Pain Management: Practical Tips and Medication Guides
If pain is messing with your daily routine, you’re not alone. Whether it’s a nagging back ache, migraine, or post‑surgery soreness, the right approach can make a huge difference. Below you’ll find easy‑to‑follow advice on medicines, over‑the‑counter options, and non‑drug methods that actually work.
Medication Options for Pain Relief
First, let’s talk meds. Over‑the‑counter drugs like ibuprofen or acetaminophen are good for mild to moderate pain. They work fast, but don’t overdo them—follow the label and watch for stomach irritation if you take NSAIDs regularly.
For stronger pain, doctors may prescribe opioids, muscle relaxants, or specific nerve‑pain drugs such as gabapentin. Opioids can be effective for short‑term use, but they carry a risk of dependence, so they should be paired with a clear taper plan.
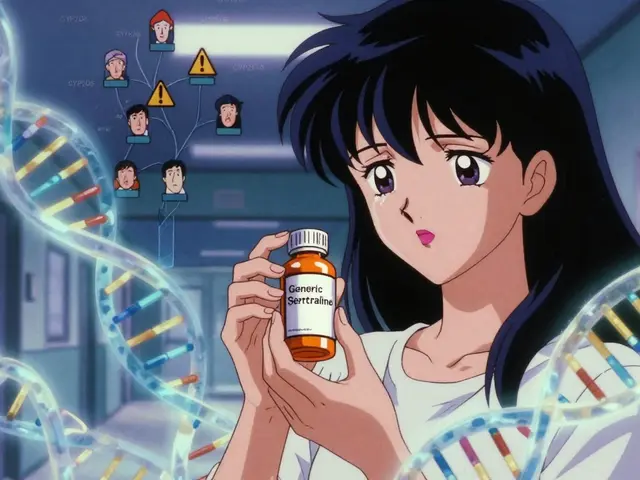
Don’t forget about prescription alternatives like topical creams (lidocaine, diclofenac) or COX‑2 inhibitors that target inflammation without hurting your stomach as much. When choosing a prescription, ask your pharmacist about possible drug interactions—especially if you’re on blood thinners or antidepressants.
Non‑Drug Strategies to Manage Pain
Medications are only one piece of the puzzle. Physical therapy can strengthen muscles around a painful joint, reducing strain and boosting mobility. Simple home exercises—like gentle stretches for the neck or a daily walk—often lessen chronic back pain without any pills.
Heat and cold therapy are cheap, effective tricks. Apply a heating pad for stiff muscles, or a cold pack for swelling and bruises. Switch every 15‑20 minutes and you’ll notice the tension easing.
Mental techniques matter, too. Deep breathing, guided meditation, or progressive muscle relaxation can lower the brain’s pain signals. Even a five‑minute daily mindfulness practice can shift your perception of pain.
Finally, watch your diet. Foods rich in omega‑3 fatty acids—like salmon, walnuts, and flaxseed—have anti‑inflammatory properties. Cutting back on processed sugars and saturated fats can also reduce systemic inflammation, which often fuels chronic pain.
Putting it all together, start with a clear plan: identify the type of pain, try a low‑risk medication or topical, add movement, and support the effort with heat, cold, and stress‑relief techniques. If pain persists beyond a couple of weeks or worsens, schedule a visit with your healthcare provider to explore stronger options or specialist referrals.
Remember, pain management isn’t a one‑size‑fits‑all game. Mix and match what works for you, stay consistent, and keep an eye on side effects. With the right combo, you can reclaim comfort and get back to the activities you love.
How Postherpetic Neuralgia Links to Chronic Fatigue Syndrome
By Lindsey Smith On 26 Sep, 2025 Comments (15)

Explore the biological overlap between postherpetic neuralgia and chronic fatigue syndrome, covering shared mechanisms, symptoms, and treatment strategies in a clear, evidence‑based guide.
View More