Menstrual Pain Meds: Best Options, How They Work, and What to Avoid
When menstrual pain meds, medications used to reduce cramping and discomfort during periods. Also known as period pain relievers, they’re one of the most commonly used drugs by women worldwide. Most people reach for something over-the-counter the first time their cramps hit hard—but not all options are equal. Some work fast, others last longer, and a few can actually make things worse if you have certain health conditions. You don’t need to guess which one’s right for you. Let’s cut through the noise.
The two biggest categories of NSAIDs, nonsteroidal anti-inflammatory drugs that reduce inflammation and block pain signals. Also known as anti-inflammatories, they are the go-to for most. Ibuprofen and naproxen are the most studied and trusted. They don’t just mask pain—they lower the production of prostaglandins, the chemicals that make your uterus contract so hard it hurts. Studies show naproxen often lasts longer than ibuprofen, which means fewer pills during a long day. But if you’ve got stomach issues, kidney problems, or take blood thinners, these aren’t always safe. That’s where acetaminophen comes in—it’s gentler on the gut but doesn’t touch inflammation. It’s a trade-off: less risk, less power.
Then there’s the other side: hormonal treatment, birth control methods that regulate hormones to reduce menstrual intensity. Also known as oral contraceptives, they aren’t pain meds in the traditional sense, but they can stop the pain at its source. If your cramps are tied to heavy flow or hormonal spikes, combining birth control pills, patches, or IUDs with NSAIDs can cut pain by 50% or more. It’s not instant—takes a cycle or two to see results—but for many, it’s the only thing that makes periods bearable long-term. And yes, it’s still a medication. You need to talk to a provider about side effects like mood changes, weight shifts, or blood clot risks.
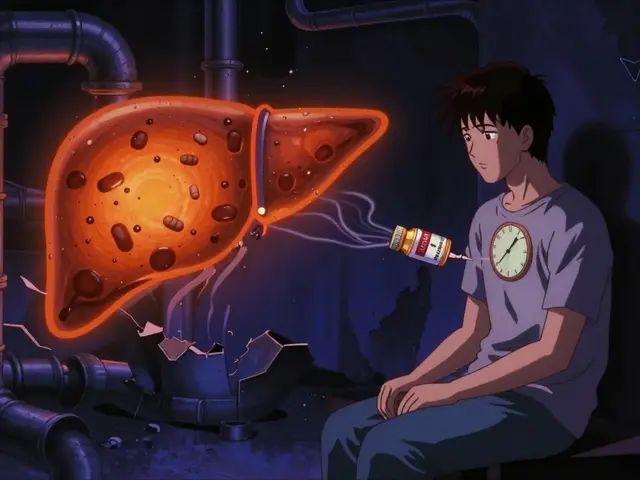
What about topical creams, patches, or herbal stuff? Some people swear by magnesium supplements or heating pads. They help, sure—but they’re support players, not starters. If your pain is bad enough to miss work or school, you need something stronger. And if you’ve tried everything and it’s still crushing you, that’s not normal. Endometriosis, fibroids, or adenomyosis can mimic bad cramps. No pill fixes those unless you get the right diagnosis.
This collection doesn’t just list pills. It shows you how delivery methods change how fast and how long relief lasts. It compares what works for one person versus another. It warns you about hidden risks in common meds and explains why some options are better for long-term use than others. You’ll find real comparisons—not marketing fluff—between NSAIDs, hormonal choices, and what to do when the basics don’t cut it. No fluff. No hype. Just what actually helps, what doesn’t, and what you need to ask your doctor before you buy another pack.
Compare Ponstel (Mefenamic Acid) with Alternatives for Pain Relief
By Lindsey Smith On 28 Oct, 2025 Comments (10)

Compare Ponstel (mefenamic acid) with ibuprofen, naproxen, paracetamol, and hormonal options for menstrual pain relief. Learn which works best, side effects, and safer alternatives.
View More