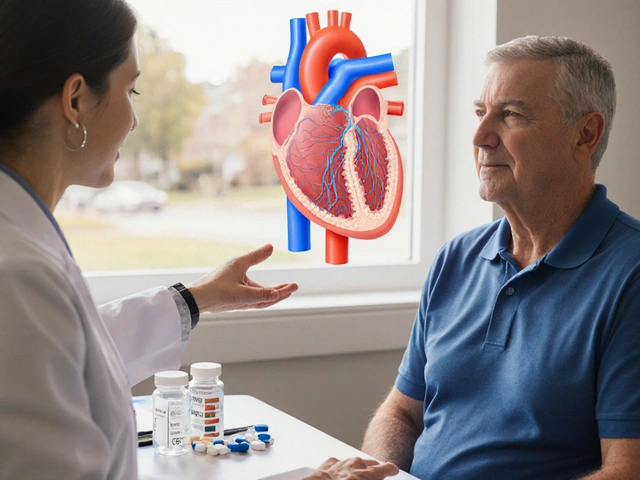
Medication Trigger: What Causes Unexpected Reactions and How to Avoid Them
When a medication trigger, a specific factor that causes an unexpected or harmful response to a drug. Also known as a drug-induced reaction, it can turn a safe treatment into a life-threatening event. It’s not always about dosage or allergies—it’s often about what else you’re taking, eating, or even your body’s changing ability to process drugs as you age. A simple combo like grapefruit juice and a statin, or Rhodiola with an SSRI, can push your system past its limit. These aren’t rare mistakes—they happen every day because the risks aren’t clear until something goes wrong.
One major adverse drug reaction, a harmful and unintended response to a medication at normal doses. Also known as ADR, it falls into two clear types: Type A, which is predictable and tied to the drug’s known effects—like bleeding from blood thinners or liver enzyme spikes from statins—and Type B, which is rare, unpredictable, and often allergic or immune-driven. The serotonin syndrome, a dangerous condition caused by too much serotonin in the brain, often from drug combinations. Also known as serotonin toxicity, it is a classic Type B reaction that can sneak up when you mix antidepressants with certain supplements or opioids. It’s not just about taking two drugs—it’s about how your body changes over time. Seniors, for example, process meds slower because their kidneys and liver aren’t what they used to be. That’s why a dose that was fine at 50 can become risky at 75.
What you eat, what you take, and even how you take it can be a medication trigger. Grapefruit juice doesn’t just affect statins—it messes with dozens of drugs by blocking enzymes that break them down. Naloxone saves lives from opioid overdoses, but if you don’t know how to use it or where to get it, that lifesaving tool is useless. Digital pill sensors help track adherence, but they won’t fix a trigger if you’re still mixing alcohol with sedatives or skipping doses because of cost. The real problem isn’t the drugs themselves—it’s the lack of clear, practical guidance about how they interact with your life.
Below, you’ll find real-world stories and science-backed facts about what makes medications go wrong—and how to keep them from harming you. From how anticoagulants affect bruising after cosmetic procedures, to why stopping blood thinners can be more dangerous than keeping them, these posts cut through the noise. You’ll learn how to spot early signs of serotonin syndrome, why biosimilars save money without risking safety, and how aging changes your body’s response to every pill you take. No fluff. No guesswork. Just what you need to stay safe.
Psoriasis and Beta-Blockers: What You Need to Know About Skin Flare Risk
By Lindsey Smith On 7 Dec, 2025 Comments (15)
Beta-blockers can trigger or worsen psoriasis in up to 20% of users, with flares appearing months after starting the drug. Learn which medications carry the highest risk and what to do if your skin reacts.
View More