Tramadol SSRI Risk: What You Need to Know About Dangerous Drug Interactions
When you take tramadol, a painkiller that also affects serotonin in the brain. Also known as Ultram, it's often prescribed for moderate to severe pain, but it doesn't play well with others—especially SSRIs, a class of antidepressants that boost serotonin levels. Also known as selective serotonin reuptake inhibitors, they include drugs like sertraline, fluoxetine, and citalopram. Mixing these two can push your serotonin levels too high, leading to a dangerous condition called serotonin syndrome, a life-threatening reaction caused by too much serotonin in the nervous system. This isn't a rare edge case—it's a well-documented risk that shows up in ERs every week.
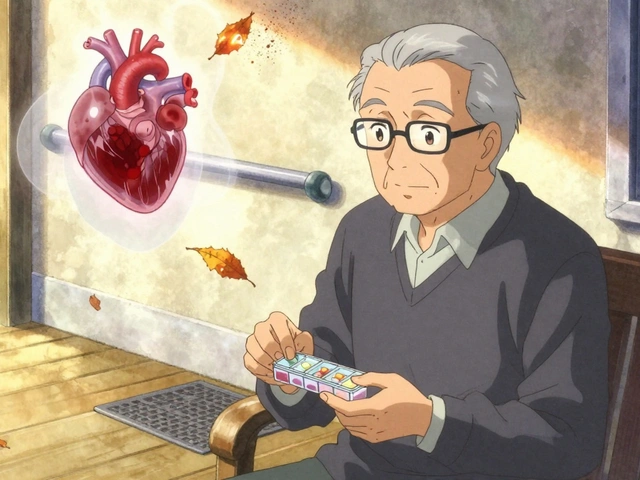
Tramadol works in two ways: it binds to opioid receptors like traditional painkillers, but it also blocks serotonin reuptake—just like SSRIs do. When you add an SSRI on top, your body can't clear the extra serotonin fast enough. Symptoms start mild: shivering, sweating, restlessness. But they can escalate fast—muscle rigidity, high fever, seizures, irregular heartbeat. If you're on both meds and feel suddenly unwell, don't wait. Call your doctor or go to the ER. Many people don’t realize the danger because they assume all prescriptions are safe together. They’re not. The FDA has issued warnings, and multiple studies confirm this interaction isn’t theoretical—it’s deadly serious. Even low doses of tramadol can trigger this when paired with SSRIs, especially in older adults or those with kidney issues, where drugs build up in the system.
You might be wondering: "What if I’ve been on both for months and feel fine?" That doesn’t mean you’re safe. Serotonin syndrome can hit suddenly, even after years of stable use. Changes in dosage, new supplements like St. John’s wort, or even a cold medicine with dextromethorphan can push you over the edge. Your pharmacist or doctor should be reviewing every new prescription you get—but they can’t catch everything if you don’t tell them everything you’re taking. Keep a list: pills, patches, herbal teas, even over-the-counter stuff. If you’re on an SSRI and your doctor prescribes tramadol, ask: "Is there a safer painkiller?" Alternatives like acetaminophen or low-dose NSAIDs often work just as well without the risk. And if you’re switching from one antidepressant to another, never stop or start meds without a clear plan. This isn’t about fear—it’s about awareness. The posts below cover real cases, doctor guidelines, and safer alternatives so you can make smart choices without guessing.
SSRIs and Opioids: Understanding Serotonin Syndrome Risk and How to Prevent It
By Lindsey Smith On 16 Nov, 2025 Comments (13)

Combining SSRIs and opioids can cause serotonin syndrome-a dangerous, sometimes fatal condition. Learn which opioid-SSRI pairs are risky, how to spot early symptoms, and what safer alternatives exist.
View More