Exercise Therapy
When working with Exercise Therapy, a structured program that uses physical activity to prevent or treat health conditions. Also known as Physical Exercise Therapy, it closely connects with Physical Rehabilitation, the process of restoring function after injury or illness, Cardiovascular Fitness, the heart and lungs' ability to deliver oxygen during activity, and Musculoskeletal Health, the strength and flexibility of muscles and joints. These three pillars form the backbone of a holistic therapeutic plan.
Understanding exercise therapy can change the way you approach wellness. By tailoring movement to individual needs, it becomes a key tool in Chronic Disease Management, the long‑term coordination of conditions like diabetes, heart disease, or arthritis. Studies show that patients who pair medication regimens with regular aerobic activity experience fewer side‑effects and better overall outcomes. Likewise, mental health benefits are evident; structured exercise reduces anxiety, improves mood, and supports coping strategies for disorders such as panic attacks.
Key Benefits of Exercise Therapy
One major advantage is the improvement of cardiovascular fitness. Aerobic workouts—like brisk walking, cycling, or swimming—raise heart rate, boost oxygen delivery, and lower blood pressure. In parallel, resistance training builds muscle mass, which helps regulate glucose levels and supports joint stability. Flexibility and balance exercises, such as yoga or tai‑chi, protect against falls and maintain range of motion, crucial for older adults and those recovering from surgery. Together, these components address both the physical and metabolic aspects of health.
Designing an effective program requires attention to dosage, intensity, and progression—much like medication titration. A typical regimen starts with low‑to‑moderate intensity 3‑5 times per week, gradually increasing duration or resistance as tolerance improves. Monitoring tools like heart‑rate monitors or mobile apps help track adherence and ensure safety. Health professionals play a vital role in prescribing specific exercises, adjusting based on comorbidities, and educating patients about proper form to prevent injury.
Real‑world examples illustrate the synergy between drug therapy and movement. For instance, patients on Imatinib for chronic myeloid leukemia who incorporate regular aerobic sessions report decreased fatigue and better tolerance to dose escalations. Similarly, individuals using tibolone for menopause‑related mood swings benefit from light resistance work that steadies hormone fluctuations. These cross‑disciplinary successes highlight that exercise therapy isn’t a standalone fad—it’s an evidence‑based complement to pharmacologic care.
Beyond clinical settings, lifestyle factors amplify the impact of exercise therapy. A plant‑based diet, as shown in gout management research, can lower uric acid levels, while regular movement improves kidney clearance of metabolites. Nutrition, sleep hygiene, and stress‑reduction techniques all interact with physical activity to create a comprehensive health strategy. When you align these elements, you maximize the therapeutic window of both drugs and exercise.
Below you’ll find a curated collection of articles that dive deeper into dosing specifics, mental‑health coping, diet interactions, and more—all viewed through the lens of exercise therapy. Each post offers practical tips, evidence summaries, and clear action steps to help you integrate movement into your treatment plan.
How Physiotherapy Improves Injury Rehabilitation: Benefits & Practical Guide
By Lindsey Smith On 18 Oct, 2025 Comments (11)
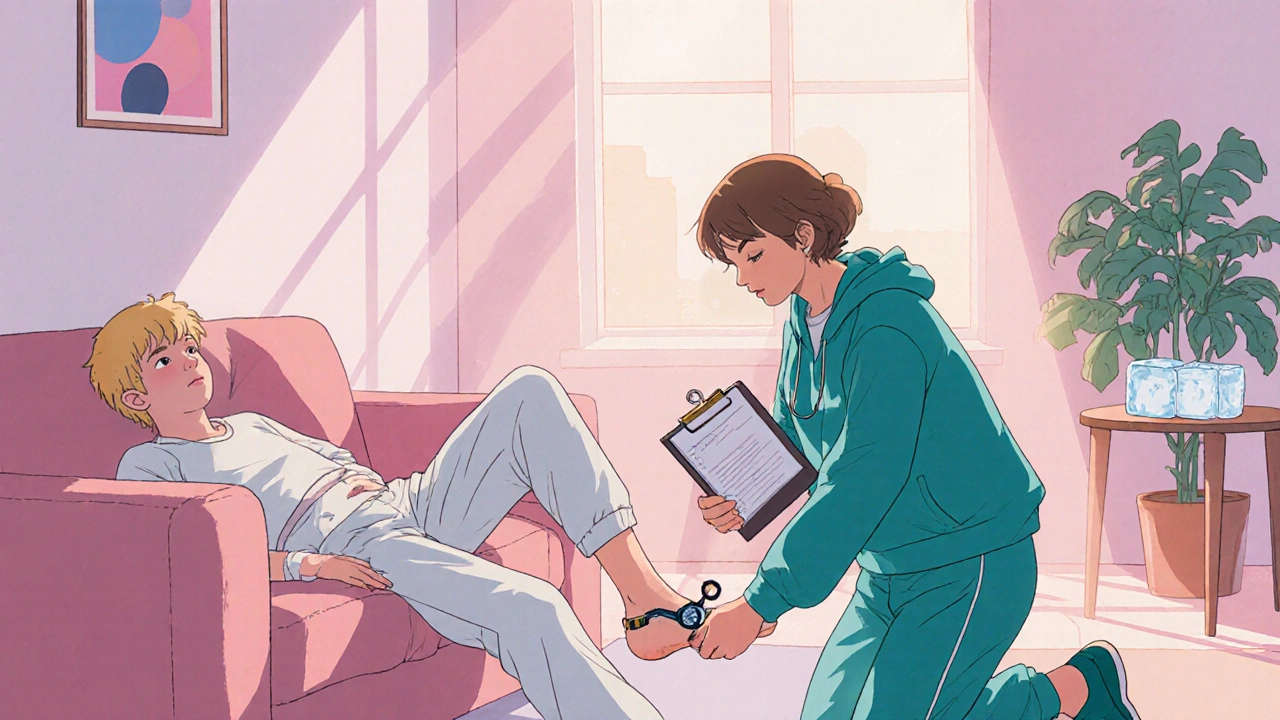
Discover how physiotherapy speeds up injury rehabilitation, the key techniques used, and how to create a personalized recovery plan for faster, safer healing.
View More