Respiratory Pressure: Understanding the Basics and Clinical Uses
When talking about respiratory pressure, the application of controlled air or gas pressure to the airways to keep them open or to assist breathing. Also known as airway pressure therapy, it plays a crucial role in treating a range of pulmonary disorders, from obstructive sleep apnea to chronic obstructive pulmonary disease (COPD). This technology isn’t just a gadget; it’s a cornerstone of modern respiratory care that blends physics with patient‑centered treatment.
One core technique falls under the umbrella of positive airway pressure, a method that delivers air at a set pressure through a mask to prevent airway collapse, often called PAP therapy. The simplest form, continuous positive airway pressure, maintains a constant pressure throughout the breathing cycle (CPAP), is the go‑to for most sleep‑related breathing problems. When a single pressure isn’t enough, clinicians may switch to bi‑level positive airway pressure, which provides a higher pressure for inhalation and a lower pressure for exhalation (BiPAP). The shift from CPAP to BiPAP is often driven by patient comfort or the presence of additional conditions like heart failure.
These devices don’t work in a vacuum—they’re tightly linked to the condition they aim to treat. Sleep apnea is the most common driver behind PAP prescriptions, because its hallmark is repeated airway blockage during sleep. The severity of apnea determines whether a single‑level CPAP will suffice or a more adjustable BiPAP is needed. Beyond sleep disorders, PAP therapy also supports people with acute respiratory distress, helping to offload work of breathing and improve oxygenation.
In practice, setting the right pressure involves a careful titration process. Clinicians measure pressure in centimeters of water (cm H₂O) and adjust based on overnight monitoring, symptom relief, and patient feedback. Too low a pressure won’t keep the airway open; too high can cause discomfort, air leaks, or even barotrauma. Modern devices often include auto‑adjusting algorithms that sense flow and automatically fine‑tune pressure, embodying the triple relationship: respiratory pressure requires accurate measurement, enables airway patency, and influences sleep quality.
Key Concepts and Real‑World Applications
Respiratory pressure therapy isn’t limited to the bedroom. Pulmonary rehabilitation programs integrate PAP devices to boost exercise tolerance in COPD patients. The added pressure reduces dynamic hyperinflation, letting patients breathe more comfortably during physical activity. Similarly, during postoperative recovery, short‑term BiPAP can prevent atelectasis and accelerate lung re‑expansion, showcasing how pressure therapy supports faster healing.
Choosing the right device also depends on lifestyle factors. Mask style (nasal, full‑face, or nasal pillows), humidification, and portability influence adherence. Patients who travel frequently may opt for lightweight CPAP machines with battery packs, while those with complex needs might favor BiPAP units that allow separate inhale/out‑exhale settings. Understanding these trade‑offs helps clinicians tailor therapy, ensuring the technology works for the person, not the other way around.
Below you’ll find a curated set of articles that dive deeper into each aspect mentioned here. From practical guides on titrating pressure levels to comparisons of CPAP versus BiPAP, the collection covers the full spectrum of respiratory pressure therapy. Explore the posts to get actionable advice, detailed drug‑device interactions, and real‑world tips for making the most of your treatment plan.
How Sneezing Affects Your Voice and Vocal Cords
By Lindsey Smith On 19 Oct, 2025 Comments (9)
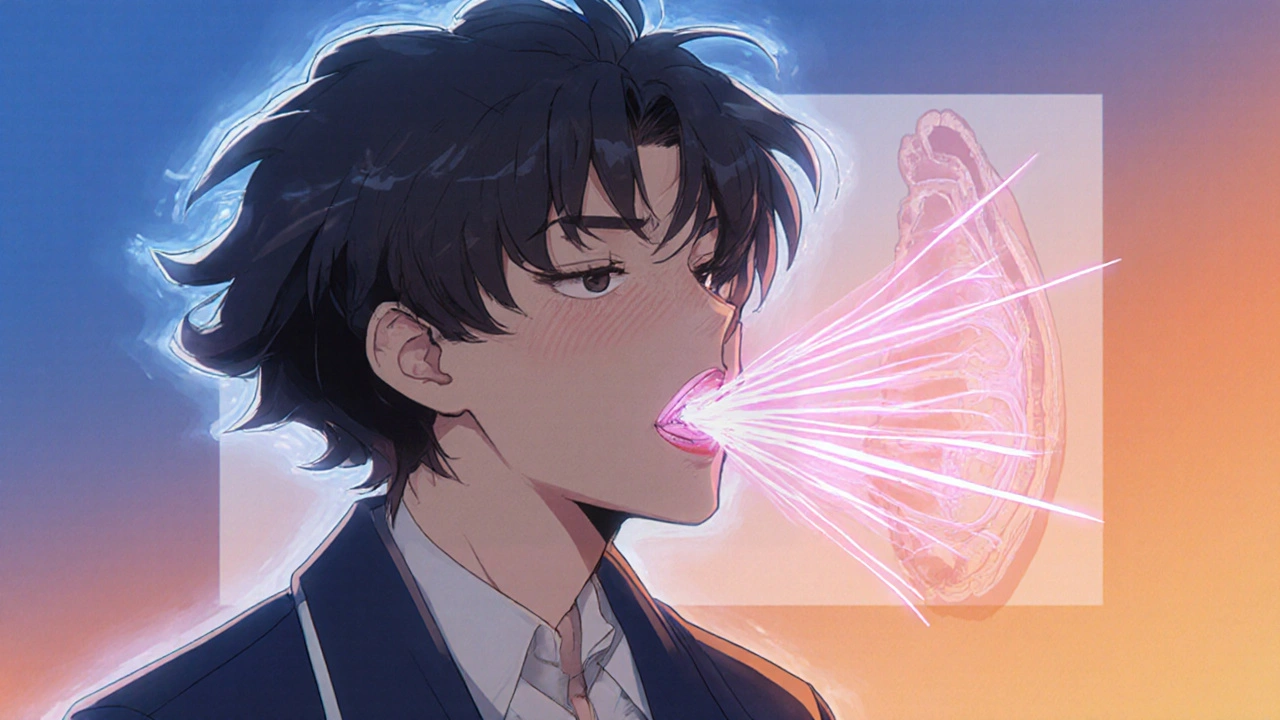
Discover how a sneeze affects your vocal cords, why you might sound hoarse, and simple steps to protect your voice during cold or allergy season.
View More