Mometasone Furoate Systemic Absorption Calculator
Estimate potential systemic absorption of mometasone furoate based on application area, duration, and patient type. The calculator uses clinical data showing systemic absorption ranges from 0.5-2% of applied dose.
When doctors prescribe a steroid for eczema or asthma, they often reach for a molecule that packs a lot of power into a tiny structure. Mometasone Furoate is a synthetic glucocorticoid designed to stay on the skin or in the lungs long enough to calm inflammation without flooding the bloodstream. In this guide we’ll break down exactly how its chemistry translates into therapeutic action, what makes it different from older steroids, and how to use it safely.
Chemical Structure at a Glance
The backbone of mometasone furoate is the classic cyclopentanoperhydrophenanthrene nucleus found in all steroids. Two key modifications set it apart:
- A 17‑alpha‑furoate ester that dramatically increases lipophilicity, allowing the drug to penetrate the stratum corneum and linger in the epidermal layer.
- A 16‑alpha‑methyl group that blocks metabolic reduction by hepatic enzymes, extending the half‑life when the drug is absorbed systemically.
These changes give mometasone a high topical potency (approximately 4‑5 times that of hydrocortisone) while keeping systemic exposure low.
Stereochemistry and Functional Groups
The molecule contains three chiral centers at C‑8, C‑9, and C‑10, all in the natural (S) configuration. The presence of a 3‑ketone and a 20‑hydroxyl group are typical of glucocorticoids and are essential for receptor binding.
Because of the 17‑alpha‑furoate ester, the compound is practically insoluble in water (logP ≈ 4.5). This property is why it’s formulated as creams, ointments, lotions, or inhalation aerosols, where a non‑aqueous vehicle can dissolve the drug.
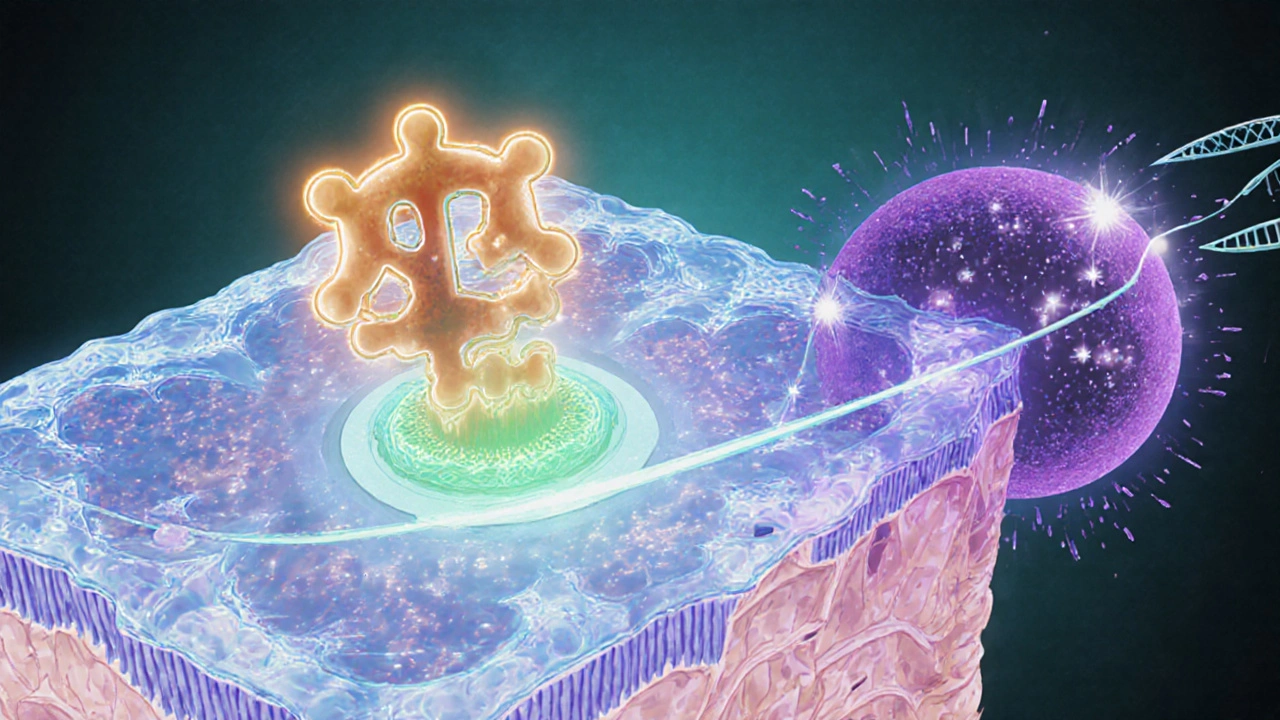
Mechanism of Action: Binding to the Glucocorticoid Receptor
Once the drug reaches its target tissue, it diffuses across the cell membrane and binds to the intracellular Glucocorticoid receptor a ligand‑activated transcription factor that regulates inflammatory genes. The steroid‑receptor complex then translocates to the nucleus, where it either:
- Activates anti‑inflammatory genes (e.g., annexin‑1, IL‑10).
- Represses pro‑inflammatory transcription factors such as NF‑κB and AP‑1.
By dampening cytokine release and reducing leukocyte infiltration, mometasone furoate quickly eases redness, itching, and swelling.
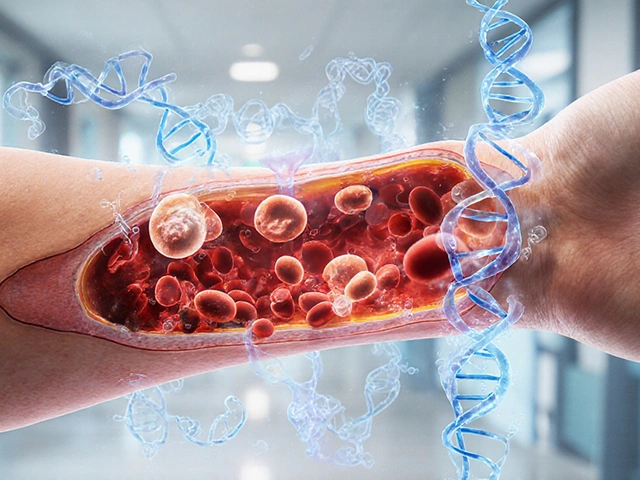
Pharmacokinetics: From Skin to System
After topical application, only about 0.5‑2% of the dose enters the systemic circulation. The high lipophilicity keeps most of the drug trapped in the epidermis, where it can act for up to 48 hours.
When inhaled, the drug’s particle size (1-3 µm) ensures deep pulmonary deposition. Absorption from the lungs is rapid, but first‑pass metabolism via the CYP3A4 enzyme the major hepatic cytochrome P450 isoform responsible for steroid clearance limits systemic exposure.
Key pharmacokinetic parameters:
- Peak plasma concentration (Cmax): 0.5-1 ng/mL after a standard 0.1 % cream applied twice daily.
- Half‑life (t½): 5‑7 hours for the intact ester; the active metabolite (mometasone) persists up to 12 hours.
- Volume of distribution (Vd): ≈ 0.3 L/kg, reflecting limited systemic spread.
Formulations & Clinical Indications
Mometasone furoate is marketed in several dosage forms, each targeting a specific route:
| Form | Strength | Typical Use | Key Advantage |
|---|---|---|---|
| Cream / Ointment | 0.1 % (1 mg/g) | Eczema, psoriasis, seborrheic dermatitis | High skin retention, low systemic risk |
| Metered‑dose inhaler (MDI) | 0.05 mg/actuation | Asthma, allergic rhinitis | Effective bronchodilation with minimal oral bioavailability |
| Nasal spray | 50 µg/spray | Seasonal allergic rhinitis | Rapid symptom relief, low systemic absorption |
For skin conditions, the 0.1 % cream is the most common prescription. Inhaled mometasone furoate (often under brand names like Asmanex) is a preferred step‑2 therapy for persistent asthma because it offers once‑daily dosing.
Safety Profile & Common Side Effects
Because only a tiny fraction reaches the bloodstream, systemic side effects such as adrenal suppression or Cushing‑like features are rare with proper use. However, local adverse events can occur:
- Skin atrophy or telangiectasia with prolonged high‑potency use.
- Secondary bacterial or fungal infection if the barrier is compromised.
- Inhalation: oral thrush; patients should rinse mouth after each dose.
Special populations-children, pregnant women, and patients with hepatic impairment-should use the lowest effective dose. Monitoring for growth retardation in pediatric eczema patients is recommended if therapy exceeds three months.
How Mometasone Stacks Up Against Other Steroids
When choosing a topical corticosteroid, clinicians weigh potency, duration of action, and safety. The table below spotlights the main differences between mometasone furoate and three frequently prescribed steroids.
| Agent | Relative Potency | Typical Indications | Systemic Absorption (% of dose) |
|---|---|---|---|
| Mometasone furoate (0.1 %) | Very high (≈4‑5× hydrocortisone) | Eczema, psoriasis, allergic rhinitis (inhaled) | 0.5‑2 % |
| Hydrocortisone (1 %) | Low | Mild dermatitis, diaper rash | 5‑10 % |
| Betamethasone dipropionate (0.05 %) | High (≈8× hydrocortisone) | Severe psoriasis, lichen planus | 1‑3 % |
| Budesonide (0.03 % inhaler) | Medium (inhaled only) | Asthma, COPD | ~2 % |
From a safety standpoint, mometasone’s ester side chain creates a “soft‑spot” that hydrolyzes slowly, letting the drug act locally before it can be cleared. This makes it a favorite when clinicians need high potency but must limit systemic exposure.

Practical Tips for Clinicians and Patients
- Topical corticosteroid a medication applied to the skin to reduce inflammation should be applied in a thin layer; over‑application does not increase efficacy but raises risk of skin thinning.
- For inhaled mometasone, use a spacer device if the patient has coordination difficulties. This reduces oropharyngeal deposition and the chance of thrush.
- Educate patients to wash hands after each application and to avoid covering treated areas with occlusive dressings unless specifically directed.
- When treating children, limit continuous use to two weeks; schedule “drug holidays” to monitor for growth effects.
- If systemic absorption becomes a concern (e.g., in patients on multiple steroid products), consider measuring morning cortisol levels.
Future Directions & Research
Newer formulations are exploring nano‑emulsion carriers that could further improve cutaneous delivery while reducing the furoate ester’s need for high lipid solvents. Early Phase II trials suggest that a lipid‑nanoparticle version of mometasone may achieve the same skin concentration with half the dose, potentially shrinking the risk of skin atrophy.
Additionally, pharmacogenomic studies are probing how variations in the CYP3A4 enzyme affect systemic clearance. Patients with certain CYP3A4 polymorphisms might experience higher plasma levels after inhaled use, hinting at a future where dose adjustments become genotype‑guided.
Key Takeaways
- Mometasone furoate is a very potent, lipophilic glucocorticoid designed for topical and inhaled use.
- The 17‑alpha‑furoate ester and 16‑alpha‑methyl group boost skin retention and slow metabolic breakdown.
- Its mechanism hinges on high‑affinity binding to the glucocorticoid receptor, suppressing inflammatory gene expression.
- Systemic exposure is low, making it safer for long‑term topical therapy when used correctly.
- Compared with hydrocortisone, betamethasone, and budesonide, mometasone offers a unique balance of potency and safety for both skin and airway inflammation.
How long can I use mometasone cream safely?
For most adults, a 2‑week continuous course is safe. If the condition requires longer treatment, doctors usually recommend intermittent use (e.g., 5 days on, 2 days off) and monitor the skin for signs of thinning.
Can mometasone cause adrenal suppression?
Systemic adrenal suppression is rare when mometasone is applied as directed. It can occur if large body‑surface areas are treated with high‑potency preparations for prolonged periods, so clinicians should check morning cortisol in those cases.
Is it safe to use mometasone during pregnancy?
Topical mometasone is classified as Pregnancy Category C. Small, localized use is generally considered low risk, but pregnant women should always discuss any steroid use with their obstetrician.
What should I do if I develop oral thrush from the inhaler?
Rinse your mouth with water and spit it out after each inhalation. If thrush persists, a short course of an antifungal mouthwash may be prescribed.
How does mometasone compare to hydrocortisone for eczema?
Mometasone is roughly 4‑5 times more potent, so it clears moderate‑to‑severe eczema faster. Hydrocortisone is useful for very mild irritation but often requires longer treatment durations.




Michael Kusold
October 23, 2025 AT 22:27yeah, mometasone's like a stealth ninja for skin inflammation.
Andrew Wilson
October 28, 2025 AT 23:18We really cant just spray any high‑potency steroid on every rash we see, it feels like a moral shortcut that puts patients at risk of skin thinning and systemic side effects.
Kristin Violette
November 3, 2025 AT 00:52From a mechanistic standpoint, mometasone furoate exemplifies the principle of ligand‑directed selectivity: the 17‑alpha‑furoate moiety enhances lipophilicity, thereby increasing partition coefficient (logP ≈ 4.5) and facilitating stratum corneum diffusion.
Concomitantly, the 16‑alpha‑methyl substituent sterically hinders hepatic reductase activity, extending the compound's half‑life relative to non‑esterified analogues.
When the drug reaches the intracellular glucocorticoid receptor (GR), it induces a conformational shift that promotes recruitment of co‑activators such as SRC‑1 and p300, which in turn drive transcription of anti‑inflammatory genes like annexin‑1 and IL‑10.
The GR‑DNA complex also exerts transrepressive effects on NF‑κB and AP‑1, curbing pro‑inflammatory cytokine cascades.
Pharmacokinetically, only a fraction (0.5‑2%) of topically applied mometasone penetrates systemic circulation, a testament to its high epidermal affinity.
Inhaled formulations benefit from particle sizes in the 1‑3 µm range, ensuring deep alveolar deposition while first‑pass hepatic metabolism via CYP3A4 attenuates systemic exposure.
Clinically, this translates to a potency roughly four to five times that of hydrocortisone, making it suitable for moderate‑to‑severe eczema, psoriasis, and allergic rhinitis when used judiciously.
Safety considerations include vigilant monitoring for local atrophy, especially with occlusive dressings, and routine oral rinsing after inhalation to prevent candidiasis.
Pediatric patients warrant particular attention; growth surveillance is advised if therapy exceeds a three‑month continuous course.
Pregnant users should consult obstetric guidance, given the Category C classification, though limited localized use is generally considered low risk.
Comparative data suggest mometasone's systemic bioavailability is lower than that of budesonide and betamethasone dipropionate, thereby offering a favorable risk‑benefit profile.
Emerging nano‑emulsion carriers promise even greater cutaneous bioavailability with reduced carrier lipid burden, potentially halving the effective dose needed for clinical remission.
Pharmacogenomic investigations are also illuminating inter‑individual variability in CYP3A4 activity, which could eventually inform genotype‑guided dosing algorithms.
Overall, mometasone furoate represents a sophisticated balance of chemical modification, receptor pharmacodynamics, and formulation science, making it a cornerstone in contemporary anti‑inflammatory therapy.
Theo Asase
November 8, 2025 AT 02:43Honestly, the pharma giants want us to believe this ‘nano‑emulsion’ breakthrough is pure science, but it’s really just another profit‑driven gimmick to lock patients into brand‑name cycles while the raw molecule stays under patent forever.
Joey Yap
November 13, 2025 AT 04:33It’s fascinating how a tiny structural tweak can so dramatically change a drug’s journey through the body; this really underscores the importance of respecting both the chemistry and the patient’s lived experience.
Lisa Franceschi
November 18, 2025 AT 06:24Esteemed colleagues, I would like to draw your attention to the paramount significance of adhering to prescribed treatment durations, as prolonged exposure-even to a comparatively low‑systemic‑absorption agent such as mometasone furoate-may precipitate adverse cutaneous outcomes.
Suraj 1120
November 23, 2025 AT 08:15While the formal tone is appreciated, the data clearly show that even "low" systemic absorption can accumulate in high‑risk groups, and the guidelines often downplay this risk to keep the drug market-friendly.
Shirley Slaughter
November 28, 2025 AT 10:06Let’s celebrate the fact that mometasone offers such powerful relief for many suffering from chronic eczema-real life stories show dramatic improvements when used responsibly.
Sean Thomas
December 3, 2025 AT 11:56Sure, but remember that the “responsible use” narrative is often a veneer; the same companies that push in‑haler convenience also fund trials that downplay long‑term hormone disruption.
Aimee White
December 8, 2025 AT 13:47Picture this: a molecular maestro wearing a cloak of furoate, dancing across your skin’s barrier like a midnight ballerina, all while whispering sweet anti‑inflammatory lullabies.
Debra Johnson
December 13, 2025 AT 15:38We must, with unflinching resolve, condemn the casual dispersion of high‑potency steroids; such practices betray a contempt for patient safety that cannot be tolerated.
Diane Larson
December 18, 2025 AT 17:29To add a practical note, monitoring morning cortisol levels in patients on extensive mometasone regimens can help detect early adrenal suppression, ensuring timely intervention.
Jeremy Lysinger
December 23, 2025 AT 19:20Stick to the plan, folks-short bursts, proper rinsing, and you’ll keep your skin happy.
Nelson De Pena
December 28, 2025 AT 21:10Remember, consistency and moderation are the twin pillars of effective steroid therapy.