When you’re on treatment for osteoporosis, waiting a year or two to see if your bone density improves can feel like flying blind. That’s where bone turnover markers come in - they give you real-time feedback on whether your medication is working, long before a scan can show results.
What Are Bone Turnover Markers?
Bone is never static. Every day, old bone breaks down and new bone forms in a process called remodeling. Bone turnover markers (BTMs) are tiny protein fragments and enzymes released into your blood or urine during this process. They act like biological signals - telling doctors whether bone is being broken down too fast (resorption) or built up too slowly (formation).
There are two main types:
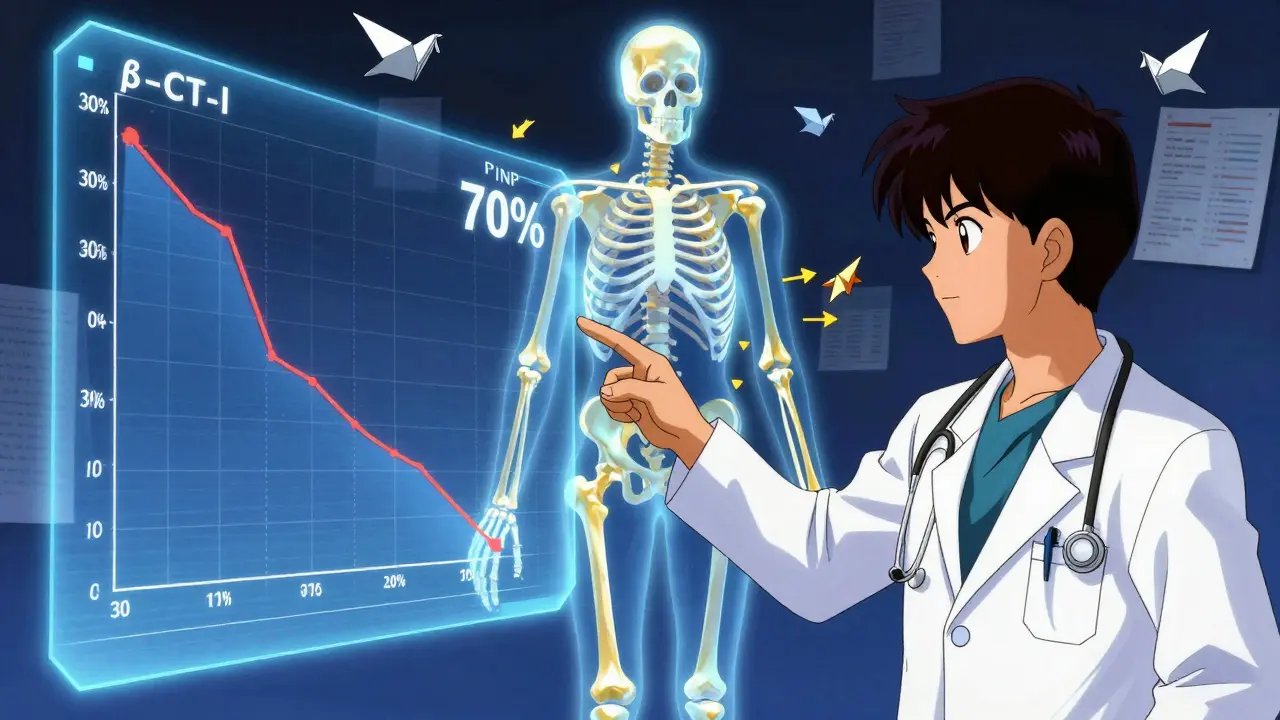
- Resorption markers: Show how quickly bone is being broken down. The gold standard is β-CTX-I (beta-C-terminal telopeptide of type I collagen), measured in plasma.
- Formation markers: Show how fast new bone is being made. The most reliable is PINP (procollagen type I N-terminal propeptide), measured in serum.
These aren’t just lab curiosities. They’re backed by the International Osteoporosis Foundation and European Calcified Tissue Society, who named PINP and β-CTX-I as the only two markers reliable enough for routine clinical use. Other markers like osteocalcin or NTx exist, but they’re less consistent and harder to compare across labs.
Why Use Them Instead of Just Waiting for a DXA Scan?
DXA scans - the standard test for bone density - are accurate, but slow. You need 12 to 24 months to see a meaningful change in your T-score. Meanwhile, BTMs respond within weeks.
If you start a bisphosphonate or denosumab (anti-resorptive drugs), your β-CTX-I levels can drop by 30% or more in just 3 months. That’s a clear sign the drug is working. If your PINP rises 70% after starting teriparatide (an anabolic drug), that tells you your body is building new bone.
Compare that to DXA: a 1-3% change in spine density over two years might be statistically significant, but it doesn’t tell you if your body responded to the drug at all. BTMs fill that gap. They answer the question: Is this treatment having any biological effect?
When and How Are They Measured?
Timing matters - a lot. These markers aren’t like cholesterol levels that stay steady all day. They fluctuate based on when you eat, sleep, and even what time it is.
For β-CTX-I:
- You must fast overnight (no food or drink except water).
- Sample must be taken between 8 and 10 a.m.
- Even a light meal can raise CTX levels by 20-30%.
PINP is more stable - only a 10-15% daily variation - but it’s still best measured in the morning after fasting. Skipping these steps can make results meaningless.
The test itself is simple: a standard blood draw. No special prep beyond fasting. Results come back in a few days. Most hospitals and major labs in the UK and US now use automated immunoassays, which are faster and more consistent than older methods like ELISA.
What Counts as a Good Response?
Not every drop or rise means success. There’s a threshold - the least significant change (LSC) - below which the change could just be noise.
- For β-CTX-I: A drop of more than 25% from baseline is considered real.
- For PINP: A drop of more than 20% is meaningful.
But here’s the key: for anti-resorptive drugs like alendronate or zoledronic acid, you want to see a 30% or greater reduction in β-CTX-I within 3 to 6 months. If you don’t, you might be non-adherent - meaning you’re not taking your pills - or your body isn’t responding.
For anabolic drugs like teriparatide or romosozumab, PINP should jump by 70-100% within 1-3 months. If it doesn’t, your doctor might reconsider your treatment plan.
The TRIO study found that patients who hit this 30% reduction in CTX at 3 months had a 1.6% lower fracture risk after 22 weeks than those who didn’t. That’s not just a lab number - it’s a real-world protection against breaking a hip or spine.
Who Should Get Tested?
Not everyone needs BTMs. They’re most useful in specific situations:
- Starting a new osteoporosis drug - especially if you’ve had fractures before.
- When adherence is questionable - if you’ve missed doses or stopped pills, BTMs can catch it early.
- If you’re on long-term therapy and your doctor wants to check if you still need it.
- If you have chronic kidney disease - standard markers like PINP and CTX can be misleading due to reduced clearance. In those cases, bone alkaline phosphatase (BALP) or TRACP5b are better options.
- If you’re switching from one drug to another - to see if the new one is working faster than expected.
For most people on standard therapy, one baseline test and one at 3 months is enough. No need to repeat every few months unless something changes.
Limitations and Pitfalls
Bone turnover markers aren’t perfect. They show overall bone activity - not whether your hip or spine is getting stronger. That’s why DXA scans still matter. BTMs are the early warning system; DXA is the final report.
They also vary by age, sex, and ethnicity. Asian populations tend to have 15-20% lower baseline CTX levels than Caucasians. African populations often show higher PINP. Most reference ranges are still based on European data, so interpretation needs context.
Lab variability is another issue. Only about 65% of US labs follow the strict IFCC protocols. In the UK, adoption is better, but not universal. Always ask your lab if they use standardized methods for PINP and β-CTX-I.
And don’t forget: if you’re taking supplements like high-dose vitamin D or calcium, or have other conditions like hyperthyroidism or rheumatoid arthritis, your BTMs might be skewed. Always tell your doctor your full medical history.
What’s Next for Bone Turnover Markers?
The field is moving fast. Medicare and many UK insurers now cover PINP and β-CTX-I testing. The global market for these tests is growing at over 8% per year, driven by aging populations and better guidelines.
Future studies are looking at using BTMs to personalize treatment - for example, stopping bisphosphonates early in high responders to avoid rare side effects like atypical femur fractures. Trials are also testing whether BTM-guided therapy reduces fractures better than standard care.
The American Association of Clinical Endocrinologists is expected to update its guidelines in mid-2024 to include BTMs as a standard tool. That will push more clinics to adopt them.
Right now, the message from experts is clear: bone turnover markers aren’t optional extras. They’re essential for modern osteoporosis care. Used right, they help you avoid unnecessary drugs, catch non-adherence early, and give you confidence your treatment is working - not just hoping it is.
What to Do Next
If you’re on osteoporosis treatment:
- Ask your doctor if a baseline PINP or β-CTX-I test was done before you started.
- If not, request one - it takes 5 minutes and costs less than £40 in the UK.
- At your 3-month follow-up, ask for a repeat test.
- Compare the results. Did your β-CTX-I drop by more than 30%? Did your PINP rise by 70% if you’re on an anabolic drug?
- If the numbers don’t move, talk about why - are you taking your pills? Is the drug right for you?
Don’t wait for a fracture to happen before you know if your treatment is working. Bone turnover markers give you the answers - sooner, simpler, and without radiation.
Are bone turnover markers better than DXA scans for monitoring osteoporosis?
No - they’re not better, they’re different. DXA scans measure actual bone density and are the gold standard for diagnosis and long-term tracking. Bone turnover markers show how fast your bones are remodeling. They’re fastest way to know if your drug is working - within weeks - while DXA takes 1-2 years. Use both: BTMs for early feedback, DXA for final confirmation.
Can I test bone turnover markers at home?
Not yet. While point-of-care tests are in development, all current BTM testing requires a blood draw and lab analysis. You can’t do it at home with a finger-prick kit. Always have it done in a certified lab that follows IFCC standards for PINP and β-CTX-I.
Do I need to fast before a bone turnover marker test?
Yes - especially for β-CTX-I. You must fast overnight and have the blood drawn between 8 and 10 a.m. Eating even a small meal can raise CTX levels by 20-30%, making results useless. PINP is less sensitive, but fasting and morning timing are still recommended for accuracy.
Why do some doctors not use bone turnover markers?
Some don’t use them because they weren’t trained to interpret them, or their lab doesn’t follow standardized protocols. Others rely on tradition - waiting for DXA changes. But guidelines from the IOF and ESCEO now strongly recommend them. Adoption is rising, especially in Europe and among endocrinologists. If your doctor hasn’t mentioned them, ask why.
Are bone turnover markers covered by insurance in the UK?
Yes. NHS labs in the UK routinely test PINP and β-CTX-I for osteoporosis monitoring. There’s no charge to patients. Private clinics also offer the tests, typically costing between £30-£50. If your GP refuses to order them, ask for a referral to a bone health clinic or endocrinologist.
Can bone turnover markers predict fracture risk?
Not directly - but they’re strongly linked. High baseline levels of β-CTX-I or PINP mean faster bone loss and higher fracture risk. A drop in these markers after treatment correlates with lower fracture risk. The TRIO study showed patients who reduced CTX by 30% had 1.6% fewer fractures after 22 weeks. So while they don’t predict fractures like a crystal ball, they’re one of the best tools we have to reduce risk.



Lance Nickie
January 14, 2026 AT 01:31btms? more like btmfs. why do we need another lab test when the dxa already tells us everything? just take your pills and chill.
Acacia Hendrix
January 15, 2026 AT 15:58It's fascinating how the clinical utility of PINP and β-CTX-I has been validated by the IOF and ESCEO guidelines-particularly their adherence to IFCC-standardized immunoassays. The coefficient of variation for β-CTX-I under fasting conditions is <10%, making it a robust dynamic biomarker for treatment response, far superior to the noisy, low-sensitivity DXA changes that manifest only after 18–24 months. The TRIO data is especially compelling: a 30% reduction in resorption correlates with a statistically significant fracture risk reduction, not just a lab curiosity. This is precision medicine in skeletal pharmacology.
Milla Masliy
January 15, 2026 AT 22:30I love how this breaks it down without jargon overload. My mom’s on alendronate and was freaking out because her last DXA didn’t change-turns out her CTX dropped 35% at 3 months. She felt so much better knowing the meds were working. Also, the fasting thing? Totally didn’t know that. I’m sending this to my whole family now.
Avneet Singh
January 16, 2026 AT 21:11As someone who’s read the ESCEO position paper thrice, I must say: the fact that so many US clinicians still ignore BTMs is embarrassing. PINP and β-CTX-I aren’t optional-they’re the *only* objective, quantifiable indicators of therapeutic efficacy before structural changes occur. Relying on DXA alone is like judging a car’s engine by looking at the tires. And don’t get me started on labs that don’t follow IFCC protocols-those results are worse than useless.
Adam Vella
January 17, 2026 AT 20:37One must consider the epistemological framework underpinning biomarker interpretation. While BTMs offer temporal immediacy, they are inherently reductionist-reducing the complex, systemic phenomenon of bone homeostasis to two molecular fragments. The DXA, though slow, captures the emergent property of skeletal integrity. To privilege kinetics over structure is to mistake the map for the territory. A truly holistic approach demands both: the thermometer and the weather report.
vishnu priyanka
January 18, 2026 AT 04:07bro, i got my blood drawn last week for this and the phlebotomist was like ‘oh you’re doing the bone thing?’ like it’s a thing people do. i just nodded like i knew what i was doing. turns out i didn’t-but this post saved me. also, i fasted. for real. no coffee. no toast. i’m a changed man.
Diana Campos Ortiz
January 18, 2026 AT 16:23Thank you for this. I’ve been on teriparatide for 4 months and my PINP jumped 82%. I cried when I saw the result. For the first time, I felt like my body was healing, not just holding on. Please tell more people about this. It’s not just science-it’s hope.
Jesse Ibarra
January 20, 2026 AT 12:32Let’s be real: if your doctor isn’t ordering BTMs, they’re either lazy, outdated, or actively harming you. Bone density scans are 1990s tech. You’re not getting better-you’re just not breaking *yet*. This isn’t ‘maybe try this’-it’s medical malpractice to skip PINP and β-CTX-I. Stop letting your GP play doctor with your spine. Demand the test. Now.
jefferson fernandes
January 21, 2026 AT 06:00Just a quick note: if you’re on bisphosphonates and your CTX didn’t drop by 30% at 3 months, don’t assume it’s ‘just how your body is.’ Check your adherence first-missed doses = false negatives. Also, if you’re taking calcium with iron or antacids? That can interfere with absorption. Talk to your pharmacist. And if your lab doesn’t use standardized assays? Find a new one. Your bones aren’t a suggestion-they’re your foundation.