Low-Fiber Diet: When and Why It’s Used, and What You Need to Know
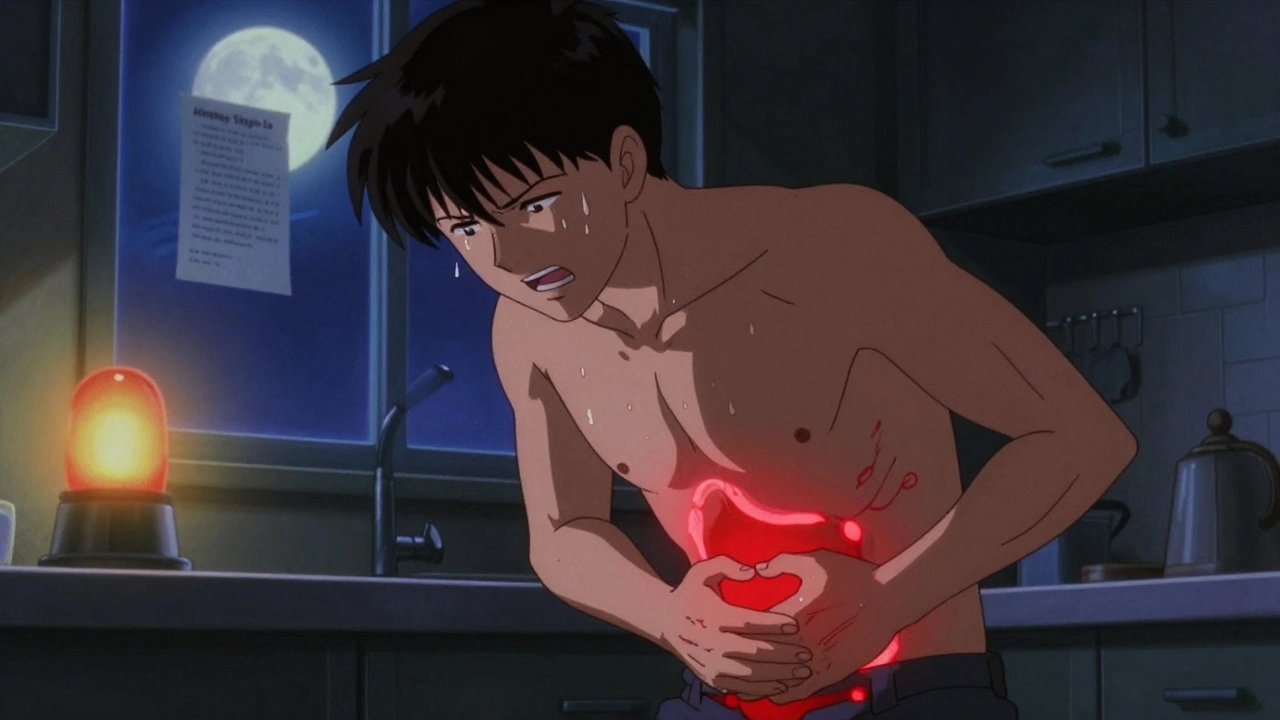
When your digestive system is struggling, a low-fiber diet, a temporary eating plan that limits indigestible plant material to reduce bowel movements and irritation. Also known as low-residue diet, it’s not a weight-loss strategy—it’s a medical tool. Doctors recommend it when your gut needs rest—after surgery, during a flare-up of Crohn’s disease or ulcerative colitis, or before a colonoscopy. It’s not about cutting out healthy foods for the sake of it; it’s about giving your intestines a break so they can heal.
This diet reduces the amount of undigested material passing through your colon, which means fewer bowel movements and less cramping. That’s why it’s often paired with conditions like intestinal inflammation, a condition where the lining of the digestive tract becomes swollen and irritated, often causing pain, diarrhea, and urgency. People with bowel rest, a clinical strategy to minimize digestive activity to allow healing of the gastrointestinal tract. needs may also follow this plan after an obstruction or during radiation therapy. It’s not permanent. Most people switch back to normal fiber levels once symptoms improve, but the timing matters—go too soon, and you risk restarting the pain.
What you eat on this diet is strict. You avoid whole grains, nuts, seeds, raw vegetables, and most fruits with skins. Instead, you get white bread, refined pasta, cooked carrots, peeled apples, and lean meats. Dairy is usually okay unless you’re lactose intolerant. Even smooth peanut butter is allowed, but crunchy? No. The goal is to minimize bulk and movement in your gut. It sounds simple, but people often underestimate how much fiber hides—in fruit juices with pulp, in fortified cereals, even in some protein bars.
It’s not just about food. Medications like laxatives or stool softeners are often paused during this time. And while you might think cutting fiber will cause constipation, that’s not always the goal. Sometimes, the aim is to reduce diarrhea and cramping, not to stop bowel movements entirely. That’s why doctors monitor symptoms closely and adjust the plan. You’re not starving your body—you’re giving your intestines a chance to recover without extra stress.
This approach shows up in real clinical settings—like when someone with peripheral neuropathy, nerve damage causing pain or numbness, often linked to diabetes or chemotherapy. also has IBD and needs to manage both conditions at once. Or when someone recovering from surgery needs to avoid gas and bloating while healing. These aren’t random cases—they’re common reasons why this diet is prescribed.
You’ll find posts here that cover how this diet fits into broader health strategies—like managing medications during digestive flare-ups, what to eat after a colonoscopy, or how to safely reintroduce fiber without triggering symptoms. Some posts even look at how fiber affects drug absorption or interacts with other conditions like liver disease or autoimmune disorders. This isn’t a one-size-fits-all plan. It’s a targeted, time-limited tool used by doctors to help people get through tough periods. And if you’re on it, you deserve clear, practical advice—not vague warnings or misleading hype.
Diverticulitis: Understanding Inflamed Pouches and Modern Treatment Approaches
By Lindsey Smith On 4 Dec, 2025 Comments (12)
Diverticulitis is inflammation of small pouches in the colon, causing severe abdominal pain and fever. Modern treatment avoids antibiotics for mild cases, focuses on fiber, and uses surgery only when necessary. Learn what works now.
View More