Elderly Medication Dosing: Safe Ways to Adjust Pills for Older Adults
When it comes to elderly medication dosing, the process of adjusting drug amounts for older adults based on how their bodies process medicine. Also known as geriatric dosing, it’s not just about making pills smaller—it’s about understanding how aging changes how drugs are absorbed, broken down, and cleared from the body. As people get older, their liver and kidneys don’t work as fast, fat and muscle balance shifts, and brain sensitivity to certain drugs increases. A dose that’s safe for a 40-year-old can be dangerous for a 75-year-old.
This is why polypharmacy in elderly, the use of multiple medications at once by older adults. Also known as multiple drug regimens, it’s so common—and so risky. Over half of seniors take five or more prescriptions daily. That means more chances for harmful interactions, like grapefruit juice making statins too strong, or meclizine adding dizziness on top of blood pressure meds. It’s not just about the drugs themselves—it’s about how they pile up. One pill might be fine. Ten? That’s a minefield.
And then there’s age-related pharmacokinetics, how the body’s handling of drugs changes with age. Also known as pharmacokinetic changes in seniors, it’s the science behind why older people need lower doses. Their stomachs absorb drugs slower. Their blood has less water, so drugs concentrate more. Their kidneys filter out toxins at half the rate they did at 30. That means a drug that lasts 8 hours in a young person might last 16 in an older one. Gabapentin, amitriptyline, even common painkillers—each behaves differently. That’s why doctors now check liver enzymes, kidney function, and even cognitive status before prescribing.
It’s not just science—it’s survival. A single wrong dose can lead to falls, confusion, hospital stays, or worse. That’s why knowing the difference between Type A and Type B adverse drug reactions matters. Type A? Predictable, dose-related, like dizziness from blood pressure meds. Type B? Rare, unpredictable, like a sudden allergic reaction. Both happen more often in seniors. And when you combine that with how easily drugs interact—like statins and grapefruit juice, or tinidazole and alcohol—it becomes clear: elderly medication dosing isn’t a one-size-fits-all task. It’s a careful balancing act.
Below, you’ll find real-world guides on how specific drugs behave in older bodies, what to watch for, and how to avoid the most common mistakes. From statin safety and gabapentin dosing to understanding how route of administration changes side effects, these posts give you the facts you need to make smarter choices—for yourself or someone you care about.
Medication Dosage Adjustments for Aging Bodies and Organs: What Seniors and Caregivers Need to Know
By Lindsey Smith On 15 Nov, 2025 Comments (16)
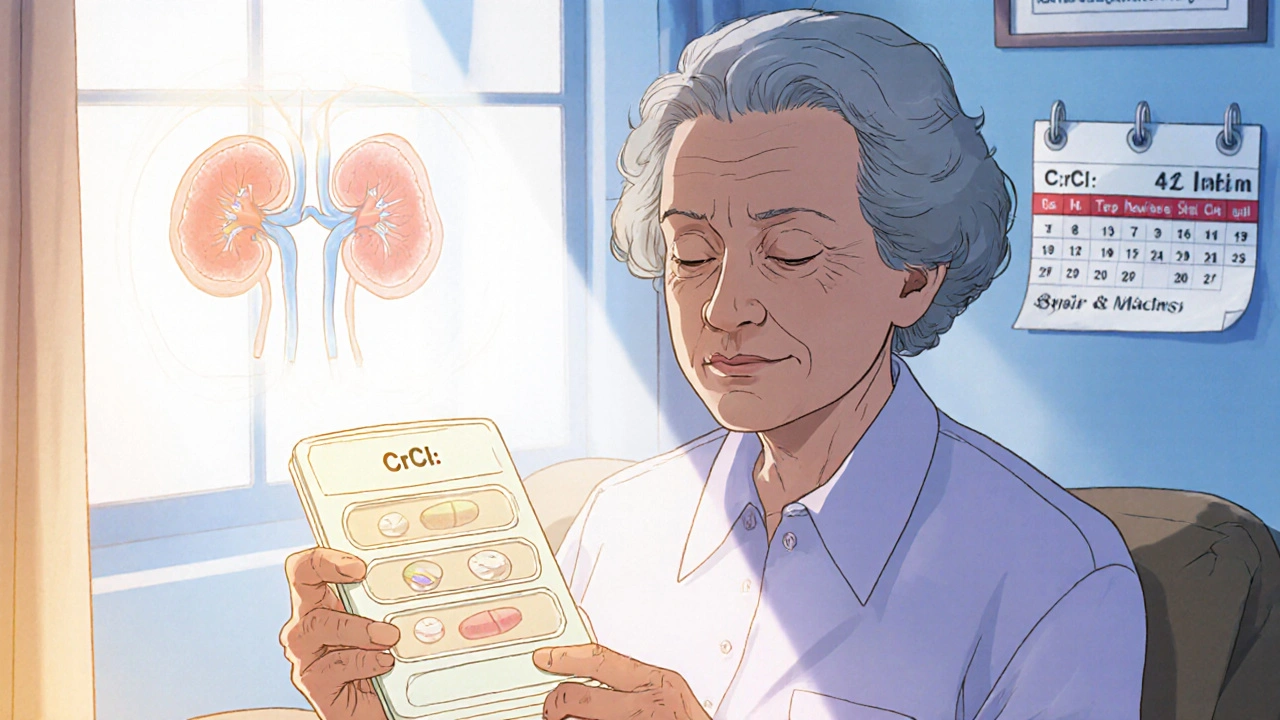
Aging changes how your body handles medication. Learn why seniors need lower doses, which drugs are risky, how kidney function affects dosing, and what you can do to avoid dangerous side effects.
View More