Psoriasis Risk Assessment Tool
Assess Your Risk
Answer these questions to determine your likelihood of psoriasis flare when taking beta-blockers.
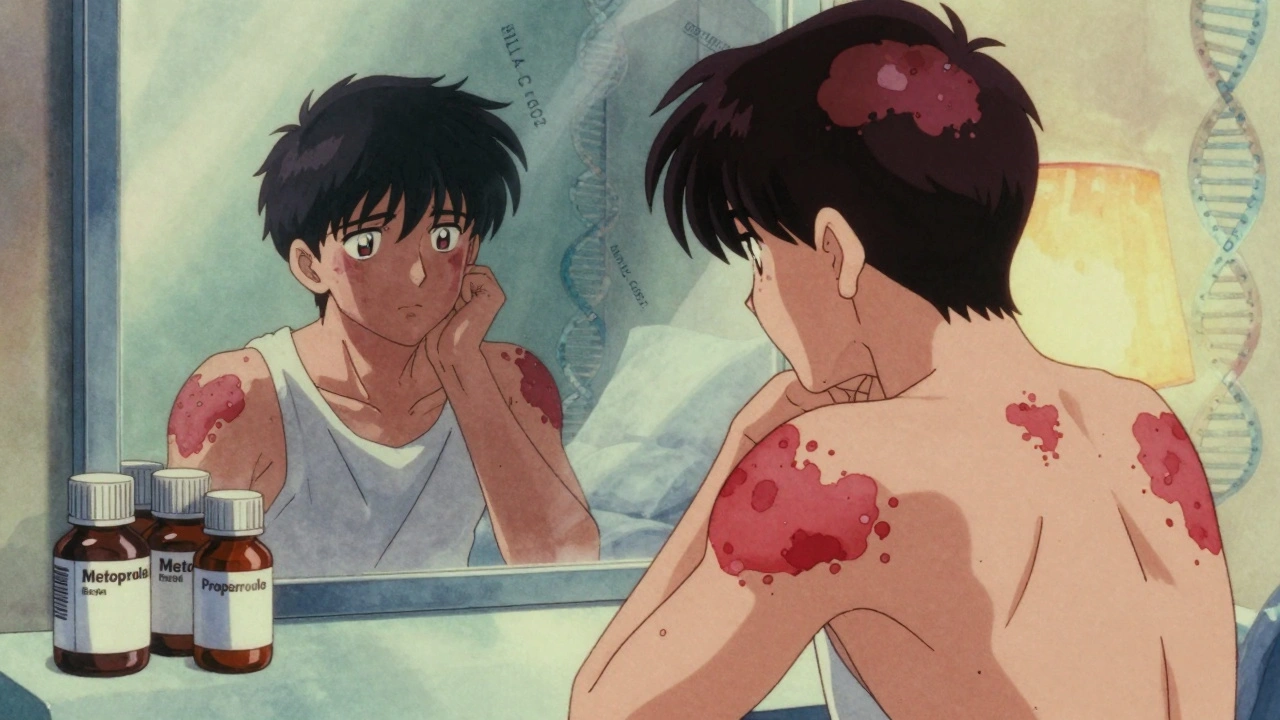
If you have psoriasis and were recently prescribed a beta-blocker for high blood pressure or heart issues, your skin flare might not be bad luck-it could be the medication. Around 20% of people with existing psoriasis see their symptoms get worse after starting drugs like metoprolol, propranolol, or atenolol. Even more troubling, some people develop psoriasis for the first time after taking these common heart meds. The connection isn’t always obvious, because the flare-up can show up months after you start the pill-sometimes as late as 18 months later. That delay makes it easy to miss the link unless you’re looking for it.
How Beta-Blockers Trigger Psoriasis Flares
Beta-blockers work by slowing your heart rate and lowering blood pressure. They do this by blocking adrenaline from binding to beta receptors in your heart and blood vessels. But those same receptors are also found in your skin. When beta-blockers interfere with them there, they disrupt how skin cells grow and how inflammation is controlled.
Research shows these drugs lower levels of cyclic AMP (cAMP), a chemical that helps keep skin cells from multiplying too fast and keeps immune cells in check. When cAMP drops, skin cells start piling up, forming those thick, scaly patches. At the same time, immune cells in the skin get overactive, causing redness, itching, and swelling. This isn’t just theory-it’s been seen in biopsies of patients who developed psoriasis after starting beta-blockers.
Not all beta-blockers carry the same risk. Propranolol and metoprolol are the most commonly reported offenders. Even eye drops containing timolol-for glaucoma-can trigger flares because some of the drug gets absorbed into your bloodstream through your eye. Pindolol has been linked to rare but severe cases, like turning regular plaque psoriasis into pustular psoriasis, where pus-filled bumps appear across large areas of skin.
Who’s Most at Risk?
It’s not everyone. Some people take beta-blockers for years with no skin issues. Others see a flare within weeks. What makes the difference? Genetics may play a role. Early results from a 2024 study at Johns Hopkins and Mayo Clinic suggest people with the HLA-C*06:02 gene variant are more likely to develop psoriasis after taking beta-blockers. This gene is already known to increase risk for plaque psoriasis, so having it might make your skin more sensitive to drug triggers.
People with moderate to severe psoriasis before starting beta-blockers are also more likely to have a major flare. One patient on Reddit shared that after six months on metoprolol, their psoriasis went from covering 5% of their body to 30%. Another user on MyPsoriasisTeam said they’d been stable for years-until they started a beta-blocker for anxiety-related palpitations. Within three months, their elbows and scalp were covered in new plaques.
Even if you don’t have psoriasis yet, you might still be at risk. About 12% of people who develop psoriasis for the first time report starting a beta-blocker shortly before the first flare. That’s why dermatologists now routinely ask: “Are you on any heart meds?” when someone comes in with unexplained skin changes.

What to Do If You Suspect a Medication Trigger
Don’t stop your beta-blocker on your own. These drugs are often critical for preventing heart attacks, strokes, or dangerous heart rhythms. Stopping suddenly can be life-threatening.
Instead, talk to both your dermatologist and cardiologist. Bring a photo of your skin before and after the flare, and note exactly when you started the medication. If your doctor suspects the beta-blocker is the cause, they may suggest switching to a different type of blood pressure medication.
Good alternatives include:
- Calcium channel blockers like amlodipine
- ARBs like losartan or valsartan
- Some diuretics (though thiazides can also trigger psoriasis in rare cases)
ACE inhibitors (like lisinopril) are sometimes suggested-but they’re not risk-free. They’ve also been linked to psoriasis flares in some studies, so they’re not always the answer.
Once you switch, it can take weeks to months for your skin to improve. Some patients see relief in four weeks. Others need three to six months. Patience is key, but improvement after stopping the drug is the clearest sign it was the trigger.
Managing the Flare While Switching Meds
In the meantime, your dermatologist will likely recommend treatments to calm your skin:
- Topical corticosteroids (like hydrocortisone or clobetasol)
- Vitamin D analogues (calcipotriene) to slow skin cell growth
- Moisturizers with ceramides or colloidal oatmeal to repair the skin barrier
- Phototherapy (UVB light treatment), especially if the flare is widespread
- For severe cases: biologics like adalimumab or ustekinumab
These treatments won’t fix the root cause-the medication-but they can give you relief while you work on switching safely.
Why This Isn’t Always Clear in the Literature
You might read conflicting studies. One 2010 paper said beta-blocker use isn’t a major risk for psoriasis. Another says it’s one of the top drug triggers. Why the confusion?
Part of it is study design. Some look at large populations and miss rare or delayed reactions. Others rely on patient recall, which can be inaccurate. Plus, many people take multiple medications at once-making it hard to isolate one culprit.
But real-world evidence is growing stronger. A 2023 survey of 187 psoriasis patients found 37% on beta-blockers reported worsening skin, compared to only 12% on other blood pressure drugs. That’s a big difference. And when doctors remove the beta-blocker and see improvement, it’s hard to ignore.
Practolol, an older beta-blocker, was pulled off the market in the 1980s because so many patients developed severe skin reactions. That’s why today’s versions are more selective-but they’re not harmless.
What You Can Do Now
If you’re on a beta-blocker and have psoriasis:
- Track your skin changes. Take photos monthly.
- Don’t assume new patches are stress or weather-related.
- Ask your doctor: “Could this medication be making my psoriasis worse?”
- Bring up the topic even if you’ve been on the drug for months or years.
If you’re starting a beta-blocker and have a history of psoriasis:
- Let your doctor know upfront.
- Ask if there’s an alternative with lower skin risk.
- Schedule a skin check 3-6 months after starting the drug.
The bottom line? Beta-blockers save lives-but they can also make psoriasis worse. That doesn’t mean you shouldn’t take them. It means you need to be informed. With the right conversation and a smart switch, you can protect both your heart and your skin.
Can beta-blockers cause psoriasis in people who never had it before?
Yes, though it’s less common than worsening existing psoriasis. Studies and patient reports show that some people develop their first psoriasis flare weeks to months after starting a beta-blocker. The risk is higher if you have a family history of psoriasis or carry the HLA-C*06:02 gene. While not everyone will react, it’s a recognized side effect that doctors should consider when evaluating new skin conditions.
Which beta-blockers are most likely to trigger psoriasis flares?
Propranolol, metoprolol, and atenolol are the most commonly reported. Pindolol has been linked to severe cases, including pustular psoriasis. Even topical timolol eye drops for glaucoma can cause flares due to systemic absorption. Not all beta-blockers carry the same risk, but if one triggers a flare, others likely will too-so switching within the same class isn’t usually recommended.
How long after starting a beta-blocker does psoriasis usually flare up?
There’s no set timeline. Flares can appear as early as one month after starting the drug, but most often they show up between three and 12 months. Some patients report changes even after 18 months. This delay is why many people don’t connect their skin flare to the medication without help from a doctor.
Should I stop taking my beta-blocker if my psoriasis gets worse?
No. Stopping suddenly can cause dangerous spikes in blood pressure, heart rate, or even heart attack. Instead, talk to your doctor. They can help you switch to a safer alternative, like a calcium channel blocker or ARB, while monitoring your heart health. Never adjust your dose or stop without medical guidance.
Are there blood pressure meds that are safer for people with psoriasis?
Yes. Calcium channel blockers like amlodipine and ARBs like losartan are generally considered safer options. Diuretics and ACE inhibitors carry some risk too, so they’re not always ideal. Your doctor will choose based on your heart health, other conditions, and how well your skin responds. The goal is to find a medication that controls your blood pressure without triggering your skin.






ian septian
December 8, 2025 AT 05:38Been on metoprolol for 3 years. My psoriasis went from mild to full-on scalp-to-knee nightmare at 14 months. Doctor didn’t even blink until I showed him the timeline. Now I’m on amlodipine and my skin’s finally chillin’. 🙌
Chris Marel
December 9, 2025 AT 23:40This is so important. I didn’t realize meds could do this. My cousin started beta-blockers after her heart palpitations and suddenly her elbows looked like cracked pottery. She’s been scared to say anything because she’s afraid to stop the heart med. Thank you for putting this out there.
Elliot Barrett
December 10, 2025 AT 20:55Wow. Another ‘meds cause side effects’ article. Newsflash: everything causes side effects. You want to live? Take the pill. Your skin will survive. Stop being dramatic.
Ajit Kumar Singh
December 12, 2025 AT 06:11Bro I had psoriasis since 18 now 32 and on propranolol for anxiety and my skin was fine until last year when I got a big flare up I thought it was stress but then I read this and holy shit I switched to losartan and boom 70% better in 6 weeks no joke I’m not lying
Maria Elisha
December 12, 2025 AT 11:57So like… I’m on metoprolol and I’ve had a few flares. I just thought it was winter or my laundry detergent. So I’m supposed to just switch meds? What if my heart goes haywire? This is wild.
Lisa Whitesel
December 13, 2025 AT 06:25People are so lazy they blame pills instead of their diet or lack of sleep. Psoriasis is a lifestyle failure. If you washed your hands more and stopped eating sugar none of this would happen. Beta-blockers aren’t the enemy. You are.
Larry Lieberman
December 14, 2025 AT 16:52Just got my bloodwork back and my cAMP levels are low 😱 I’ve been on atenolol for 8 months and my elbows are on fire. I’m scheduling an appt with my derm tomorrow. Thanks for the heads up! 🙏
Sabrina Thurn
December 15, 2025 AT 22:26From a clinical perspective, the mechanism is well-documented: beta-adrenergic antagonism reduces intracellular cAMP in keratinocytes, leading to dysregulated proliferation and Th17-driven inflammation. The HLA-C*06:02 association is particularly significant-it’s a pharmacogenomic red flag. Switching to an ARB or CCB is the gold standard, but monitor renal function and electrolytes post-switch. Also, UVB phototherapy has Level 1 evidence for drug-induced flares.
Simran Chettiar
December 17, 2025 AT 04:31It is not merely the medication that is the issue, dear readers, but the metaphysical dissonance between the modern medical paradigm and the ancient wisdom of the body. The skin, as the mirror of the soul, reflects not only the chemical imbalance but the spiritual neglect of our times. Beta-blockers, in their mechanistic reductionism, suppress the vital pulse, and thus the skin, in its sacred autonomy, rebels. One must ask: is healing a matter of substitution, or of surrender to the rhythm of nature?
Richard Eite
December 17, 2025 AT 19:48USA medical system is broken. You get a pill for everything. In Russia we use cold showers and vodka. Skin clears up in a week. Stop whining. Take your meds. Stop being weak.
Katherine Chan
December 18, 2025 AT 07:19You got this! I know it’s scary but talking to your docs is the bravest thing you can do. My friend switched from metoprolol to losartan and now she’s hiking again without itching. You’re not alone 💪❤️
Shubham Mathur
December 19, 2025 AT 22:13Bro I’m from Delhi and my uncle was on propranolol for 10 years and his psoriasis was under control until he moved to the US and switched to metoprolol and boom full body flare I told him to switch back to propranolol and he did and it got better so maybe its not the class its the specific drug
Ronald Ezamaru
December 21, 2025 AT 15:59I’ve been a cardiologist for 22 years. I’ve seen this pattern dozens of times. Patients come in with flares, we ask about meds, and 80% of the time it’s a beta-blocker. We’ve started asking proactively. The key is not fear-it’s awareness. Don’t panic. But do speak up.
Andrea Petrov
December 23, 2025 AT 07:22Did you know the FDA has known about this since 1998 but buried the data because Big Pharma pays them? I’ve got screenshots. Timolol eye drops are part of a global mind control scheme to weaken the immune system. Your skin is just the first sign. They want you dependent on biologics. Wake up.
Suzanne Johnston
December 25, 2025 AT 01:04There’s a deeper truth here: modern medicine treats symptoms without honoring the body’s intelligence. Beta-blockers silence the heart’s rhythm, and the skin, as the body’s largest organ, becomes the messenger. Perhaps the flare isn’t a side effect-it’s a call to reevaluate our relationship with pharmaceutical control. Not to reject medicine, but to seek harmony within it.