Beta-Blockers: What They Are, How They Work, and What You Need to Know
When your heart races too fast or your blood pressure stays too high, beta-blockers, a class of medications that block the effects of adrenaline on the heart and blood vessels. Also known as beta-adrenergic blocking agents, they’re one of the most commonly prescribed drugs for heart-related issues and are used by millions worldwide. They don’t cure conditions like high blood pressure or arrhythmias, but they help your body manage them—often with noticeable results in just days.
Beta-blockers work by attaching to beta receptors in your heart and blood vessels, stopping adrenaline from overstimulating them. This slows your heart rate, lowers blood pressure, and reduces the heart’s need for oxygen. That’s why they’re used after a heart attack—to give the heart time to heal. They’re also prescribed for migraines, tremors, and even performance anxiety, like stage fright or public speaking. Not all beta-blockers are the same. Some target only the heart (like metoprolol), while others affect blood vessels too (like carvedilol). The right one depends on your condition, age, and other meds you take.
They’re not without trade-offs. Common side effects include fatigue, cold hands, dizziness, and sometimes depression or trouble sleeping. People with asthma or severe diabetes need to be careful—beta-blockers can mask low blood sugar symptoms or tighten airways. And you can’t just stop taking them cold turkey; that can trigger a dangerous spike in heart rate or blood pressure. Your doctor will guide you on how to taper off safely.
What’s surprising is how widely they’re used beyond the heart. You’ll find them helping people with glaucoma (as eye drops), managing symptoms of hyperthyroidism, and even reducing the risk of recurrent heart attacks in young patients. They’re often paired with other meds like ACE inhibitors or diuretics for better control. And while newer drugs are emerging, beta-blockers remain a cornerstone because they’re affordable, well-studied, and work reliably for many.
There’s a lot of confusion around them. Some think they’re only for older adults with heart disease. Others believe they’re a cure-all for anxiety. The truth is more nuanced. Their effectiveness depends on the exact condition, dosage, and how your body responds. That’s why personalization matters—what works for one person might not work for another.
In the posts below, you’ll find real-world insights on how beta-blockers interact with alcohol, why they’re sometimes avoided in seniors, how they affect sleep and metabolism, and what alternatives exist when side effects become too much. You’ll also see how they fit into broader treatment plans—for heart failure, hypertension, and even conditions like phantom limb pain or migraine prevention. These aren’t theoretical guides. They’re based on clinical evidence, patient experiences, and updated guidelines. Whether you’re taking one now, considering it, or just trying to understand a loved one’s prescription, this collection gives you the facts you need to ask better questions and make smarter choices.
Psoriasis and Beta-Blockers: What You Need to Know About Skin Flare Risk
By Lindsey Smith On 7 Dec, 2025 Comments (15)
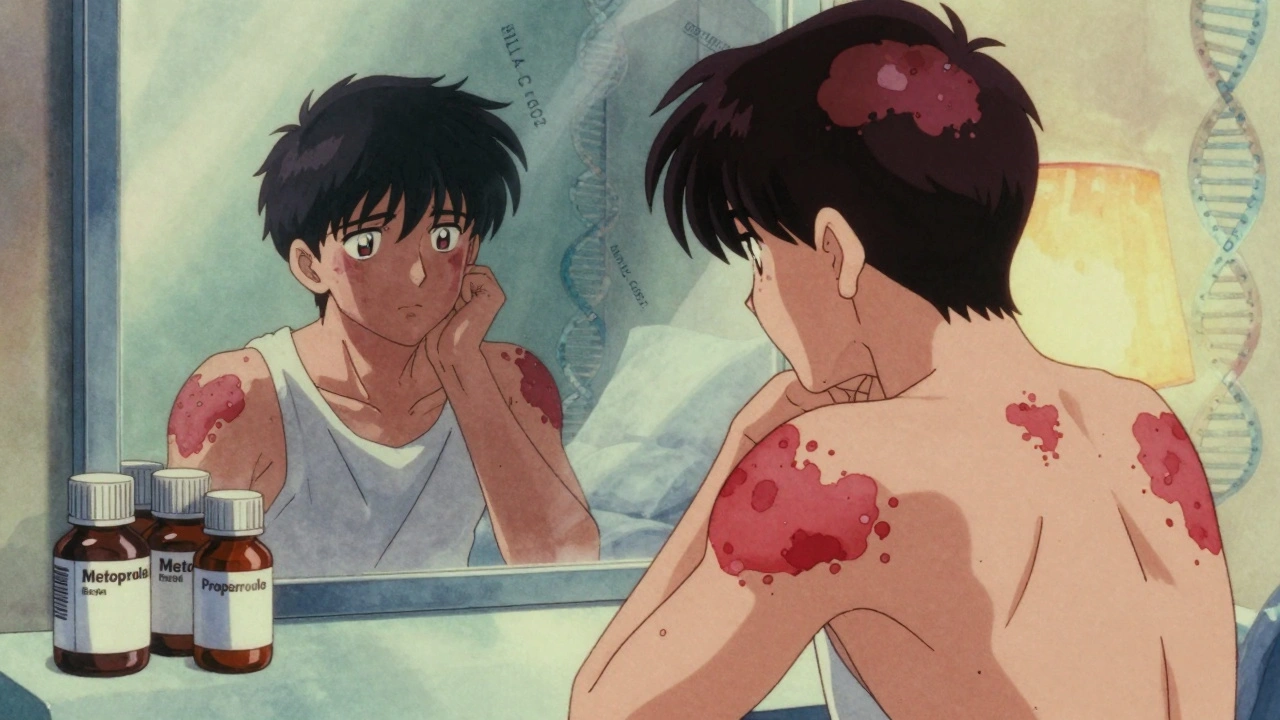
Beta-blockers can trigger or worsen psoriasis in up to 20% of users, with flares appearing months after starting the drug. Learn which medications carry the highest risk and what to do if your skin reacts.
View More