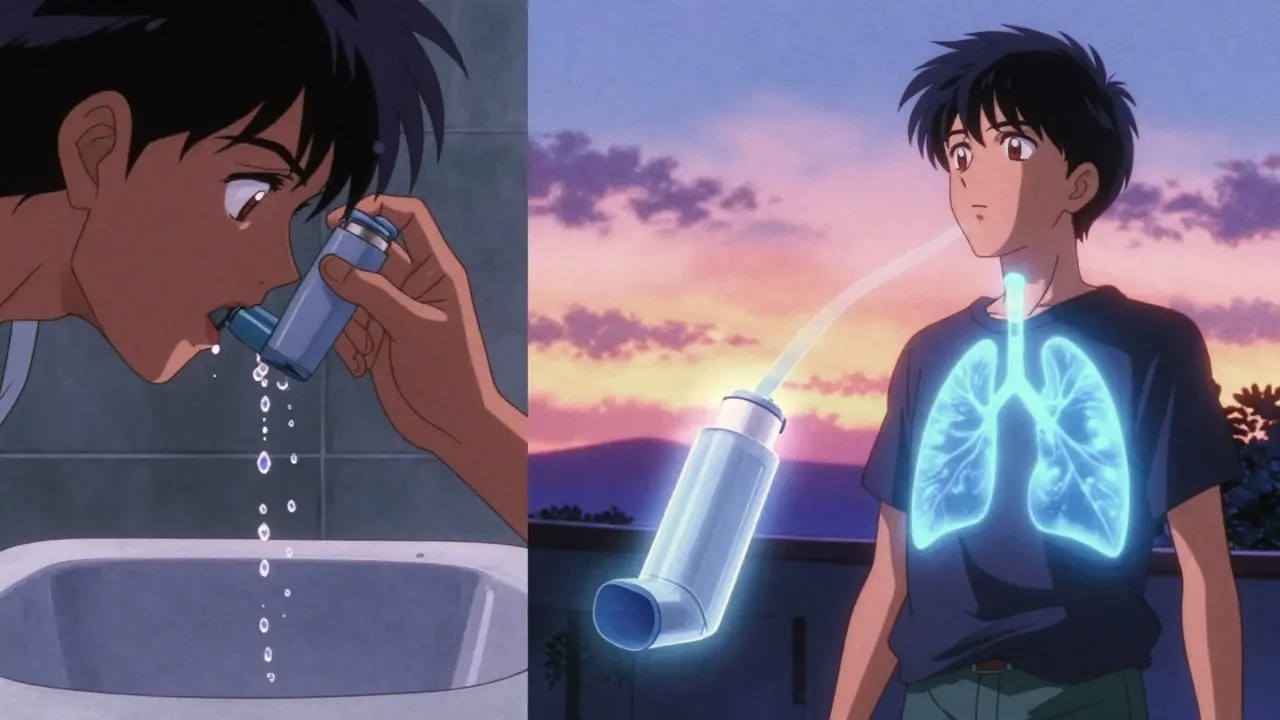
Millions of people with asthma or COPD rely on inhalers every day. But here’s the hard truth: if you’re not using your inhaler right, you might as well be breathing in air. Studies show that 70% to 90% of people get less than 30% of their medication into their lungs because of poor technique. That means your inhaler isn’t working - not because the medicine is weak, but because you’re not using it the way it was designed to be used.
Why Technique Matters More Than the Device
It doesn’t matter if you have the latest, most expensive inhaler. If you press the button too early, don’t hold your breath long enough, or inhale too fast, the medicine ends up stuck in your mouth or throat. That’s not just wasted medication - it’s a risk. Inhaled steroids can cause thrush, hoarseness, or even pneumonia if they sit in your mouth. And if you’re not getting enough medicine into your lungs, your symptoms won’t improve. You might end up using your rescue inhaler more often, or worse, wind up in the emergency room.Research from the National Heart, Lung, and Blood Institute (NHLBI) shows that correct technique can double how much medicine reaches your lungs - from as low as 8% to as high as 60%. That’s not a small difference. That’s the difference between breathing easily and struggling to catch your breath.
Three Main Types of Inhalers - And How Each Works
There are three types of inhalers you’re likely to be prescribed. Each one works differently, and each requires a different technique.- Metered-Dose Inhalers (MDIs) - These are the classic press-and-breathe devices. You’ll see them in brands like ProAir HFA or Ventolin. They use a propellant to spray out a puff of medicine. But here’s the catch: you have to press the canister and breathe in slowly at the exact same time. Most people mess this up. They press too early, too late, or breathe too fast.
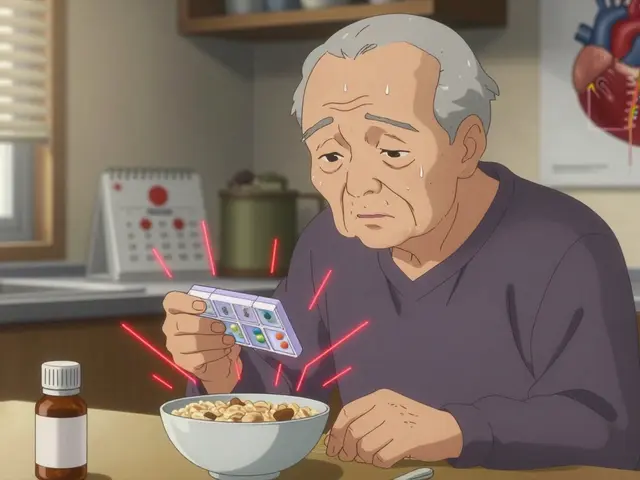
- Dry Powder Inhalers (DPIs) - These include devices like the Diskus, Ellipta, and Turbuhaler. They don’t use propellant. Instead, they release a fine powder when you inhale quickly and forcefully. This sounds simple - until you realize you need to generate a breath flow of 60 to 90 liters per minute. That’s hard if you’re older, weak, or having a flare-up.
- Soft Mist Inhalers - The Respimat is the most common one. It doesn’t spray. It releases a slow, gentle mist over 1.5 seconds. This gives you more time to inhale, which helps if you struggle with timing. But you still need to breathe in slowly and deeply.
Here’s the surprising part: MDIs with a spacer deliver just as much - or even more - medicine than DPIs. A spacer is a plastic tube you attach to the inhaler. It holds the puff of medicine so you can breathe in slowly without timing it perfectly. The Global Initiative for Asthma (GINA) recommends spacers for everyone, especially children and older adults.
How to Use an MDI With a Spacer - Step by Step
If you’re using an MDI, this is the best way to make sure you get the full dose:- Shake the inhaler well - at least 5 shakes. Skipping this means the medicine isn’t mixed right. Studies show 45% of users forget this.
- Attach the spacer. Make sure it’s clean and dry.
- Breathe out fully - not into the spacer, just away from it.
- Put the spacer mouthpiece in your mouth. Seal your lips around it.
- Press the inhaler once to release one puff into the spacer.
- Breathe in slowly and deeply through your mouth. Count to 5 as you inhale.
- Hold your breath for 10 seconds. This lets the medicine settle in your lungs. Most people exhale too soon - cutting effectiveness by 20-30%.
- Breathe out slowly.
- If you need a second puff, wait at least 60 seconds before repeating.
And don’t forget: rinse your mouth with water and spit it out after using any steroid inhaler. It cuts your risk of oral thrush by 75%.

How to Use a Dry Powder Inhaler - What Most People Get Wrong
DPIs are popular because they’re easier to carry and don’t need a spacer. But they have their own traps.- Never exhale into the device. If you blow into it before inhaling, you’ll ruin the powder. It clumps and won’t reach your lungs.
- Inhale fast and hard. You need to create a strong, deep breath - not a slow one. If you’re weak or tired, this can be hard. That’s why many older patients struggle.
- Don’t open the capsule. Some DPIs use capsules you load. Never, ever open them. The powder is meant to be inhaled from the capsule. 15% of users try to open them - and end up wasting their dose.
- Don’t use a spacer. Spacers don’t work with DPIs. They trap the powder. The Cleveland Clinic says this cuts effectiveness by 50-70%.
If you’re using a DPI and still coughing or feeling the powder in your throat, you’re probably breathing too slowly. Try standing up, taking a big breath from your belly, and then inhaling sharply through the mouthpiece.
Common Mistakes - And How to Fix Them
Here’s what most people do wrong - and how to fix it:- Not shaking the inhaler - Always shake it. Even if it feels like there’s no liquid inside.
- Not holding breath long enough - Aim for 10 seconds. Set a mental timer. If you can’t count to 10, try saying "elephant" slowly - that’s about 10 seconds.
- Exhaling into the device - Always breathe out first, then inhale.
- Using multiple inhalers without training - Switching between MDIs and DPIs without practice causes confusion. The European Respiratory Society says this reduces effectiveness by 35-50%.
- Storing inhalers in hot places - Keep them at room temperature. Above 30°C, the medicine loses 15-20% of its strength.
What to Do If Your Inhaler Isn’t Working
If you’ve been using your inhaler the same way for years and still feel short of breath - you’re not alone. But you’re not stuck.Ask your doctor or pharmacist to watch you use it. Don’t be embarrassed. Most professionals expect this. The UK Inhaler Group says the average patient needs three practice sessions to get it right. Some need five. That’s normal.
Also, ask if you’re on the right device. If you’re older or have severe COPD, a DPI might be too hard. An MDI with a spacer could be better. If you’re young and active, a DPI might be more convenient. Your doctor should help you choose based on your strength, coordination, and lifestyle - not just what’s cheapest.
Technology Is Helping - But It’s Not a Replacement
New smart inhalers like the one from Propeller Health track when you use your inhaler and whether your technique is correct. A 2022 study found they’re 92% accurate. That’s impressive. But they don’t fix technique - they just tell you you’re doing it wrong. You still need to learn how to breathe right.By 2025, 40% of inhalers will have some kind of digital feedback. But until then, your best tool is still your doctor, a spacer, and practice.
Final Advice: Don’t Guess. Get Checked.
Inhalers are powerful tools - but only if you use them right. The good news? You can fix this. You don’t need to be a medical expert. You just need to know the steps.Here’s what to do next:
- Watch a video from the American Lung Association or NHLBI - they have free, clear tutorials.
- Ask your pharmacist to show you how to use your specific device. Do it in front of them.
- Practice in front of a mirror. Watch your lips, your breath, your timing.
- Set a reminder: every 3 months, review your technique. Even if you feel fine.
Proper inhaler use isn’t about following rules. It’s about getting the medicine where it needs to go - into your lungs - so you can breathe easier, sleep better, and live without fear.
What happens if I don’t use my inhaler correctly?
If you don’t use your inhaler correctly, only 8-30% of the medication reaches your lungs. The rest stays in your mouth or throat. This means your symptoms won’t improve, you might need to use your rescue inhaler more often, and you increase your risk of side effects like oral thrush or pneumonia. Over time, poor technique can lead to more hospital visits and worse long-term lung damage.
Can I use a spacer with any inhaler?
No. Spacers only work with metered-dose inhalers (MDIs). They do not work with dry powder inhalers (DPIs) - using one with a DPI can reduce medication delivery by 50-70%. Always check the instructions for your specific device. If you’re unsure, ask your pharmacist.
Why do I need to hold my breath for 10 seconds?
Holding your breath for 10 seconds lets the medication settle in your airways and lungs. If you exhale too soon, much of the medicine gets pushed back out. Studies show this simple step increases lung deposition by 20-30%. It’s not optional - it’s essential.
Should I rinse my mouth after using my inhaler?
Yes - especially if it contains a steroid. Rinsing your mouth with water and spitting it out cuts your risk of oral thrush by 75%. Don’t swallow the water. Just swish and spit. This is one of the easiest ways to prevent side effects.
Is one type of inhaler better than another?
When used correctly, all inhalers are equally effective. But real-world use matters more. MDIs with spacers are often the best choice for older adults or those with weak breath. DPIs are good for younger, healthier people who can inhale forcefully. The best inhaler is the one you can use correctly every time.



Sarah Barrett
February 14, 2026 AT 22:41It’s wild how something so simple - breathing in - can be so wildly misunderstood. I used to think my inhaler was broken because I still felt like I was drowning after using it. Turns out, I was pressing the canister like I was starting a lawnmower. The spacer game changed everything. Suddenly, I could actually feel the medicine floating down, like a quiet snowfall in my lungs. No more throat grit. No more panic attacks from wheezing. Just… air. Easy air.
And rinsing? Absolute non-negotiable. I keep a little bottle of water by my bed now. Swish. Spit. Done. It’s the smallest ritual with the biggest payoff.
Also - never exhale into a DPI. I did that once. Felt like I’d swallowed a handful of powdered glass. Lesson learned the hard way.
Turns out, your lungs don’t care about brand loyalty. They just want you to be quiet, slow, and intentional.
Erica Banatao Darilag
February 15, 2026 AT 09:06i just reaaldy want to say thank you for writting this. i’ve been using my inhaler for 12 years and never knew i was doing it wrong. i thought the puff was supposed to be quick and sharp like a sneeze. turns out i was just spraying medicine on my tongue. now i use a spacer and hold my breath for 10 seconds. i even set a timer on my phone. it feels like i can finally breathe again. thank you thank you thank you.
p.s. i still forget to shake it sometimes. im working on it. 😅
Esha Pathak
February 17, 2026 AT 01:33Life is a paradox, isn’t it? We are given tools to heal - yet we are never taught how to hold them. The inhaler is not a magic wand. It is a mirror. It reflects our haste, our distraction, our refusal to slow down. We live in a world that rewards speed - but the lungs? The lungs demand stillness.
That 10-second hold? It’s not medical advice. It’s meditation.
And the spacer? It’s not a gadget. It’s a teacher. It says: ‘Wait. Let the medicine breathe before you do.’
We are not broken. We are just untrained. And that… is a quiet revolution waiting to happen.
✨
Mike Hammer
February 17, 2026 AT 18:09Yup. I used to think my inhaler was junk. Turns out I was the junk. 😅
Used to just press and cough. Now I use a spacer, shake it like I’m trying to wake up a sleeping baby, hold my breath like I’m trying to smell a flower, and rinse like I’m brushing my teeth after a burrito. It’s a whole routine now. I even got my wife to do it with me. We’re like inhaler twins now.
Also - never blow into a DPI. I did it once. Felt like I’d inhaled a bag of chalk. Don’t be me.
Daniel Dover
February 19, 2026 AT 14:00Spacer works. Rinsing helps. Hold your breath. Simple. Done.
Chiruvella Pardha Krishna
February 20, 2026 AT 10:44There is a deeper truth here - one that transcends medicine. The inhaler is not merely a device. It is a test of discipline. To inhale slowly is to resist the chaos of modern life. To hold your breath is to refuse the urgency of the moment. We are conditioned to consume - quickly, loudly, impatiently. But the lung does not respond to haste. It responds to reverence.
One day, perhaps, we will not need inhalers. But until then - let us breathe as if our lives depend on it. Because they do.
Joe Grushkin
February 21, 2026 AT 15:49Look - this whole post is just a pharmaceutical marketing tactic dressed up as health advice. Spacers? They’re bulky. DPIs? They’re fine if you’re not a geriatric. And don’t even get me started on the 10-second hold - that’s not science, that’s dogma. I’ve been on inhalers for 20 years. I press. I breathe. I live. You’re overcomplicating a simple thing. Also - who the hell has time to rinse their mouth after every puff? This isn’t a spa day. It’s a lung crisis.
Stop telling people how to breathe. Let them live.
Virginia Kimball
February 22, 2026 AT 15:16OMG I DIDN’T KNOW I WAS DOING IT ALL WRONG!! I’ve been using my inhaler like a soda can since 2018 😭
Just tried the spacer method today - and I swear, I felt the medicine GO IN. Like, actually GO IN. No more throat scratch. No more wheeze after 5 minutes. I even did the 10-second hold and counted ‘elephant’ like you said. It worked. I’m crying. Not from sadness - from ‘oh my god I can actually breathe again’.
Shoutout to the person who wrote this. You just changed my life. 🙌 Now I’m telling everyone I know. Let’s get our lungs the love they deserve 💙
Michael Page
February 23, 2026 AT 14:10My father used an MDI without a spacer for 15 years. He thought he was fine. Then he got pneumonia. Twice. The doctors said it was likely from the steroid residue. He started using a spacer. Now he walks 3 miles a day. No more ER visits. No more oxygen at night.
It’s not glamorous. It’s not trendy. But it’s the quietest kind of victory - the kind that happens when you stop rushing, and start listening.
He didn’t need a new inhaler. He needed to be shown how to use the one he already had.