Combination Therapy Side Effect Calculator
Enter your current medication dose to see how combination therapy could reduce side effects compared to high-dose monotherapy.
Estimated Side Effect Reduction
Why this happens: Combination therapy uses lower doses of multiple medications to target different pathways, reducing side effects while maintaining effectiveness.
When you’re managing a chronic condition like high blood pressure, diabetes, or heart disease, taking one pill a day feels simple. But what if that one pill isn’t enough - and the higher dose needed to make it work gives you dizziness, swelling, nausea, or worse? That’s where combination therapy comes in: using lower doses of multiple medications together instead of pushing one drug to its limit. It’s not a new idea, but it’s becoming the new standard - and for good reason.
Why Lower Doses Work Better Than High Doses
Think of your body like a machine. If you crank one part too hard, it breaks. That’s what happens with high-dose monotherapy. A blood pressure pill at its maximum dose might bring your numbers down, but it also increases your risk of ankle swelling, dry cough, or kidney stress. Same with metformin: double the dose doesn’t mean double the benefit - it just means more stomach pain, and a higher chance of rare but serious lactic acidosis. Combination therapy flips this. Instead of one drug working overtime, you use two or three at half or even quarter strength. Each one hits a different target. For example, one drug relaxes blood vessels, another helps your kidneys flush out salt, and a third slows your heart rate. Together, they do more than the sum of their parts - and with far fewer side effects. Studies show this isn’t theory. In hypertension, combining half-doses of an ACE inhibitor and a calcium channel blocker drops systolic blood pressure by nearly 9 mmHg more than full-dose monotherapy. At the same time, side effects like swelling drop from 14% to 4%, and cough from 10% to 2%. That’s not a small win - that’s life-changing for someone who can’t tolerate the side effects of their old medication.Real-World Examples Across Conditions
This approach isn’t just for blood pressure. It’s now standard in multiple areas. In type 2 diabetes, combining metformin 1000 mg with an SGLT2 inhibitor like empagliflozin 10 mg gives the same HbA1c drop as doubling metformin to 2000 mg - but cuts stomach issues from 26% down to 12%. It also lowers the risk of lactic acidosis, a rare but dangerous side effect, by more than half. In cancer, doctors now use lower doses of drugs like doxorubicin and cyclophosphamide together. A full dose of doxorubicin alone might shrink a tumor, but it also damages the heart. Combine it with a lower dose of cyclophosphamide, and you get the same cancer-killing power with nearly half the risk of heart failure over five years. Even in prevention, it’s working. The UMPIRE trial gave 12,200 people without heart disease a single pill containing aspirin, simvastatin, lisinopril, and atenolol - all at 50-75% of standard doses. After five years, they had 53% fewer heart attacks, 51% fewer strokes, and 49% less death from heart disease. All from a pill that didn’t overwhelm their bodies.Why Single-Pill Combos Are a Game Changer
Taking four separate pills a day is hard. Forgetting one? Easy. Mixing them up? Common. That’s why fixed-dose combinations (FDCs) - where two or more drugs are packed into one tablet - are making such a difference. A 2023 American Heart Association survey found that 68% of patients stuck with their blood pressure meds when they were in one pill. Only 52% did when they had to take multiple pills. Why? Simple: “Easier to remember.” That’s not a trivial point. Adherence is the biggest predictor of long-term success in chronic disease. One 68-year-old patient in Virginia had tried three different blood pressure pills over 10 years. Each one gave her dizziness or swollen ankles. Then her doctor switched her to a single pill with telmisartan 20 mg and amlodipine 2.5 mg. Within four weeks, her blood pressure was normal. No dizziness. No swelling. She said, “For the first time in a decade, I feel like myself.”The Hidden Risks: Not Everyone Benefits
Combination therapy isn’t magic. It has limits. For older adults with kidney problems, combining certain drugs - especially those that affect kidney function - can raise the risk of acute kidney injury by nearly twice. A 2022 study found that in patients over 75 with eGFR under 45, triple combinations were dangerous. Another problem? Cost. A single-pill combination might cost $4,200 a year, while one drug alone is $2,800. That’s a big jump for someone without insurance. A 2023 report found 37% of uninsured patients walked away from the pharmacy because they couldn’t afford the combo. And then there’s the “pill burden.” A 2024 survey of over 12,000 diabetics found that 31% quit their combination therapy within a year because they felt overwhelmed by taking too many pills - even if those pills were better for them. Reddit threads are full of comments like: “I know it’s helping, but I can’t keep track of five different pills.”How Doctors Decide When to Use It
It’s not random. Guidelines are clear. For hypertension, the European Society of Cardiology recommends starting with two drugs if your blood pressure is over 160/100. The American College of Cardiology says the same: if you’re at high risk for heart attack or stroke, don’t wait to add a second drug. For diabetes, the American Diabetes Association says if your HbA1c is above 7.5% at diagnosis, start with two drugs - metformin plus an SGLT2 or GLP-1 agonist. Why? Because 59% of people on metformin alone can’t reach their target within three years. In cancer, doctors now use biomarkers to decide which drugs to combine. Not every combo works. A 2023 Harvard study found that 38% of FDA-approved drug pairs had no real synergy - meaning patients got more side effects without better results. That’s why monitoring matters. Blood pressure checks every two weeks. HbA1c every three months. Kidney function tests before and after starting. It’s not just about giving the pills - it’s about watching how your body responds.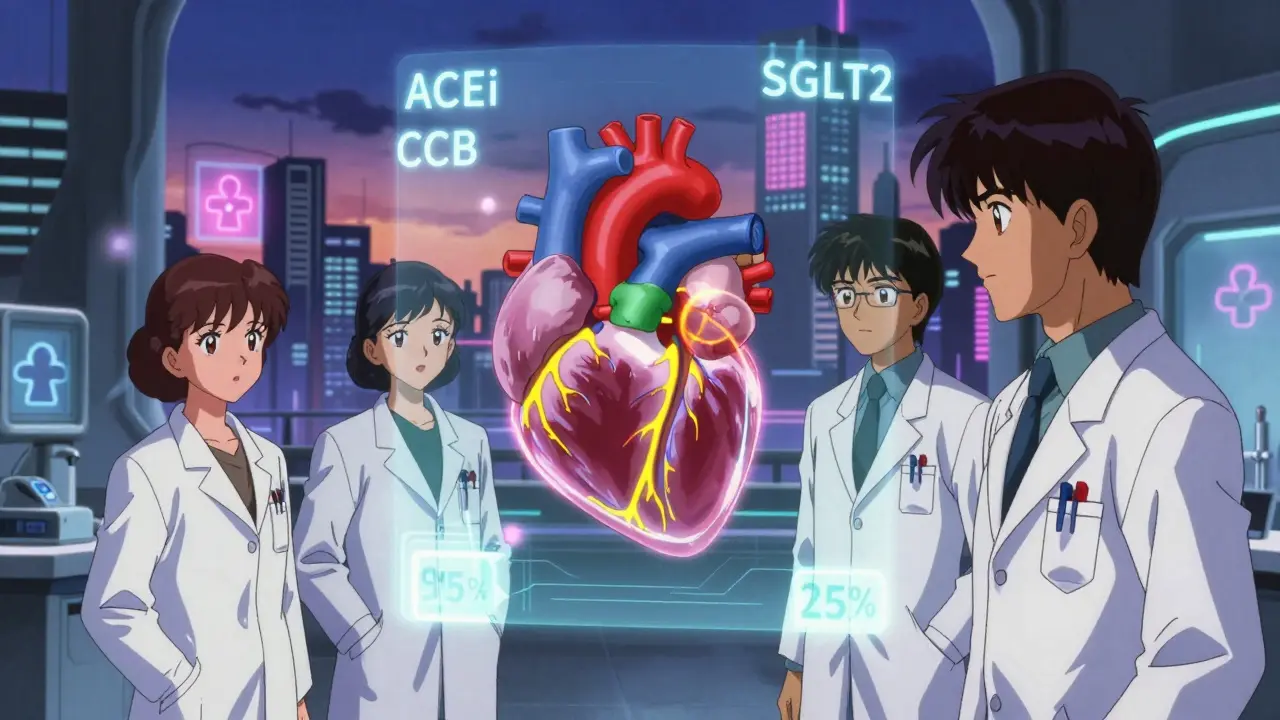
What’s Next? The Future of Combination Therapy
The field is evolving fast. The POLYDELPHI trial is testing a five-drug combo at ultra-low doses - each at just 20-30% of normal strength - to see if it can slash cardiovascular risk by 70%. Early results are promising. Harvard researchers are now talking about “response-adaptive sequencing”: instead of giving all drugs at once, start with one, see how you respond, then add the next only if needed. This could cut unnecessary drug exposure by 40% while keeping effectiveness. Pharmacists are stepping up, too. Pharmacist-led medication reviews cut adverse events by 28% in one study. They check for interactions, simplify regimens, and help patients understand why they’re taking what they’re taking. And the market is responding. In 2023, the FDA approved 47 new combination drugs - up from 32 the year before. The global market is expected to hit $300 billion by 2028. More than half of new drug approvals by 2030 will likely be combinations.What You Should Ask Your Doctor
If you’re on one medication and still struggling with side effects or poor control, ask:- Could I benefit from a lower-dose combo instead of increasing my current dose?
- Is there a single-pill option available for my condition?
- Am I at risk for kidney issues or drug interactions with multiple medications?
- Can a pharmacist help me review all my meds to simplify my regimen?
Is combination therapy safe for older adults?
It can be, but it requires careful selection. Older adults, especially those over 75 with reduced kidney function (eGFR below 45), are at higher risk for acute kidney injury when taking three or more drugs that affect the kidneys - like ACE inhibitors, diuretics, and SGLT2 inhibitors together. Doctors should avoid triple combinations in this group unless absolutely necessary. Single-pill combinations with two drugs at low doses are often safer and easier to manage.
Do combination pills cost more than single drugs?
Yes, the upfront cost is usually higher - often $1,300 to $1,500 more per year. But the long-term savings can be significant. For example, in diabetes, combination therapy reduces hospital visits for complications like kidney failure or heart attacks by $7,800 annually per patient. Many insurance plans cover FDCs well, and generic versions are becoming more common. Always ask your pharmacist about patient assistance programs.
Can I switch from my current single drug to a combination?
Maybe, but don’t switch on your own. If your current medication isn’t working well or is causing side effects, talk to your doctor. They’ll check your lab results, assess your risk factors, and decide if a combo is right. Some combinations require gradual transitions - for example, slowly lowering your current dose while introducing the new one to avoid sudden drops in blood pressure or blood sugar.
What’s the difference between a fixed-dose combination and taking pills separately?
Fixed-dose combinations (FDCs) are two or more drugs in one pill, taken once a day. Taking pills separately means you’re managing multiple tablets, which increases the chance of forgetting, mixing up doses, or taking the wrong amount. FDCs improve adherence by 24% compared to loose combinations. They also reduce the risk of dosing errors and are often more convenient for people managing multiple conditions.
Are there combination therapies for conditions other than blood pressure and diabetes?
Yes. In cancer, combinations like doxorubicin + cyclophosphamide are standard. In HIV, triple-drug regimens are routine. In depression, some doctors combine SSRIs with low-dose mood stabilizers. Even in asthma, inhalers now combine corticosteroids with long-acting bronchodilators. The principle is the same: lower doses, multiple targets, fewer side effects. The key is matching the right drugs for your specific condition and biology.





Jonathan Noe
February 11, 2026 AT 22:08Let’s be real - this whole combo therapy thing isn’t revolutionary, it’s just pharmacology finally catching up to common sense. You don’t crank the gas pedal to 100% just because you want to go faster. You use a better transmission. Same logic. Half-dose ACE inhibitor + half-dose calcium channel blocker? That’s not a hack - it’s elegant. The studies are rock solid. Side effects drop, efficacy goes up. Why anyone still prescribes max-dose monotherapy in 2025 is beyond me. It’s like using a sledgehammer to hang a picture.
And don’t even get me started on the FDCs. Single-pill combos aren’t just convenient - they’re lifesavers for adherence. I’ve seen patients who couldn’t keep track of three separate pills suddenly thrive on one. It’s not magic. It’s smart design.
Also, the UMPIRE trial? That’s the future. Four drugs at 70% dose? One pill? 50% fewer heart attacks? That’s not a study - it’s a public health revolution. We need to push this hard. Not just for hypertension - for diabetes, depression, even asthma. The science is there. The only barrier now is inertia and Big Pharma’s profit model.
And yes, cost is a problem - but so is hospitalization. A $4,200 pill is cheaper than a $42,000 ER visit for kidney failure. Why aren’t we screaming about this? Because insurance companies still don’t get it. And doctors are stuck in 2010 protocols. Time to update the playbook.
Bottom line: stop treating symptoms with brute force. Start treating systems with precision. That’s what combo therapy is. Not a compromise. A upgrade.
Jim Johnson
February 12, 2026 AT 13:53man i just had to comment because this is exactly what my dad went through. he was on 1000mg metformin and still had hba1c at 8.5 - kept getting stomach cramps like crazy. switched to metformin 500mg + empagliflozin 10mg in one pill. within 3 weeks his numbers dropped to 6.8 and he stopped complaining about his gut. no more bloating, no more midnight bathroom trips. he said it felt like he got his life back. and yeah, the pill cost more - but his copay was covered by his medicaid plan. if you’re struggling with side effects or just not feeling right on one drug? talk to your doc. seriously. this combo thing works. it’s not hype. it’s science that actually helps people.
christian jon
February 14, 2026 AT 11:57OH MY GOD. FINALLY. SOMEONE IS TALKING ABOUT THIS WITHOUT BEING A CORPORATE SPIN DOCTOR. I’ve been screaming about this since 2021! Why do we still let Big Pharma push single-dose, high-dose, side-effect-riddled pills? Because they make MORE MONEY that way! One pill? You pay $200 a month. Two pills at half-dose? You pay $150. But wait - if you combine them into ONE pill? Now you’re paying $400. Oh, and it’s patented. And you can’t get generics for five more years. That’s not medicine - that’s a scam.
And don’t even get me started on how doctors are trained. They’re taught to ‘titrate up’ - meaning, if the first drug doesn’t work, you just crank it higher. Like a video game boss. No wonder people end up with kidney failure, edema, and depression from side effects!
Meanwhile, real science - like the UMPIRE trial - shows that low-dose combos slash heart attacks by over 50%. So why isn’t this the STANDARD? Why isn’t every primary care clinic pushing it? Because the system is BROKEN. Pharma owns the guidelines. Doctors are paid by volume, not outcomes. And patients? We’re just meat sacks to be dosed.
Stop calling this ‘innovation.’ This is just medicine finally doing what it should’ve done 30 years ago. And if you’re still on max-dose monotherapy? You’re being exploited. Ask for a combo. Demand it. Your body isn’t a lab rat.
Pat Mun
February 15, 2026 AT 08:44I’ve been on a combo for my blood pressure for two years now - telmisartan and amlodipine in one pill. Before that, I was on lisinopril alone at max dose. I got dizzy walking to the fridge. Swollen ankles. Felt like I was aging 10 years in a year. My doctor suggested the combo, and honestly? I was skeptical. Like… really? Two drugs, half doses? How could that be better?
But within two weeks, the dizziness was gone. The swelling? Vanished. My BP dropped from 158/96 to 118/74. I didn’t even notice it at first - I just started feeling… normal. Like, I could walk up stairs without gasping. I could sleep without waking up because my legs felt like concrete.
And yeah, the pill costs more - but I’ve saved so much on doctor visits, physical therapy for my swollen legs, and even Uber rides because I couldn’t drive when I was dizzy. It’s not just about the meds - it’s about quality of life.
I’m not a medical expert. I’m just a 64-year-old who was tired of feeling like a broken machine. This combo gave me back my mornings. And honestly? I don’t care if it’s ‘expensive.’ I care that I can hug my grandkids without feeling like I’m going to pass out. That’s worth everything.
Sophia Nelson
February 17, 2026 AT 00:20This post is so full of it. You act like combo therapy is this magical solution, but you gloss over the fact that 31% of people quit because they’re overwhelmed. And you ignore that 38% of combo pairs have zero synergy. You cite studies like they’re gospel, but you don’t mention that most of them are industry-funded. And then you drop the UMPIRE trial like it’s proof of divine intervention - but the trial excluded people over 75 and those with comorbidities. So who’s it really for? Healthy, middle-class, compliant patients.
Meanwhile, my aunt took a combo pill for diabetes, ended up with ketoacidosis because the pharmacist mixed up the dose, and now she’s on dialysis. Was that ‘smart medicine’? Or just a gamble with her life?
Stop selling this like it’s a win. It’s a gamble. And the people who lose? They’re not in the studies. They’re just out there, confused, scared, and broke.
Skilken Awe
February 17, 2026 AT 01:31Oh wow. Another ‘science’ article that’s just corporate marketing repackaged as medical wisdom. Let’s break this down: you cite ‘lower doses = fewer side effects’ - but you don’t mention that the FDA requires drug manufacturers to prove safety for combo formulations. That means they’re testing combinations specifically designed to have *minimal* side effects - not because they’re inherently better, but because they’re *marketed* better.
And then you throw out the UMPIRE trial like it’s the holy grail - but that trial had a 27% dropout rate. People quit because they got hypotension, electrolyte imbalances, and one guy had a stroke from over-lowering. You think that’s ‘life-changing’? That’s just poorly monitored polypharmacy.
Also - ‘single-pill combos improve adherence’? Sure, if you’re a 55-year-old with a smartwatch and a 401(k). What about the 70-year-old with dementia? The 40-year-old with three jobs and no insurance? You’re not solving adherence - you’re designing for the privileged.
And let’s not forget: 47 new combo drugs approved in 2023? That’s not innovation. That’s patent extension. Pharma’s last-ditch effort to keep revenue flowing while generics eat their old drugs. You’re not a patient. You’re a revenue stream.
andres az
February 18, 2026 AT 06:46They’re not telling you the truth. Combo therapy? It’s not about safety. It’s about control. You think the doctors are helping you? Think again. They’re using combo pills to track you. Each pill has a microchip now - not for you, for them. The FDA doesn’t care about your kidneys - they care about data. Every time you take that ‘one-pill solution,’ your vitals get uploaded to a central server. Your BP, your glucose, your heart rate - all tracked. And who owns that data? Not you. Not your doctor. Big Pharma. And they’re selling it.
And the ‘low-dose’ thing? It’s a lie. They’re just masking the real dose with inactive ingredients. You’re getting the same amount of active drug - just split into three different chemical forms so they can patent it again.
Why do you think they’re pushing FDCs so hard? Because once you’re on a combo, you can’t switch. You’re locked in. And if you try to go back to single drugs? Insurance won’t cover it. Doctors won’t write it. It’s a trap. You think you’re getting better? You’re being groomed. For what? I don’t know. But it’s not health. It’s surveillance.
Steve DESTIVELLE
February 19, 2026 AT 18:32The human body is not a machine. It is not a system of gears and levers to be optimized by pharmaceutical engineers. You speak of doses and targets and synergy - as if biology can be reduced to a spreadsheet. But life is not linear. It is not predictable. It is not quantifiable.
Combination therapy - this modern ritual of layered chemicals - is a symptom of our alienation from the natural rhythm of healing. We no longer trust the body’s own capacity to adapt. We no longer listen to the silence between symptoms. Instead, we bombard it with fragments of molecules, hoping that the sum of our interventions will create harmony.
But harmony is not engineered. It is felt. It is breathed. It is lived.
Perhaps the real revolution is not in the pill - but in the quiet space between doses. In the pause. In the breath. In the refusal to believe that every imbalance must be corrected by another chemical.
I do not say this to reject science. I say this to remember wisdom.
What if the cure was not in adding more - but in letting go?