Candida Immune Response: What Your Body Needs to Know
When dealing with Candida immune response, the collection of cellular and molecular actions that detect, contain, and clear Candida infections. Also known as Candida immunity, it plays a critical role in keeping the common yeast in check. One of the main culprits behind overgrowth is Candida albicans, the most prevalent species that lives harmlessly on skin and mucous membranes until the host defenses slip. The body relies on innate immunity, the first‑line, non‑specific shield made up of barriers, phagocytes, and pattern‑recognition receptors to spot the fungus early. When those defenses falter, clinicians often turn to antifungal therapy, medications like fluconazole or echinocandins that directly inhibit fungal growth. Yet the story doesn’t end with drugs; the gut microbiome, the diverse community of bacteria, viruses, and fungi inhabiting the intestines shapes and fine‑tunes the immune response, influencing whether Candida stays benign or becomes problematic.
Key Components of the Candida Immune Response
The immune system tackles Candida on several fronts. First, physical barriers such as intact skin and mucosal layers prevent the yeast from breaching into deeper tissues. If it does slip through, epithelial cells release antimicrobial peptides that create a hostile environment. Next, pattern‑recognition receptors—especially Dectin‑1 and Toll‑like receptors—detect fungal cell wall components and trigger signaling cascades that mobilize neutrophils and macrophages. These phagocytes engulf the yeast, subject it to oxidative bursts, and present antigens to adaptive immune cells. Adaptive immunity then tailors a more specific attack, with Th17 cells producing IL‑17 that enhances neutrophil recruitment and antimicrobial peptide production. In short, Candida immune response intertwines innate detection, cellular killing, and adaptive fine‑tuning to keep the fungus in balance.
Several factors can tip this balance toward overgrowth. Broad‑spectrum antibiotics wipe out beneficial bacteria that compete with Candida, opening ecological niches. High‑sugar diets feed the yeast and impair neutrophil function. Hormonal shifts, such as elevated estrogen during pregnancy or oral‑contraceptive use, can modify fungal adhesion properties. Chronic stress suppresses cytokine production, weakening the Th17 pathway. Understanding these triggers helps explain why some people develop recurrent thrush, gut dysbiosis, or systemic candidiasis while others coexist peacefully with the same organism.
Treatment strategies reflect the layered nature of the response. For mild oral or vaginal infections, topical antifungals combined with probiotic supplementation often restore balance quickly. In more severe cases—like esophageal candidiasis or invasive bloodstream infections—systemic antifungal agents are essential, and clinicians may monitor immune markers like neutrophil counts or IL‑17 levels to gauge recovery. Emerging research points to immunomodulatory approaches: boosting Th17 activity with vitamin D or using microbiome‑based therapies to outcompete Candida. While these ideas are still in development, they underscore the principle that supporting the body’s own defenses can be as powerful as killing the fungus outright.
From a practical standpoint, readers will find a range of actionable insights in the posts below. You’ll discover how diet and lifestyle shape the gut microbiome, which antifungal options are safest for specific conditions, and what lab tests can reveal about your immune status. Whether you’re a patient dealing with recurrent infection, a caregiver seeking simple prevention tips, or a health professional looking for up‑to‑date comparative reviews, this collection offers clear, evidence‑based guidance. Dive in to learn how each piece of the Candida immune response works together, and how you can tip the scales in your favor.
Genetic Factors Behind Candidemia and Disseminated Candida Infections
By Lindsey Smith On 6 Oct, 2025 Comments (13)
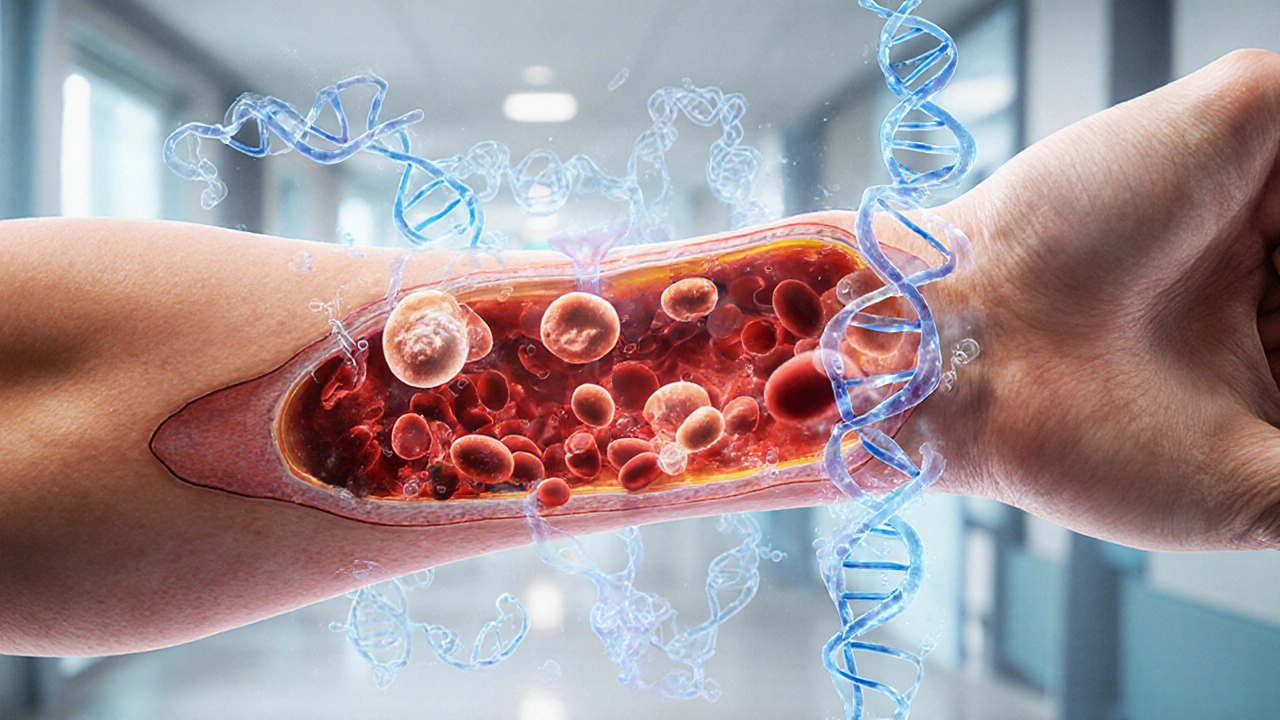
Explore how rare gene mutations and common genetic variants boost the risk of candidemia and spread of Candida, with practical guidance for testing and personalized care.
View More