When you get an injection, you expect it to be safe. You don’t think about the cleanroom, the air filters, or the 30-minute heat cycle that sterilized the vial. But behind every safe injectable drug - whether it’s insulin, chemotherapy, or a COVID vaccine - is a highly controlled, tightly regulated manufacturing process. One mistake, one contaminated batch, and people can die. That’s why sterile manufacturing for injectables has some of the strictest requirements in all of pharmaceutical production.
Why Injectables Are Different
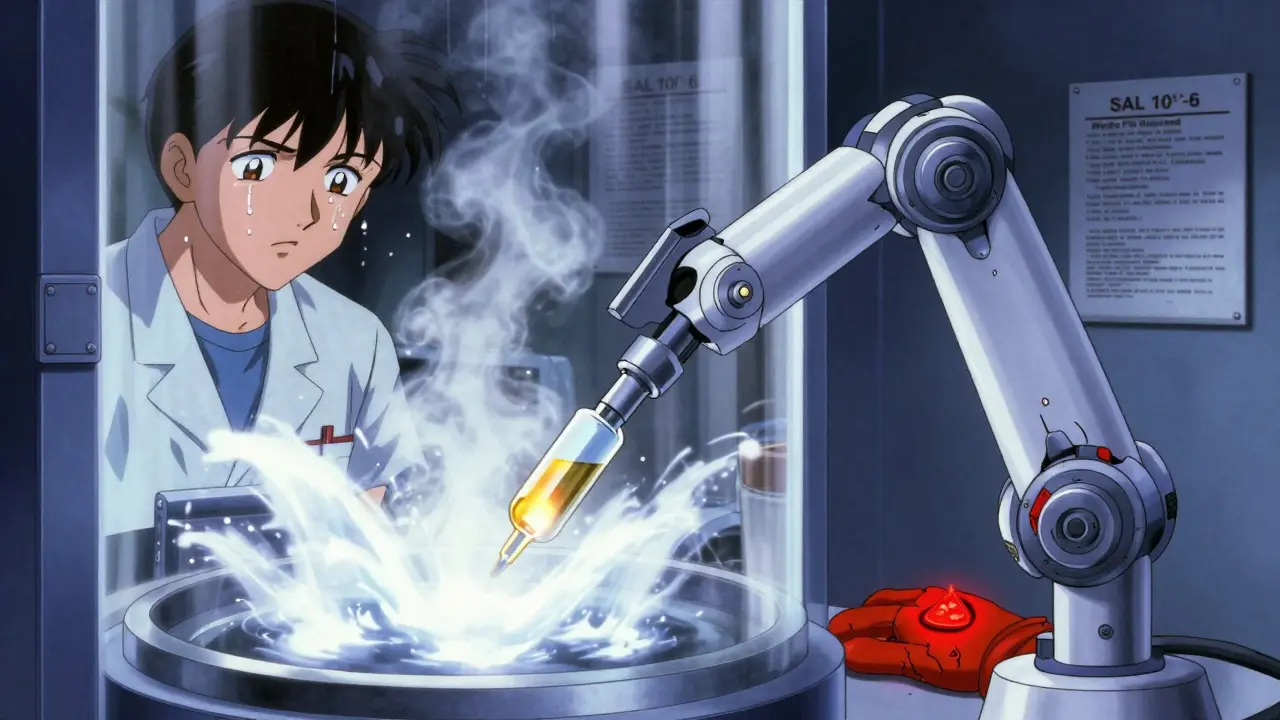
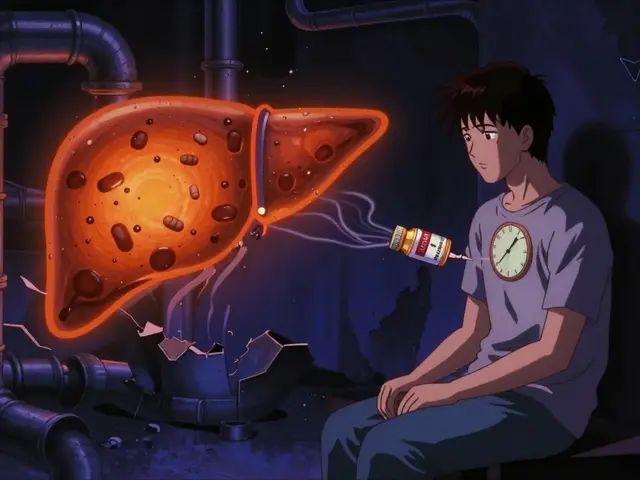
Oral pills pass through your stomach and liver before entering your bloodstream. Your body has defenses. Injectables? They go straight in. No filters. No barriers. That means even a single bacterium or endotoxin can trigger sepsis, organ failure, or death. The 2012 fungal meningitis outbreak linked to contaminated steroid injections killed 64 people and sickened over 750. The CDC report called it one of the worst public health disasters in U.S. history. It wasn’t a lab error. It was a failure in sterile manufacturing.That’s why regulators treat injectables differently. The goal isn’t just "clean." It’s sterile. The World Health Organization sets the bar at a Sterility Assurance Level (SAL) of 10^-6. That means, statistically, only one in a million vials could be contaminated. No other drug form has this requirement.
Two Ways to Get There: Terminal vs. Aseptic
There are only two approved paths to sterile injectables: terminal sterilization and aseptic processing. Each has trade-offs.Terminal sterilization is the simpler method. You fill the vial, seal it, then blast it with steam at 121°C for 15-20 minutes. Or you hit it with gamma radiation. This kills everything. It’s reliable. It’s validated. And the FDA prefers it - for good reason. But here’s the catch: 60-70% of modern injectables can’t take this heat. Biologics like monoclonal antibodies, vaccines, and protein therapies break down under high temperatures. So for those, you need aseptic processing.
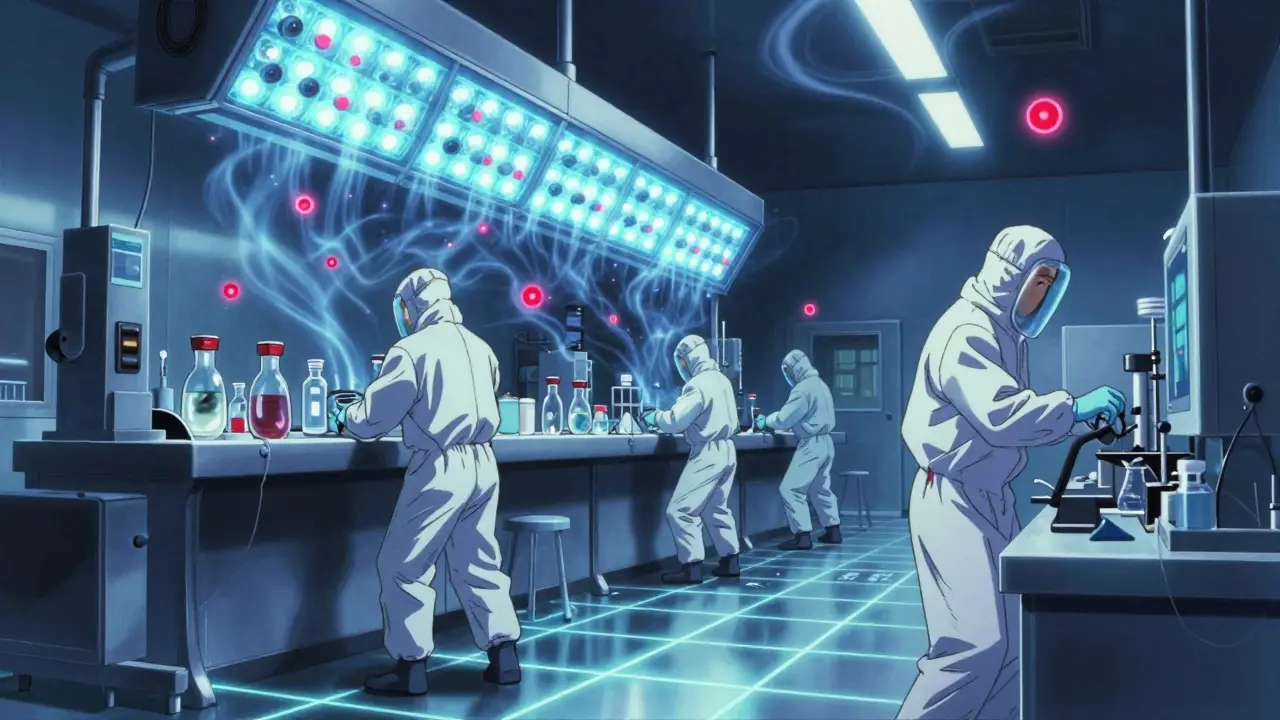
Aseptic processing is where things get intense. No heat. No radiation. Instead, every step happens in a cleanroom so controlled it’s almost sci-fi. Workers wear full gowns, masks, hoods, and double gloves. Air is filtered through HEPA systems. Rooms are kept at 20-24°C with 45-55% humidity. Pressure differences between rooms are maintained at 10-15 Pascals - just enough to keep dirty air from creeping in.
The heart of the process is the ISO 5 zone - the filling area. It must have fewer than 3,520 particles per cubic meter that are 0.5 microns or larger. That’s tighter than a hospital operating room. To monitor it, you need real-time particle counters and air samplers. If you catch more than 1 colony-forming unit (CFU) per cubic meter of air, you’ve hit your alert level. Five CFUs? That’s an action level. Production stops. Investigation starts.
The Hidden Rules: Water, Containers, and Pyrogens
Sterility isn’t just about air. It’s about every material that touches the product.Water for Injection (WFI) isn’t just purified water. It’s distilled, deionized, and filtered to remove endotoxins. The limit? Less than 0.25 Endotoxin Units (EU) per milliliter. Anything above that and you risk fever, shock, or death.
Containers - vials, syringes, ampoules - must be depyrogenated. That means baking them at 250°C for 30 minutes. Or using a validated equivalent. Why? Because even if you sterilize the liquid, a single endotoxin left on the glass can trigger a dangerous immune response.
Media fill simulations are mandatory. Every six months, manufacturers run a full production cycle using growth media instead of the real drug. If even one vial grows bacteria? That’s a failure. The FDA says you need to simulate 5,000 to 10,000 units per test. And if your failure rate hits 0.1%, your process isn’t stable. You fix it - or shut down.
Costs, Risks, and Real-World Failures
Sterile manufacturing isn’t cheap. A small-scale facility costs $50 million to $100 million to build. Annual operating costs? Millions more.Terminal sterilization runs about $50,000 per batch. Aseptic processing? $120,000 to $150,000. Why the gap? Cleanrooms, monitoring systems, training, and validation. But the bigger cost is failure.
A 2022 BioPhorum survey found that 68% of sterile manufacturing sites had at least one sterility test failure in a year. Each failure cost an average of $1.2 million. One company lost $450,000 in a single batch because a glove tear in their RABS system introduced contamination. Another spent $2.5 million on automated visual inspection just to drop defects from 0.2% to 0.05%.
Inspections tell the story. In 2022, 68% of FDA deficiencies in sterile facilities were tied to aseptic technique. Only 12% involved terminal sterilization. That tells you where the real risk lies - not in the heat, but in human hands.

Technology Is Changing the Game
The old way - people in cleanrooms moving vials by hand - is fading. New facilities use isolators: sealed, robotic systems where operators manipulate products through gloves built into the wall. Isolators cut contamination risk by 100 to 1,000 times compared to traditional cleanrooms, according to Dr. James Akers. But they cost 40% more to install.Some companies stick with RABS (Restricted Access Barrier Systems). They’re cheaper. They’re flexible. And if operated perfectly, they can match isolators. But one slip - a glove tear, a door left open, a technician moving too fast - and you’re back in danger.
Continuous monitoring is now required under EU GMP Annex 1 (2022). No more weekly checks. You need sensors running 24/7, logging every particle, every microbe. And it’s working. Lonza’s Swiss facility cut deviations by 45% after installing real-time monitoring. Batch release time dropped 30%.
Automation is rising. Robotic filling systems are growing fast. By 2027, McKinsey predicts a 40% increase. Faster. More accurate. Fewer human errors.
What’s Next? Regulation, Growth, and Global Pressure
The global sterile injectables market hit $225 billion in 2023. Biologics are driving most of that growth. Monoclonal antibodies alone make up 32% of new drug approvals.Regulators are catching up. The FDA’s 2024-2026 plan includes AI-powered inspections and data analytics to catch problems before they happen. The EU’s Annex 1 update forced companies to adopt Quality Risk Management - a formal way to predict and prevent failures.
But the biggest challenge? Global supply chains. China has over 1,200 sterile manufacturing sites. Only 28 passed FDA inspections in 2022. India’s growing fast too. But compliance isn’t automatic. It’s expensive. And it’s not just about equipment - it’s about culture, training, and discipline.
By 2028, the market will hit $350 billion. But only those who invest in real sterility - not just paperwork - will survive.
What’s the difference between sterile and cleanroom manufacturing?
Cleanroom manufacturing reduces contamination - it doesn’t eliminate it. Sterile manufacturing ensures zero viable microorganisms in the final product. Cleanrooms are part of sterile manufacturing, but sterile manufacturing includes sterilized materials, validated processes, media fills, and environmental monitoring. A cleanroom alone doesn’t make a product sterile.
Why can’t all injectables be terminally sterilized?
Many injectables - especially biologics like monoclonal antibodies, vaccines, and protein-based drugs - are sensitive to heat and radiation. Steam sterilization at 121°C or gamma radiation can break their molecular structure, making them ineffective or even harmful. For these products, aseptic processing is the only option.
What’s a media fill simulation?
A media fill simulation is a mock production run where you fill vials with nutrient-rich broth instead of the actual drug. After incubation, you check for bacterial growth. If any vial grows microbes, your process failed. It’s the gold standard test for aseptic technique. The FDA requires at least 5,000 units per simulation, done twice a year.
How often do sterile manufacturing facilities fail inspections?
In 2022, the FDA cited 1,872 deficiencies in sterile manufacturing facilities - up from 1,245 in 2019. Over two-thirds of those were related to aseptic technique failures, environmental monitoring gaps, or inadequate personnel training. It’s not rare. It’s common. That’s why every facility must treat sterility as a daily discipline, not a checklist.
Is aseptic processing safer than terminal sterilization?
It’s not about which is safer - it’s about which is appropriate. Terminal sterilization has a lower risk of contamination because it kills everything after packaging. Aseptic processing relies on flawless control at every step. But with modern isolators, continuous monitoring, and rigorous training, aseptic processing can be just as safe - if not safer for sensitive drugs. The real issue is consistency. Human error is the biggest threat in aseptic areas.





Tasha Lake
February 8, 2026 AT 11:44Terminal sterilization is elegant in its simplicity-steam at 121°C for 15 minutes, validate, move on. But the real magic? Aseptic processing. You’re not just controlling the environment-you’re engineering a microbial no-fly zone. ISO 5 zones, HEPA filters, RABS, gowning protocols that look like NASA prep-every variable is locked down. And yet, human error still slips through. That’s why media fills aren’t just compliance-they’re a daily war game. One CFU in a 10,000-unit batch? That’s not a failure. That’s a wake-up call.
And don’t even get me started on endotoxins. You can sterilize the liquid, but if your vial’s been sitting on a bench for 47 minutes without a depyrogenation certificate? You’re just decorating a bomb.
The FDA’s 2024 AI inspection push? Long overdue. Real-time particle counters, machine learning anomaly detection-this isn’t sci-fi anymore. It’s Tuesday morning at Lonza.
Sam Dickison
February 9, 2026 AT 13:53Yeah but let’s be real-most of these cleanrooms are just fancy air purifiers with panic buttons. I’ve seen facilities where the gowning room looks like a spa day and the filling line is one sneeze away from a recall. The $150k/batch cost? That’s the price of paranoia. And honestly? Half of it’s just documentation theater. You can’t audit a glove tear. You can only hope nobody was having a bad day.
Terminal’s the answer for 60% of stuff. Why are we pretending aseptic is the future? It’s the necessary evil. The rest is just PR.
Chelsea Cook
February 10, 2026 AT 16:06So let me get this straight-we spend $100M to build a room where people wear full hazmat suits to pour liquid into vials… and still, someone’s glove rips and 450k goes down the drain? Like. What are we even doing here? This isn’t manufacturing. It’s a high-stakes game of Jenga where the blocks are people’s lives.
And don’t even get me started on ‘media fills.’ You mean we fake-run the whole thing with broth just to see if our ‘perfect’ process secretly hates us? That’s not QA. That’s therapy for engineers.
John Sonnenberg
February 11, 2026 AT 00:05The real issue isn’t the technology-it’s the culture. You can install isolators, you can deploy AI monitoring, you can have 24/7 particle counters-but if your operator thinks ‘5 CFUs’ is just a suggestion, you’re already dead. The FDA deficiencies aren’t about equipment. They’re about attitude. And attitude doesn’t come from SOPs. It comes from leadership that actually cares. And that’s rare.
Jessica Klaar
February 12, 2026 AT 00:20I’ve worked in three sterile facilities across three continents. The U.S. has the most rules. Europe has the most rigor. India has the most hustle. China? They’ve got the most volume-and the most quiet failures.
But here’s what no one talks about: the technicians. The ones who show up at 4 a.m., scrub for 20 minutes, and fill 12,000 vials without a single error. They’re not robots. They’re human. And when they’re overworked, undertrained, or ignored? That’s when the CFUs creep in.
Invest in people. Not just sensors. Not just isolators. People.
Brett Pouser
February 13, 2026 AT 06:40My cousin works in pharma in Mumbai. He told me their facility runs 18-hour shifts, 7 days a week. They use RABS because isolators cost too much. They do media fills quarterly-not biannually. They’ve never failed an inspection… because they don’t report the near-misses.
Global supply chains aren’t just about cost. They’re about trust. And right now, we’re trusting a lot of places that aren’t ready. The FDA can’t inspect everywhere. So who’s watching? The answer? No one. Until the next outbreak.
PAUL MCQUEEN
February 14, 2026 AT 08:05Let’s not pretend this is rocket science. You want sterile? Freeze-dry it. Or use lyophilization. Or just don’t inject it. Why are we forcing biology into a metal vial like it’s a soda can? Most of these biologics are just fancy proteins that fall apart if you look at them funny. Maybe the real solution is not to inject them at all. Maybe we should just… not.
glenn mendoza
February 15, 2026 AT 09:28While I appreciate the technical depth of this post, I would like to offer a perspective grounded in human dignity and operational humility. The sterile manufacturing process is not merely a sequence of engineering controls-it is a covenant between science and society. Every vial, every glove, every air sample represents a promise: that no one will suffer because we cut corners.
When we speak of $1.2 million failures, we must remember that behind each number is a patient who may have been denied a life-saving therapy. The cost of sterility is not measured in dollars, but in trust. And trust, once broken, is the most expensive thing of all.
Randy Harkins
February 16, 2026 AT 09:33Isolators are the future. 100 to 1,000x reduction in contamination? That’s not a win-that’s a revolution. And yes, they cost 40% more. But so did automated teller machines. So did smartphones. We don’t do things the hard way anymore. We do them the right way.
Real-time monitoring isn’t optional. It’s the new standard. And companies still clinging to weekly air samples? They’re not just behind-they’re dangerous.
Automation isn’t replacing people. It’s elevating them. From sterile gloved hands to sterile data analysts. That’s progress.
Karianne Jackson
February 16, 2026 AT 10:15Someone just died because a glove tore. That’s it. That’s the whole story.