Overdose Rescue: What Works, What Doesn’t, and How to Act Fast
When someone overdoses, every second counts. Overdose rescue, the immediate actions taken to reverse or manage a life-threatening drug reaction. Also known as drug overdose response, it’s not just about calling 911—it’s about knowing what to do while you wait. Whether it’s opioids, benzodiazepines, or even mixing prescription meds with alcohol, the body can shut down fast. And too often, people wait too long because they’re scared, confused, or don’t recognize the signs.
One of the most powerful tools in naloxone, a medication that rapidly reverses opioid overdoses by blocking opioid receptors in the brain. Also known as Narcan, it’s safe, easy to use, and works even if you’re not sure what drug was taken. It doesn’t work on stimulants like cocaine or meth, but if someone is unresponsive, has slow or shallow breathing, or their lips are blue, naloxone is the first line of defense. You can get it without a prescription in most states, and many pharmacies hand it out for free. Keep it in your bag, your car, your home. It’s not just for people who use drugs—it’s for friends, family, neighbors.
But naloxone isn’t a magic fix. After giving it, you still need to stay with the person. The effects of naloxone wear off in 30 to 90 minutes, and if the opioid is still in their system, they can slip back into overdose. That’s why calling 911 is non-negotiable—even if they wake up. Emergency responders can monitor them, give more naloxone if needed, and connect them to care. And if you’re ever unsure whether someone is overdosing, err on the side of caution. A person who’s not breathing normally is in danger, no matter what they took.
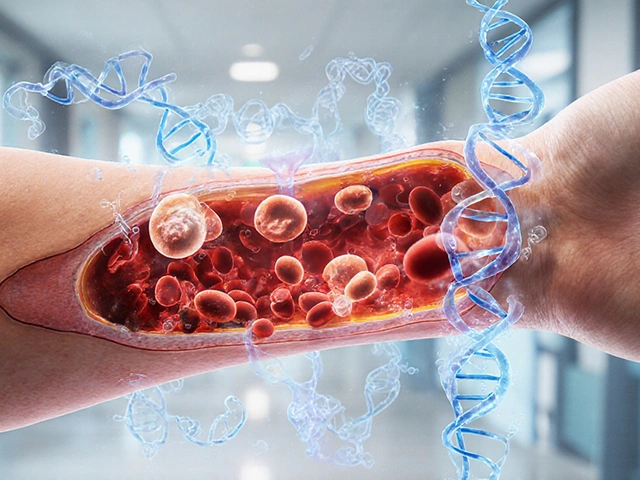
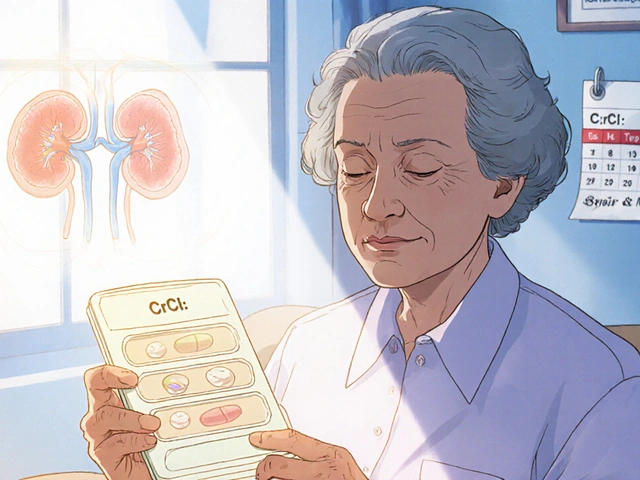
Overdose rescue also means understanding what puts people at risk. Mixing opioids with alcohol or benzodiazepines is one of the deadliest combinations. So is using after a period of abstinence—your tolerance drops, and the same dose you used before can now kill you. That’s why so many overdoses happen after rehab, after jail, or after a break from use. It’s not about willpower. It’s about biology.
You’ll find real stories here—not theory, not lectures—just clear, practical advice from people who’ve been there. Posts cover how to recognize early signs of overdose, how to use naloxone correctly, what to say to emergency dispatchers, and why some medications like tramadol or fentanyl are especially dangerous. You’ll also see how digital pill sensors and medication adherence tools are helping prevent overdoses before they happen. And you’ll learn why stopping certain drugs cold turkey can be riskier than staying on them under supervision.
This isn’t about judgment. It’s about survival. Whether you’re a caregiver, a friend, a patient, or just someone who wants to be ready, the tools to save a life are simpler than you think. And they’re within reach.
How to Use Naloxone Nasal Spray for Opioid Overdose: Step-by-Step Guide
By Lindsey Smith On 27 Nov, 2025 Comments (15)

Learn how to use naloxone nasal spray to reverse an opioid overdose in 9 simple steps. Includes signs of overdose, dosing tips for fentanyl, what to do after giving naloxone, and where to get it without a prescription.
View More