Relapse Risk: Understanding What Triggers Return of Symptoms and How to Prevent It
When symptoms come back after a period of improvement, it’s not bad luck—it’s usually a mismatch between treatment and biology. Relapse risk, the chance that a medical condition returns after improvement or remission. Also known as disease recurrence, it’s not just about forgetting to take pills—it’s about how your body reacts to stress, drugs, and changes in brain chemistry. Whether you’re managing depression after SSRIs, recovering from a stroke, or controlling gout with allopurinol, relapse risk is shaped by real, measurable factors—not guesswork.
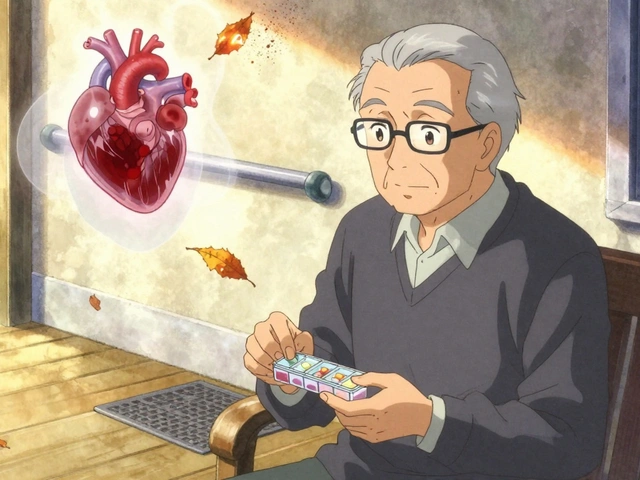
One big player in relapse risk is drug interactions, when two or more medications change how each other works in your body. For example, combining SSRIs with certain opioids like tramadol can trigger serotonin syndrome, a dangerous condition that pushes your system into overload. That kind of reaction doesn’t just cause new symptoms—it can undo months of progress. Then there’s medication adherence, how consistently you take your drugs as prescribed. Many people stop because of side effects, cost, or feeling better, but that’s often when relapse kicks in. Studies show that up to half of patients with chronic conditions miss doses, and that’s a major reason symptoms return. Even something as simple as drinking grapefruit juice while on statins can spike drug levels enough to cause muscle damage or liver stress, which might lead you to quit your meds altogether.
Recovery isn’t just about drugs. Your brain rewires itself after injury or illness—this is called neuroplasticity, the brain’s ability to form new neural connections to compensate for damage. After a stroke, rehab works because your brain learns new pathways. But if you stop therapy too soon, those new connections weaken. Relapse isn’t failure—it’s the brain reverting to old patterns when support fades. And then there’s adverse drug reactions, unexpected side effects that aren’t just annoying but can force you off treatment. Type A reactions are predictable and dose-related—like dizziness from blood pressure meds. Type B are rare but serious, like allergic reactions to antibiotics. Both can derail recovery if not monitored.
What you’ll find in these articles isn’t theory—it’s what actually happens in real lives. You’ll see how shunt surgery for normal pressure hydrocephalus can reverse dementia symptoms, why stopping blood thinners before cosmetic procedures can be riskier than keeping them, and how adjusting doses for aging kidneys prevents dangerous buildup. You’ll learn why phantom limb pain responds to mirror therapy, how febuxostat beats allopurinol for some gout patients, and why skipping doses on antidepressants can trigger a crash. These aren’t isolated cases—they’re patterns. And understanding them is the first step to beating relapse risk.
Medications for Alcohol Use Disorder and the Hidden Risk of Relapse
By Lindsey Smith On 20 Nov, 2025 Comments (15)

Medications for alcohol use disorder can reduce relapse risk - but only when used correctly. Learn how naltrexone, acamprosate, and disulfiram work, why they sometimes fail, and what actually helps people stay sober.
View More