Renal Opioid Dosing Calculator
Safe Opioid Selection Guide
Key Safety Notes: Avoid morphine, codeine, meperidine, and propoxyphene in moderate to severe kidney disease (GFR <30 mL/min). Fentanyl, buprenorphine, and methadone are preferred options.
Dosing Calculator
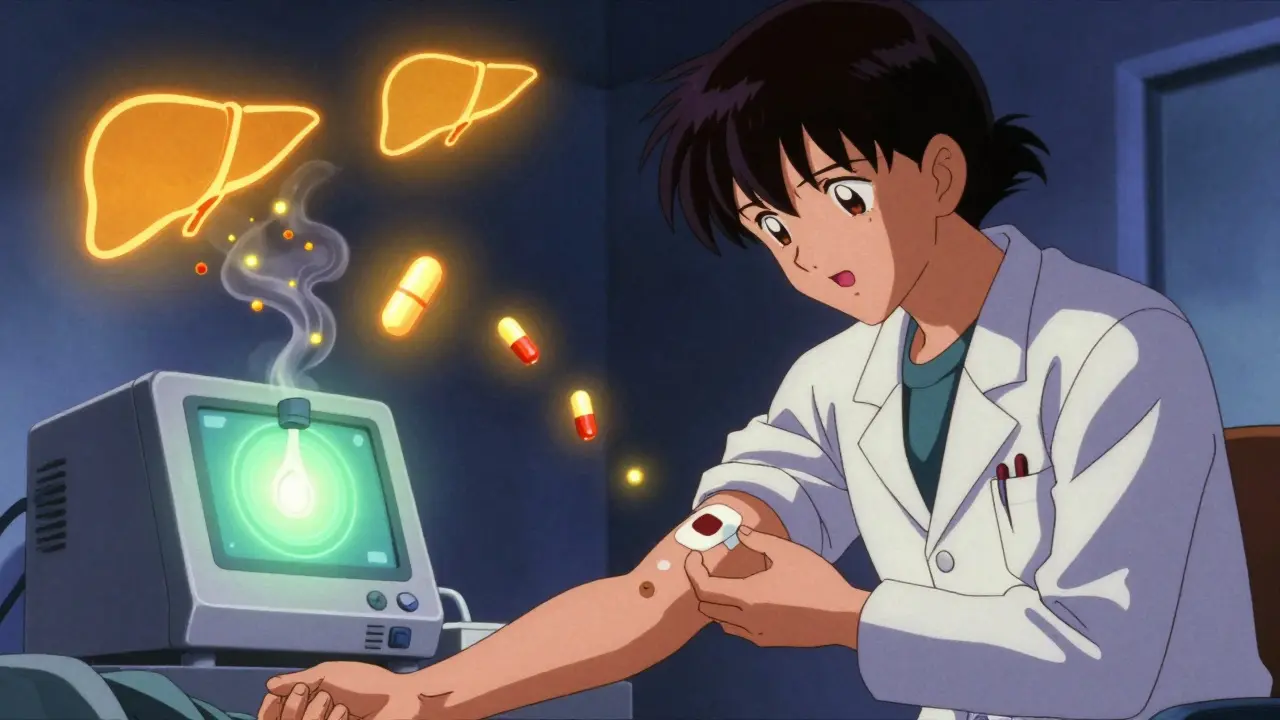
Managing pain in patients with kidney failure is one of the most tricky problems in clinical practice. Opioids are often needed - chronic pain affects up to 85% of people with end-stage renal disease - but many common painkillers can turn dangerous when the kidneys can’t clear them. The wrong choice isn’t just ineffective; it can cause seizures, confusion, or even respiratory arrest. The good news? There are safer options. And with the right dosing, they work.
Why Most Opioids Are Risky in Kidney Failure
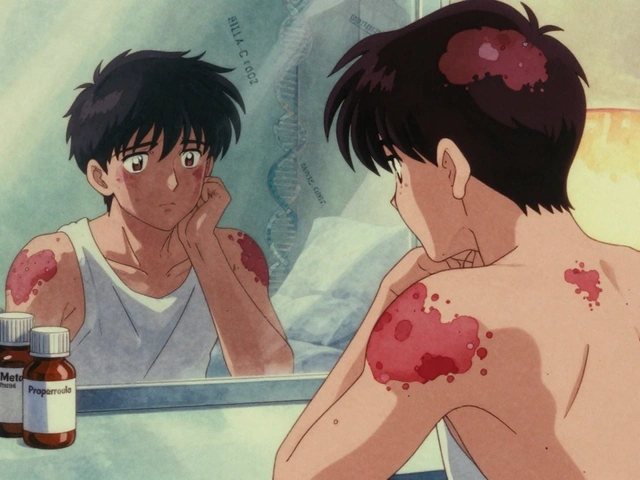
Your kidneys don’t just make urine. They filter out waste, including drug metabolites. When kidney function drops below 30 mL/min (Stage 4 CKD), many opioids and their breakdown products build up. These aren’t just inactive leftovers - some are highly toxic.Morphine, for example, turns into morphine-3-glucuronide. That metabolite doesn’t help with pain. Instead, it causes muscle twitching, delirium, and seizures. Codeine becomes morphine in the liver, then the same toxic metabolites pile up. Meperidine (pethidine) breaks down into normeperidine - a known seizure trigger. In kidney failure, normeperidine levels can cross the danger line even at normal doses.
That’s why the KDIGO guidelines say: avoid morphine, codeine, meperidine, and propoxyphene in moderate to severe kidney disease. These aren’t just warnings - they’re red flags. Yet, studies show nearly half of kidney patients still get these drugs because prescribers aren’t trained on renal dosing.
Safe Opioids for Kidney Patients: What Actually Works
Not all opioids are created equal. Some are mostly broken down by the liver, not the kidneys. That makes them far safer.Fentanyl is one of the top choices. Only 7% of it leaves the body through urine. The rest is processed by the liver. Studies show no dangerous buildup in people with advanced kidney disease. Transdermal patches are ideal - steady release, no peaks and crashes. But never start a fentanyl patch in someone who’s never taken opioids before. The risk of overdose is real.
Buprenorphine is another first-line option. About 30% is cleared by the kidneys, but because it’s so potent and has a long half-life, you don’t need to reduce the dose even in dialysis patients. It’s also less likely to cause breathing problems than other opioids. Watch for QT prolongation on an ECG - it’s rare, but it happens.
Methadone is tricky. It’s metabolized by the liver and doesn’t form toxic metabolites. But it’s long-acting, and its effects can stack up. It also carries a risk of heart rhythm problems. That means ECG monitoring is required when starting or increasing the dose. You need special training to prescribe it - not every doctor is licensed.
Oxycodone has mixed data. About 45% of its metabolites are cleared by the kidneys. Still, clinical experience shows it’s often tolerated if kept under 20 mg per day in advanced CKD. Don’t go higher unless you’re closely watching for sedation or confusion.
Tapentadol is newer. It works on two pain pathways and doesn’t need dose changes in mild-to-moderate kidney disease. But there’s almost no data for people on dialysis. Use it cautiously until more evidence comes in.
Dosing Adjustments Based on Kidney Function
There’s no one-size-fits-all dose. You have to tailor it to the patient’s GFR.- GFR >50 mL/min: Standard doses are usually okay for fentanyl, methadone, and buprenorphine.
- GFR 10-50 mL/min: Cut morphine to 50-75% of normal. Keep fentanyl at 75-100%. Methadone can stay at 100%, but monitor closely.
- GFR <10 mL/min (or on dialysis): Use only 25% of the normal morphine dose. Methadone at 50-75%. Fentanyl at 50%. Buprenorphine? No change needed.
Start low. Go slow. Wait 48 hours before increasing the dose. Pain doesn’t disappear overnight - and neither should the risk of overdose.
What About Dialysis Patients?
Dialysis removes some drugs, but not all. And it doesn’t follow a predictable pattern.Fentanyl? Avoid during dialysis sessions. It’s highly protein-bound and doesn’t get cleared well by the machine. You might think the patient is getting relief, but the drug stays in their system.
Buprenorphine? Safe during dialysis. No dose adjustment needed. That’s why many nephrology teams now prefer it for patients on hemodialysis.
Hydromorphone? Avoid. Its metabolite builds up dramatically in non-dialysis patients and still causes neurotoxicity even after dialysis. The risk is 37% higher than in dialyzed patients.
For patients on dialysis, the best strategy is to use a drug that doesn’t rely on kidney clearance - and stick with it consistently. Switching between opioids after each dialysis session is a recipe for error.
Non-Opioid Options and Complementary Therapies
Opioids shouldn’t be the only tool. In fact, the best outcomes come from combining them with safer alternatives.Gabapentin and pregabalin are often used for nerve pain. But they’re cleared by the kidneys. In CKD, gabapentin must be cut to 200-700 mg once daily. Pregabalin needs even lower doses and longer intervals. Too much can cause dizziness, falls, or confusion.
Tricyclic antidepressants like nortriptyline can help with chronic pain. But they’re risky in kidney patients. When electrolytes shift - which they often do - these drugs can trigger dangerous heart rhythms. Serum levels above 100 ng/mL triple the risk of cardiac events.
NSAIDs like ibuprofen? Avoid. They reduce kidney blood flow and can make kidney function worse.
Consider non-drug options: physical therapy, nerve blocks, acupuncture, or cognitive behavioral therapy. These aren’t just add-ons - they’re essential parts of a complete plan.

Constipation: The Silent Side Effect
Up to 80% of kidney patients on opioids get constipated. It’s not just uncomfortable - it can lead to bowel obstruction, especially in older adults.Standard laxatives often don’t work. That’s where naldemedine comes in. It’s a peripherally-acting opioid blocker - it doesn’t cross the blood-brain barrier, so it doesn’t undo pain relief. And unlike other options, it doesn’t need any dose adjustment in kidney failure or dialysis. One 0.2 mg pill daily is enough.
Don’t wait for constipation to become severe. Start a bowel regimen from day one.
Why So Many Patients Still Get the Wrong Drugs
Despite clear guidelines, under-treatment is common. In dialysis centers, up to 64% of patients with chronic pain get no opioid therapy at all. Why?Many drug labels don’t mention kidney dosing. A 2019 FDA review found 68% of opioid package inserts lack renal guidance. Doctors rely on outdated training or guesswork. Even in hospitals, electronic systems rarely flag unsafe prescriptions for kidney patients.
Integrated health systems like Kaiser Permanente have fixed this by building alerts into their EHRs. When a doctor tries to prescribe morphine to a patient with GFR <15, the system blocks it and suggests fentanyl instead. Result? A 47% drop in unsafe prescriptions between 2018 and 2022.
The Future: Personalized Pain Care
Research is moving fast. The NIDDK’s PAIN-CKD study is tracking 1,200 patients over five years to see which opioids work best long-term. Early data suggests genetics matter. People who are CYP2D6 poor metabolizers are over three times more likely to have toxic reactions to morphine.Future guidelines will likely include genetic testing. For now, stick to the safest bets: fentanyl patches, buprenorphine, and methadone - with careful monitoring.
The goal isn’t just to relieve pain. It’s to do it without harming the patient further. In kidney failure, that means choosing wisely - and never assuming a standard dose is safe.
Which opioids are safest for patients with kidney failure?
Fentanyl and buprenorphine are the safest choices. Fentanyl is mostly metabolized by the liver, with only 7% excreted by the kidneys. Buprenorphine has low renal clearance and doesn’t require dose adjustment in advanced kidney disease or dialysis. Methadone is also an option but requires ECG monitoring due to QT prolongation risk. Avoid morphine, codeine, meperidine, and hydromorphone - their metabolites accumulate and cause neurotoxicity.
Can you use morphine in kidney disease?
No - morphine is contraindicated in moderate to severe kidney disease (GFR <50 mL/min). Its metabolite, morphine-3-glucuronide, builds up and causes seizures, myoclonus, and confusion. Even if you reduce the dose, the risk remains. Stick to safer alternatives like fentanyl or buprenorphine.
How should opioid doses be adjusted for CKD patients?
Start at 50% of the standard dose for advanced CKD (GFR <15 mL/min). For GFR 10-50 mL/min, reduce morphine to 50-75%, keep fentanyl at 75-100%, and methadone at 100%. For GFR <10 mL/min, use only 25% of the morphine dose, 50-75% of methadone, and 50% of fentanyl. Always extend dosing intervals by 50-100%. Never increase the dose faster than every 48 hours.
Is buprenorphine safe during hemodialysis?
Yes. Buprenorphine is safe to use during hemodialysis without dose adjustment. Only about 30% of it is cleared by the kidneys, and its metabolites are not toxic. It’s one of the few opioids recommended for dialysis patients by nephrology guidelines.
What’s the best treatment for opioid-induced constipation in kidney patients?
Naldemedine is the preferred choice. Unlike other peripherally-acting opioid blockers, it doesn’t require dose adjustment in kidney failure or dialysis. The standard dose is 0.2 mg once daily. It relieves constipation without reducing pain control or causing withdrawal.
Why do some doctors still prescribe morphine to kidney patients?
Many opioid labels don’t include renal dosing instructions - 68% of them, according to an FDA review. Doctors may rely on outdated training or assume a lower dose is safe. Electronic health record systems often don’t flag unsafe prescriptions. This gap leads to continued inappropriate use despite clear guidelines from KDIGO and the American Academy of Family Physicians.
Are there any non-opioid alternatives for pain in kidney disease?
Yes. Gabapentin and pregabalin can help with nerve pain but require dose reductions. Tricyclic antidepressants like nortriptyline carry heart risks. NSAIDs should be avoided as they harm kidney function. Non-drug options - physical therapy, acupuncture, cognitive behavioral therapy - are safe and effective. A multimodal approach reduces opioid needs and improves outcomes.





Angel Tiestos lopez
January 13, 2026 AT 19:55Alan Lin
January 14, 2026 AT 19:28Priyanka Kumari
January 15, 2026 AT 21:36Avneet Singh
January 17, 2026 AT 05:40Nelly Oruko
January 18, 2026 AT 07:51vishnu priyanka
January 19, 2026 AT 04:18Lethabo Phalafala
January 20, 2026 AT 06:47Lance Nickie
January 21, 2026 AT 20:23Milla Masliy
January 23, 2026 AT 19:50Damario Brown
January 23, 2026 AT 20:30sam abas
January 24, 2026 AT 10:02John Pope
January 25, 2026 AT 09:20Clay .Haeber
January 26, 2026 AT 09:16Adam Vella
January 28, 2026 AT 08:59Trevor Whipple
January 29, 2026 AT 17:51